
Spinal disc herniation
Encyclopedia
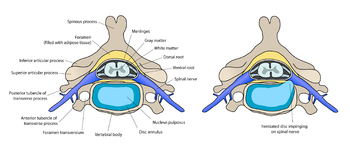
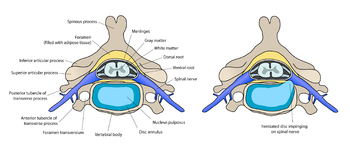
A spinal disc herniation (prolapsus disci intervertebralis), informally and misleadingly called a "slipped disc", is a medical condition affecting the spine
due to trauma
, lifting injuries, or idiopathic
, in which a tear in the outer, fibrous ring (annulus fibrosus
) of an intervertebral disc
(discus intervertebralis) allows the soft, central portion (nucleus pulposus
) to bulge out
. Tears are almost always postero-lateral in nature owing to the presence of the posterior longitudinal ligament
in the spinal canal. This tear in the disc ring may result in the release of inflammatory chemical mediators which may directly cause severe pain, even in the absence of nerve root compression (see pathophysiology below). This is the rationale for the use of anti-inflammatory treatments for pain associated with disc herniation, protrusion, bulge, or disc tear.
It is normally a further development of a previously existing disc protrusion, a condition in which the outermost layers of the annulus fibrosus are still intact, but can bulge when the disc is under pressure.
 Most English language publications use the spelling disc more often than disk. Nomina Anatomica
Most English language publications use the spelling disc more often than disk. Nomina Anatomica
designates the structures as disci intervertebrales [plural form] and Terminologia Anatomica
as discus intervertebralis/intervertebral disc
, [singular form].
Some of the terms commonly used to describe the condition include herniated disc, prolapsed disc, ruptured disc and the misleading expression slipped disc. Other terms that are closely related include disc protrusion, bulging disc, pinched nerve, sciatica
, disc disease, disc degeneration, degenerative disc disease
, and black disc.
The popular term slipped disc is misleading, as an intervertebral disc, being tightly sandwiched between two vertebrae to which the disc is attached, cannot actually "slip", "slide", or even get "out of place". The disc is actually grown together with the adjacent vertebrae and can be squeezed, stretched and twisted, all in small degrees. It can also be torn, ripped, herniated, and degenerated, but it cannot "slip". "The term 'slipped disc' may be harmful as it leads to a false idea of what is happening and therefore of the likely outcome." However, one vertebral body can slip relative to an adjacent vertebral body. This is called spondylolisthesis
and can damage the disc between the two vertebrae.
that will radiate into the regions served by affected nerve roots that are irritated or impinged by the herniated material. Often, herniated discs are not diagnosed immediately, as the patients come with undefined pains in the thighs, knees, or feet. Other symptoms may include sensory changes such as numbness, tingling, muscular weakness, paralysis, paresthesia
, and affection of reflexes. If the herniated disc is in the lumbar region the patient may also experience sciatica
due to irritation of one of the nerve roots of the sciatic nerve
. Unlike a pulsating pain or pain that comes and goes, which can be caused by muscle spasm, pain from a herniated disc is usually continuous or at least is continuous in a specific position of the body.
It is possible to have a herniated disc without any pain or noticeable symptoms, depending on its location. If the extruded nucleus pulposus material doesn't press on soft tissues or nerves, it may not cause any symptoms. A small-sample study examining the cervical spine in symptom-free volunteers has found focal disc protrusions in 50% of participants, which shows that a considerable part of the population can have focal herniated discs in their cervical region that do not cause noticeable symptoms.
Typically, symptoms are experienced only on one side of the body. If the prolapse is very large and presses on the spinal cord or the cauda equina
in the lumbar region, affection of both sides of the body may occur, often with serious consequences. Compression of the cauda equina can cause permanent nerve damage or paralysis. The nerve damage can result in loss of bowel and bladder control as well as sexual dysfunction. See Cauda equina syndrome
.
Minor back pain and chronic back tiredness are indicators of general wear and tear that make one susceptible to herniation on the occurrence of a traumatic event, such as bending to pick up a pencil or falling. When the spine is straight, such as in standing or lying down, internal pressure is equalized on all parts of the discs. While sitting or bending to lift, internal pressure on a disc can move from 17 psi
(lying down) to over 300 psi (lifting with a rounded back).
Herniation of the contents of the disc into the spinal canal often occurs when the anterior side (stomach side) of the disc is compressed while sitting or bending forward, and the contents (nucleus pulposus) get pressed against the tightly stretched and thinned membrane (annulus fibrosis) on the posterior side (back side) of the disc. The combination of membrane thinning from stretching and increased internal pressure (200 to 300 psi) results in the rupture of the confining membrane. The jelly-like contents of the disc then move into the spinal canal, pressing against the spinal nerves, thus producing intense and usually disabling pain and other symptoms.
There is also a strong genetic component. Mutation in genes coding for proteins involved in the regulation of the extracellular matrix, such as MMP2
and THBS2
, has been demonstrated to contribute to lumbar disc herniation.
The majority of spinal disc herniation cases occur in lumbar region (95% in L4-L5 or L5-S1). The second most common site is the cervical region
(C5-C6, C6-C7). Thoracic region accounts for only 0.15% to 4.0% of cases.
and brachial plexus
can be affected.
disc herniations occur in the lower back, most often between the fourth and fifth lumbar vertebral bodies or between the fifth and the sacrum
. Symptoms can affect the lower back, buttocks
, thigh
, anal/genital region
(via the Perineal nerve
), and may radiate into the foot and/or toe
. The sciatic nerve
is the most commonly affected nerve, causing symptoms of sciatica
. The femoral nerve
can also be affected and cause the patient to experience a numb, tingling feeling throughout one or both legs and even feet or even a burning feeling in the hips and legs.
. A primary focus of surgery is to remove “pressure” or reduce mechanical compression on a neural element: either the spinal cord
, or a nerve root
. But it is increasingly recognized that back pain, rather than being solely due to compression, may also be due to chemical inflammation. There is evidence that points to a specific inflammatory mediator of this pain. This inflammatory molecule, called tumor necrosis factor-alpha (TNF), is released not only by the herniated disc, but also in cases of disc tear (annular tear), by facet joints, and in spinal stenosis
. In addition to causing pain and inflammation, TNF
may also contribute to disc degeneration.
. At some point in the evaluation, tests may be performed to confirm or rule out other causes of symptoms such as spondylolisthesis
, degeneration, tumor
s, metastases and space-occupying lesion
s, as well as to evaluate the efficacy of potential treatment options.
may be positive, as this finding has low specificity; however, it has high sensitivity. Thus the finding of a negative SLR sign is an important in helping to "rule out" the possibility of a lower lumbar disc herniation. A variation is to lift the leg while the patient is sitting. However, this reduces the sensitivity of the test.
, which can be caused by spinal disc herniation, found that "After 12 weeks, 73% of patients showed reasonable to major improvement without surgery." The study, however, did not determine the number of individuals in the group that had sciatica caused by disc herniation.
If pain due to disc herniation, protrusion, bulge, or disc tear is due to chemical radiculitis pain, then prior to surgery it may make sense to try an anti-inflammatory approach. Often this is first attempted with non-steroidal anti-inflammatory medications (NSAIDs), but the long-term use of NSAIDs for patients with persistent back pain is complicated by their possible cardiovascular and gastrointestinal toxicity; and NSAIDs have limited value to intervene in tumor necrosis factor-alpha (TNF)-mediated processes. An alternative often employed is the injection of cortisone
into the spine adjacent to the suspected pain generator, a technique known as “epidural steroid injection”. Although this technique began more than a decade ago for pain due to disc herniation, the efficacy of epidural steroid injections is now generally thought to be limited to short term pain relief in selected patients only. In addition, epidural steroid injections, in certain settings, may result in serious complications. Fortunately there are now emerging new methods that directly target TNF. These TNF-targeted methods represent a highly promising new approach for patients with chronic severe spinal pain, such as those with failed back surgery syndrome. Ancillary approaches, such as rehabilitation, physical therapy
, anti-depressants, and, in particular, graduated exercise programs, may all be useful adjuncts to anti-inflammatory approaches.
, contraindicated
, relatively contraindicated, or inconclusive based on the safety profile of their risk-benefit ratio
and on whether they may or may not help:
(in which there is incontinence, weakness and genital numbness) is considered a medical emergency requiring immediate attention and possibly surgical decompression.
Any claim of absolute contraindications for lumbar disc disease would invariably be challenged. Most spine surgeons adhere to some guidelines, including the following:
• A patient with unrelenting back pain: Patients who have back pain after a bout of sciatica has resolved are not good candidates for operative treatment. Often, these patients are the most insistent and difficult to manage. Occasionally, these are patients whose back pain improved after discectomy for a large central disc herniation.
• A patient with an incomplete workup: When diagnosis is uncertain, postpone surgery. Disc herniations are so ubiquitous that being cavalier in diagnosis is easy. Ensure the completeness of the workup prior to proceeding with the operation. All surgeons can recall several cases in which a diabetic plexopathy or an epidural metastasis was missed.
• A patient not provided adequate conservative treatment: Spine surgeons rarely commit a patient with a short period of sciatica and without bedrest and a steroid trial to an operation that will permanently alter the patient's back mechanics and strength.
Regarding the role of surgery for failed medical therapy in patients without a significant neurological deficit, a meta-analysis
of randomized controlled trials by the Cochrane Collaboration
concluded that "limited evidence is now available to support some aspects of surgical practice". More recent randomized controlled trials refine indications for surgery as follows:
Surgical goals include relief of nerve compression, allowing the nerve to recover, as well as the relief of associated back pain and restoration of normal function.
 Disc herniation can occur in any disc in the spine, but the two most common forms are lumbar disc herniation and cervical disc herniation. The former is the most common, causing lower back pain (lumbago) and often leg pain as well, in which case it is commonly referred to as sciatica
Disc herniation can occur in any disc in the spine, but the two most common forms are lumbar disc herniation and cervical disc herniation. The former is the most common, causing lower back pain (lumbago) and often leg pain as well, in which case it is commonly referred to as sciatica
.
Lumbar disc herniation occurs 15 times more often than cervical (neck) disc herniation, and it is one of the most common causes of lower back pain. The cervical discs are affected 8% of the time and the upper-to-mid-back (thoracic) discs only 1 - 2% of the time.
The following locations have no discs and are therefore exempt from the risk of disc herniation: the upper two cervical intervertebral spaces, the sacrum
, and the coccyx
.
Most disc herniations occur when a person is in their thirties or forties when the nucleus pulposus is still a gelatin-like substance. With age the nucleus pulposus changes ("dries out") and the risk of herniation is greatly reduced. After age 50 or 60, osteoarthritic
degeneration (spondylosis) or spinal stenosis
are more likely causes of low back pain
or leg pain.
became available in the U.S. in 1998, and were demonstrated to be potentially effective for treating sciatica
in experimental models beginning in 2001. Targeted anatomic administration of one of these anti-TNF agents, etanercept
, a patented treatment method, has been suggested in published pilot studies to be effective for treating selected patients with severe pain due to disc herniation, protrusion, bulge, or disc tear. The scientific basis for pain relief in these patients is supported by the most current review articles. In the future new imaging methods may allow non-invasive identification of sites of neuronal inflammation, thereby enabling more accurate localization of the "pain generators" responsible for symptom production.
Future treatments may include stem cell therapy. Doctors Victor Y. L. Leung, Danny Chan and Kenneth M. C. Cheung have reported in the European Spine Journal that "substantial progress has been made in the field of stem cell regeneration of the intervertebral disc. Autogenic mesenchymal stem cells in animal models can arrest intervertebral disc degeneration or even partially regenerate it and the effect is suggested to be dependent on the severity of the degeneration."
Vertebral column
In human anatomy, the vertebral column is a column usually consisting of 24 articulating vertebrae, and 9 fused vertebrae in the sacrum and the coccyx. It is situated in the dorsal aspect of the torso, separated by intervertebral discs...
due to trauma
Trauma (medicine)
Trauma refers to "a body wound or shock produced by sudden physical injury, as from violence or accident." It can also be described as "a physical wound or injury, such as a fracture or blow." Major trauma can result in secondary complications such as circulatory shock, respiratory failure and death...
, lifting injuries, or idiopathic
Idiopathic
Idiopathic is an adjective used primarily in medicine meaning arising spontaneously or from an obscure or unknown cause. From Greek ἴδιος, idios + πάθος, pathos , it means approximately "a disease of its own kind". It is technically a term from nosology, the classification of disease...
, in which a tear in the outer, fibrous ring (annulus fibrosus
Annulus fibrosus disci intervertebralis
Each intervertebral fibrocartilage is composed, at its circumference, of laminæ of fibrous tissue and fibrocartilage, forming the annulus fibrosus.-Spelling notes:...
) of an intervertebral disc
Intervertebral disc
Intervertebral discs lie between adjacent vertebrae in the spine. Each disc forms a cartilaginous joint to allow slight movement of the vertebrae, and acts as a ligament to hold the vertebrae together.-Structure:...
(discus intervertebralis) allows the soft, central portion (nucleus pulposus
Nucleus pulposus
Nucleus pulposus is the jelly-like substance in the middle of the spinal disc. It is the remnant of the notochord . It functions to distribute hydraulic pressure in all directions within each disc under compressive loads. The nucleus pulposus consists of chondrocyte-like cells, collagen fibrils,...
) to bulge out
Hernia
A hernia is the protrusion of an organ or the fascia of an organ through the wall of the cavity that normally contains it. A hiatal hernia occurs when the stomach protrudes into the mediastinum through the esophageal opening in the diaphragm....
. Tears are almost always postero-lateral in nature owing to the presence of the posterior longitudinal ligament
Posterior longitudinal ligament
The posterior longitudinal ligament is situated within the vertebral canal, and extends along the posterior surfaces of the bodies of the vertebræ, from the body of the axis, where it is continuous with the membrana tectoria, to the sacrum....
in the spinal canal. This tear in the disc ring may result in the release of inflammatory chemical mediators which may directly cause severe pain, even in the absence of nerve root compression (see pathophysiology below). This is the rationale for the use of anti-inflammatory treatments for pain associated with disc herniation, protrusion, bulge, or disc tear.
It is normally a further development of a previously existing disc protrusion, a condition in which the outermost layers of the annulus fibrosus are still intact, but can bulge when the disc is under pressure.
Terminology
Nomina Anatomica
In the late nineteenth century some 50,000 terms for various body parts were in use. The same structures were described by different names, depending on the anatomist’s school and national tradition. Vernacular translations of Latin and Greek, as well as various eponymous terms, were barriers to...
designates the structures as disci intervertebrales [plural form] and Terminologia Anatomica
Terminologia Anatomica
Terminologia Anatomica is the international standard on human anatomic terminology. It was developed by the Federative Committee on Anatomical Terminology and the International Federation of Associations of Anatomists and was released in 1998. It supersedes the previous standard, Nomina...
as discus intervertebralis/intervertebral disc
Intervertebral disc
Intervertebral discs lie between adjacent vertebrae in the spine. Each disc forms a cartilaginous joint to allow slight movement of the vertebrae, and acts as a ligament to hold the vertebrae together.-Structure:...
, [singular form].
Some of the terms commonly used to describe the condition include herniated disc, prolapsed disc, ruptured disc and the misleading expression slipped disc. Other terms that are closely related include disc protrusion, bulging disc, pinched nerve, sciatica
Sciatica
Sciatica is a set of symptoms including pain that may be caused by general compression or irritation of one of five spinal nerve roots that give rise to each sciatic nerve, or by compression or irritation of the left or right or both sciatic nerves. The pain is felt in the lower back, buttock, or...
, disc disease, disc degeneration, degenerative disc disease
Degenerative disc disease
Degeneration of the intervertebral disc, often called "degenerative disc disease" of the spine, is a condition that can be painful and can greatly affect the quality of one's life...
, and black disc.
The popular term slipped disc is misleading, as an intervertebral disc, being tightly sandwiched between two vertebrae to which the disc is attached, cannot actually "slip", "slide", or even get "out of place". The disc is actually grown together with the adjacent vertebrae and can be squeezed, stretched and twisted, all in small degrees. It can also be torn, ripped, herniated, and degenerated, but it cannot "slip". "The term 'slipped disc' may be harmful as it leads to a false idea of what is happening and therefore of the likely outcome." However, one vertebral body can slip relative to an adjacent vertebral body. This is called spondylolisthesis
Spondylolisthesis
Spondylolisthesis describes the anterior or posterior displacement of a vertebra or the vertebral column in relation to the vertebrae below. It was first described in 1782 by Belgian obstetrician, Dr. Herbinaux. He reported a bony prominence anterior to the sacrum that obstructed the vagina of a...
and can damage the disc between the two vertebrae.
Signs and symptoms
Symptoms of a herniated disc can vary depending on the location of the herniation and the types of soft tissue that become involved. They can range from little or no pain if the disc is the only tissue injured, to severe and unrelenting neck or low back painLow back pain
Low back pain or lumbago is a common musculoskeletal disorder affecting 80% of people at some point in their lives. In the United States it is the most common cause of job-related disability, a leading contributor to missed work, and the second most common neurological ailment — only headache is...
that will radiate into the regions served by affected nerve roots that are irritated or impinged by the herniated material. Often, herniated discs are not diagnosed immediately, as the patients come with undefined pains in the thighs, knees, or feet. Other symptoms may include sensory changes such as numbness, tingling, muscular weakness, paralysis, paresthesia
Paresthesia
Paresthesia , spelled "paraesthesia" in British English, is a sensation of tingling, burning, pricking, or numbness of a person's skin with no apparent long-term physical effect. It is more generally known as the feeling of "pins and needles" or of a limb "falling asleep"...
, and affection of reflexes. If the herniated disc is in the lumbar region the patient may also experience sciatica
Sciatica
Sciatica is a set of symptoms including pain that may be caused by general compression or irritation of one of five spinal nerve roots that give rise to each sciatic nerve, or by compression or irritation of the left or right or both sciatic nerves. The pain is felt in the lower back, buttock, or...
due to irritation of one of the nerve roots of the sciatic nerve
Sciatic nerve
The sciatic nerve is a large nerve fiber in humans and other animals. It begins in the lower back and runs through the buttock and down the lower limb...
. Unlike a pulsating pain or pain that comes and goes, which can be caused by muscle spasm, pain from a herniated disc is usually continuous or at least is continuous in a specific position of the body.
It is possible to have a herniated disc without any pain or noticeable symptoms, depending on its location. If the extruded nucleus pulposus material doesn't press on soft tissues or nerves, it may not cause any symptoms. A small-sample study examining the cervical spine in symptom-free volunteers has found focal disc protrusions in 50% of participants, which shows that a considerable part of the population can have focal herniated discs in their cervical region that do not cause noticeable symptoms.
Typically, symptoms are experienced only on one side of the body. If the prolapse is very large and presses on the spinal cord or the cauda equina
Cauda equina
The cauda equina is a structure within the lower end of the spinal column of most vertebrates, that consists of nerve roots and rootlets from above...
in the lumbar region, affection of both sides of the body may occur, often with serious consequences. Compression of the cauda equina can cause permanent nerve damage or paralysis. The nerve damage can result in loss of bowel and bladder control as well as sexual dysfunction. See Cauda equina syndrome
Cauda equina syndrome
Cauda equina syndrome ' is a serious neurologic condition in which there is acute loss of function of the lumbar plexus, neurologic elements of the spinal canal below the termination of the spinal cord.-Causes:...
.
Cause
Disc herniations can result from general wear and tear, such as when performing jobs that require constant sitting. However, herniations often result from jobs that require lifting. Traumatic (quick) injury to lumbar discs commonly occurs when lifting while bent at the waist, rather than lifting with the legs while the back is straight.Minor back pain and chronic back tiredness are indicators of general wear and tear that make one susceptible to herniation on the occurrence of a traumatic event, such as bending to pick up a pencil or falling. When the spine is straight, such as in standing or lying down, internal pressure is equalized on all parts of the discs. While sitting or bending to lift, internal pressure on a disc can move from 17 psi
Pounds per square inch
The pound per square inch or, more accurately, pound-force per square inch is a unit of pressure or of stress based on avoirdupois units...
(lying down) to over 300 psi (lifting with a rounded back).
Herniation of the contents of the disc into the spinal canal often occurs when the anterior side (stomach side) of the disc is compressed while sitting or bending forward, and the contents (nucleus pulposus) get pressed against the tightly stretched and thinned membrane (annulus fibrosis) on the posterior side (back side) of the disc. The combination of membrane thinning from stretching and increased internal pressure (200 to 300 psi) results in the rupture of the confining membrane. The jelly-like contents of the disc then move into the spinal canal, pressing against the spinal nerves, thus producing intense and usually disabling pain and other symptoms.
There is also a strong genetic component. Mutation in genes coding for proteins involved in the regulation of the extracellular matrix, such as MMP2
MMP2
72 kDa type IV collagenase also known as matrix metalloproteinase-2 and gelatinase A is an enzyme that in humans is encoded by the MMP2 gene....
and THBS2
THBS2
Thrombospondin-2 is a protein that in humans is encoded by the THBS2 gene.-Further reading:...
, has been demonstrated to contribute to lumbar disc herniation.
The majority of spinal disc herniation cases occur in lumbar region (95% in L4-L5 or L5-S1). The second most common site is the cervical region
Cervical vertebrae
In vertebrates, cervical vertebrae are those vertebrae immediately inferior to the skull.Thoracic vertebrae in all mammalian species are defined as those vertebrae that also carry a pair of ribs, and lie caudal to the cervical vertebrae. Further caudally follow the lumbar vertebrae, which also...
(C5-C6, C6-C7). Thoracic region accounts for only 0.15% to 4.0% of cases.
Cervical
Cervical disc herniations occur in the neck, most often between the fifth & sixth (C5/6) and the sixth and seventh (C6/7) cervical vertebral bodies. Symptoms can affect the back of the skull, the neck, shoulder girdle, scapula, shoulder, arm, and hand. The nerves of the cervical plexusCervical plexus
The cervical plexus is a plexus of the ventral rami of the first four cervical spinal nerves which are located from C1 to C4 cervical segment in the neck. They are located laterally to the transverse processes between prevertebral muscles from the medial side and vertebral from lateral side...
and brachial plexus
Brachial plexus
The brachial plexus is a network of nerve fibers, running from the spine, formed by the ventral rami of the lower four cervical and first thoracic nerve roots...
can be affected.
Thoracic
Thoracic discs are very stable and herniations in this region are quite rare. Herniation of the uppermost thoracic discs can mimic cervical disc herniations, while herniation of the other discs can mimic lumbar herniations.Lumbar
LumbarLumbar
In tetrapod anatomy, lumbar is an adjective that means of or pertaining to the abdominal segment of the torso, between the diaphragm and the sacrum ...
disc herniations occur in the lower back, most often between the fourth and fifth lumbar vertebral bodies or between the fifth and the sacrum
Sacrum
In vertebrate anatomy the sacrum is a large, triangular bone at the base of the spine and at the upper and back part of the pelvic cavity, where it is inserted like a wedge between the two hip bones. Its upper part connects with the last lumbar vertebra, and bottom part with the coccyx...
. Symptoms can affect the lower back, buttocks
Buttocks
The buttocks are two rounded portions of the anatomy, located on the posterior of the pelvic region of apes and humans, and many other bipeds or quadrupeds, and comprise a layer of fat superimposed on the gluteus maximus and gluteus medius muscles. Physiologically, the buttocks enable weight to...
, thigh
Thigh
In humans the thigh is the area between the pelvis and the knee. Anatomically, it is part of the lower limb.The single bone in the thigh is called the femur...
, anal/genital region
Perineum
In human anatomy, the perineum is a region of the body including the perineal body and surrounding structures...
(via the Perineal nerve
Perineal nerve
The perineal nerve is a nerve arising from the pudendal nerve that supplies the perineum.-Structure:The perineal nerve is the inferior and larger of the two terminal branches of the pudendal nerve, is situated below the internal pudendal artery....
), and may radiate into the foot and/or toe
Toe
Toes are the digits of the foot of a tetrapod. Animal species such as cats that walk on their toes are described as being digitigrade. Humans, and other animals that walk on the soles of their feet, are described as being plantigrade; unguligrade animals are those that walk on hooves at the tips of...
. The sciatic nerve
Sciatic nerve
The sciatic nerve is a large nerve fiber in humans and other animals. It begins in the lower back and runs through the buttock and down the lower limb...
is the most commonly affected nerve, causing symptoms of sciatica
Sciatica
Sciatica is a set of symptoms including pain that may be caused by general compression or irritation of one of five spinal nerve roots that give rise to each sciatic nerve, or by compression or irritation of the left or right or both sciatic nerves. The pain is felt in the lower back, buttock, or...
. The femoral nerve
Femoral nerve
The femoral nerve, the largest branch of the lumbar plexus, arises from the dorsal divisions of the ventral rami of the second, third, and fourth lumbar nerves...
can also be affected and cause the patient to experience a numb, tingling feeling throughout one or both legs and even feet or even a burning feeling in the hips and legs.
Pathophysiology
There is now recognition of the importance of “chemical radiculitis” in the generation of back painBack pain
Back pain is pain felt in the back that usually originates from the muscles, nerves, bones, joints or other structures in the spine.The pain can often be divided into neck pain, upper back pain, lower back pain or tailbone pain...
. A primary focus of surgery is to remove “pressure” or reduce mechanical compression on a neural element: either the spinal cord
Spinal cord
The spinal cord is a long, thin, tubular bundle of nervous tissue and support cells that extends from the brain . The brain and spinal cord together make up the central nervous system...
, or a nerve root
Nerve root
A nerve root is the initial segment of a nerve leaving the central nervous system. Types include:* A cranial nerve root, the beginning of one of the twelve pairs leaving the central nervous system from the brain stem or the highest levels of the spinal cord;...
. But it is increasingly recognized that back pain, rather than being solely due to compression, may also be due to chemical inflammation. There is evidence that points to a specific inflammatory mediator of this pain. This inflammatory molecule, called tumor necrosis factor-alpha (TNF), is released not only by the herniated disc, but also in cases of disc tear (annular tear), by facet joints, and in spinal stenosis
Spinal stenosis
Lumbar spinal stenosis is a medical condition in which the spinal canal narrows and compresses the spinal cord and nerves at the level of the lumbar vertebra. This is usually due to the common occurrence of spinal degeneration that occurs with aging. It can also sometimes be caused by spinal disc...
. In addition to causing pain and inflammation, TNF
Tumor necrosis factors
Tumor necrosis factors refers to a group of cytokines family that can cause cell death . The first two members of the family to be identified were:...
may also contribute to disc degeneration.
Diagnosis
Diagnosis is made by a practitioner based on the history, symptoms, and physical examinationPhysical examination
Physical examination or clinical examination is the process by which a doctor investigates the body of a patient for signs of disease. It generally follows the taking of the medical history — an account of the symptoms as experienced by the patient...
. At some point in the evaluation, tests may be performed to confirm or rule out other causes of symptoms such as spondylolisthesis
Spondylolisthesis
Spondylolisthesis describes the anterior or posterior displacement of a vertebra or the vertebral column in relation to the vertebrae below. It was first described in 1782 by Belgian obstetrician, Dr. Herbinaux. He reported a bony prominence anterior to the sacrum that obstructed the vagina of a...
, degeneration, tumor
Tumor
A tumor or tumour is commonly used as a synonym for a neoplasm that appears enlarged in size. Tumor is not synonymous with cancer...
s, metastases and space-occupying lesion
Lesion
A lesion is any abnormality in the tissue of an organism , usually caused by disease or trauma. Lesion is derived from the Latin word laesio which means injury.- Types :...
s, as well as to evaluate the efficacy of potential treatment options.
Physical examination
The Straight leg raiseStraight leg raise
The Straight leg raise, also called Lasègue's sign, Lasègue test or Lazarević's sign, is a test done during the physical examination to determine whether a patient with low back pain has an underlying herniated disk, mostly located at L5 , S1 or S2 .-Technique:With the patient...
may be positive, as this finding has low specificity; however, it has high sensitivity. Thus the finding of a negative SLR sign is an important in helping to "rule out" the possibility of a lower lumbar disc herniation. A variation is to lift the leg while the patient is sitting. However, this reduces the sensitivity of the test.
Imaging
- X-rayX-rayX-radiation is a form of electromagnetic radiation. X-rays have a wavelength in the range of 0.01 to 10 nanometers, corresponding to frequencies in the range 30 petahertz to 30 exahertz and energies in the range 120 eV to 120 keV. They are shorter in wavelength than UV rays and longer than gamma...
: Although traditional plain X-rays are limited in their ability to image soft tissues such as discs, muscles, and nerves, they are still used to confirm or exclude other possibilities such as tumors, infections, fractures, etc. In spite of these limitations, X-ray can still play a relatively inexpensive role in confirming the suspicion of the presence of a herniated disc. If a suspicion is thus strengthened, other methods may be used to provide final confirmation. - Computed tomographyComputed tomographyX-ray computed tomography or Computer tomography , is a medical imaging method employing tomography created by computer processing...
scan (CT or CAT scan): A diagnostic image created after a computer reads x-rays. It can show the shape and size of the spinal canal, its contents, and the structures around it, including soft tissues. However, visual confirmation of a disc herniation can be difficult with a CT. - Magnetic resonance imagingMagnetic resonance imagingMagnetic resonance imaging , nuclear magnetic resonance imaging , or magnetic resonance tomography is a medical imaging technique used in radiology to visualize detailed internal structures...
(MRI): A diagnostic test that produces three-dimensional images of body structures using powerful magnets and computer technology. It can show the spinal cord, nerve roots, and surrounding areas, as well as enlargement, degeneration, and tumors. It shows soft tissues even better than CAT scans. An MRI performed with a high magnetic field strength usually provides the most conclusive evidence for diagnosis of a disc herniation. T2-weighted images allow for clear visualization of protruded disc material in the spinal canal. - MyelogramMyelographyMyelography is a type of radiographic examination that uses a contrast medium to detect pathology of the spinal cord, including the location of a spinal cord injury, cysts, and tumors...
: An x-ray of the spinal canal following injection of a contrast material into the surrounding cerebrospinal fluid spaces. By revealing displacement of the contrast material, it can show the presence of structures that can cause pressure on the spinal cord or nerves, such as herniated discs, tumors, or bone spurBone spurOsteophytes, commonly referred to as bone spurs, are bony projections that form along joint margins. They should not be confused with enthesophytes, which are bony projections which form at the attachment of a tendon or ligament.-Pathophysiology:...
s. Because it involves the injection of foreign substances, MRI scans are now preferred in most patients. Myelograms still provide excellent outlines of space-occupying lesions, especially when combined with CT scanning (CT myelography). - ElectromyogramElectromyographyElectromyography is a technique for evaluating and recording the electrical activity produced by skeletal muscles. EMG is performed using an instrument called an electromyograph, to produce a record called an electromyogram. An electromyograph detects the electrical potential generated by muscle...
and Nerve conduction studies (EMG/NCS): These tests measure the electrical impulse along nerve roots, peripheral nerves, and muscle tissue. This will indicate whether there is ongoing nerve damage, if the nerves are in a state of healing from a past injury, or whether there is another site of nerve compression. EMG/NCS studies are typically used to pinpoint the sources of nerve dysfunction distal to the spine.
Differential diagnosis
- Mechanical painPainPain is an unpleasant sensation often caused by intense or damaging stimuli such as stubbing a toe, burning a finger, putting iodine on a cut, and bumping the "funny bone."...
- Discogenic painPainPain is an unpleasant sensation often caused by intense or damaging stimuli such as stubbing a toe, burning a finger, putting iodine on a cut, and bumping the "funny bone."...
- Myofacial painPainPain is an unpleasant sensation often caused by intense or damaging stimuli such as stubbing a toe, burning a finger, putting iodine on a cut, and bumping the "funny bone."...
- SpondylosisSpondylosisSpondylosis is a term referring to degenerative osteoarthritis of the joints between the centra of the spinal vertebrae and/or neural foraminae. If this condition occurs in the zygapophysial joints, it can be considered facet syndrome...
/spondylolisthesisSpondylolisthesisSpondylolisthesis describes the anterior or posterior displacement of a vertebra or the vertebral column in relation to the vertebrae below. It was first described in 1782 by Belgian obstetrician, Dr. Herbinaux. He reported a bony prominence anterior to the sacrum that obstructed the vagina of a... - Spinal stenosisSpinal stenosisLumbar spinal stenosis is a medical condition in which the spinal canal narrows and compresses the spinal cord and nerves at the level of the lumbar vertebra. This is usually due to the common occurrence of spinal degeneration that occurs with aging. It can also sometimes be caused by spinal disc...
- AbscessAbscessAn abscess is a collection of pus that has accumulated in a cavity formed by the tissue in which the pus resides due to an infectious process or other foreign materials...
- HematomaHematomaA hematoma, or haematoma, is a localized collection of blood outside the blood vessels, usually in liquid form within the tissue. This distinguishes it from an ecchymosis, which is the spread of blood under the skin in a thin layer, commonly called a bruise...
- Discitis/osteomyelitisOsteomyelitisOsteomyelitis simply means an infection of the bone or bone marrow...
- Mass lesion/malignancy
- Myocardial infarctionMyocardial infarctionMyocardial infarction or acute myocardial infarction , commonly known as a heart attack, results from the interruption of blood supply to a part of the heart, causing heart cells to die...
- Aortic dissectionAortic dissectionAortic dissection occurs when a tear in the inner wall of the aorta causes blood to flow between the layers of the wall of the aorta and force the layers apart. The dissection typically extends anterograde, but can extend retrograde from the site of the intimal tear. Aortic dissection is a medical...
Treatment
The majority of herniated discs will heal themselves in about six weeks and do not require surgery. One study on sciaticaSciatica
Sciatica is a set of symptoms including pain that may be caused by general compression or irritation of one of five spinal nerve roots that give rise to each sciatic nerve, or by compression or irritation of the left or right or both sciatic nerves. The pain is felt in the lower back, buttock, or...
, which can be caused by spinal disc herniation, found that "After 12 weeks, 73% of patients showed reasonable to major improvement without surgery." The study, however, did not determine the number of individuals in the group that had sciatica caused by disc herniation.
If pain due to disc herniation, protrusion, bulge, or disc tear is due to chemical radiculitis pain, then prior to surgery it may make sense to try an anti-inflammatory approach. Often this is first attempted with non-steroidal anti-inflammatory medications (NSAIDs), but the long-term use of NSAIDs for patients with persistent back pain is complicated by their possible cardiovascular and gastrointestinal toxicity; and NSAIDs have limited value to intervene in tumor necrosis factor-alpha (TNF)-mediated processes. An alternative often employed is the injection of cortisone
Cortisone
Cortisone is a steroid hormone. It is one of the main hormones released by the adrenal gland in response to stress. In chemical structure, it is a corticosteroid closely related to corticosterone. It is used to treat a variety of ailments and can be administered intravenously, orally,...
into the spine adjacent to the suspected pain generator, a technique known as “epidural steroid injection”. Although this technique began more than a decade ago for pain due to disc herniation, the efficacy of epidural steroid injections is now generally thought to be limited to short term pain relief in selected patients only. In addition, epidural steroid injections, in certain settings, may result in serious complications. Fortunately there are now emerging new methods that directly target TNF. These TNF-targeted methods represent a highly promising new approach for patients with chronic severe spinal pain, such as those with failed back surgery syndrome. Ancillary approaches, such as rehabilitation, physical therapy
Physical therapy
Physical therapy , often abbreviated PT, is a health care profession. Physical therapy is concerned with identifying and maximizing quality of life and movement potential within the spheres of promotion, prevention, diagnosis, treatment/intervention,and rehabilitation...
, anti-depressants, and, in particular, graduated exercise programs, may all be useful adjuncts to anti-inflammatory approaches.
Lumbar
Non-surgical methods of treatment are usually attempted first, leaving surgery as a last resort. Pain medications are often prescribed as the first attempt to alleviate the acute pain and allow the patient to begin exercising and stretching. There are a variety of other non-surgical methods used in attempts to relieve the condition after it has occurred, often in combination with pain killers. They are either considered indicatedIndication (medicine)
In medicine, an indication is a valid reason to use a certain test, medication, procedure, or surgery. The opposite of indication is contraindication.-Drugs:...
, contraindicated
Contraindication
In medicine, a contraindication is a condition or factor that serves as a reason to withhold a certain medical treatment.Some contraindications are absolute, meaning that there are no reasonable circumstances for undertaking a course of action...
, relatively contraindicated, or inconclusive based on the safety profile of their risk-benefit ratio
Risk-benefit analysis
Risk–benefit analysis is the comparison of the risk of a situation to its related benefits. Exposure to personal risk is recognized as a normal aspect of everyday life. We accept a certain level of risk in our lives as necessary to achieve certain benefits. In most of these risks we feel as though...
and on whether they may or may not help:
Indicated
- Patient education on proper body mechanics
- Physical therapyPhysical therapyPhysical therapy , often abbreviated PT, is a health care profession. Physical therapy is concerned with identifying and maximizing quality of life and movement potential within the spheres of promotion, prevention, diagnosis, treatment/intervention,and rehabilitation...
, to address mechanical factors, and may include modalities to temporarily relieve pain (i.e. tractionTraction (orthopedics)In orthopedic medicine, traction refers to the set of mechanisms for straightening broken bones or relieving pressure on the spine and skeletal system.There are two types of traction: skin traction and skeletal traction....
, electrical stimulation, massageMassageMassage is the manipulation of superficial and deeper layers of muscle and connective tissue to enhance function, aid in the healing process, and promote relaxation and well-being. The word comes from the French massage "friction of kneading", or from Arabic massa meaning "to touch, feel or handle"...
) - Non-steroidal anti-inflammatory drugs (NSAIDs)
- Oral steroids (e.g. prednisonePrednisonePrednisone is a synthetic corticosteroid drug that is particularly effective as an immunosuppressant drug. It is used to treat certain inflammatory diseases and some types of cancer, but has significant adverse effects...
or methylprednisoloneMethylprednisoloneMethylprednisolone is a synthetic glucocorticoid or corticosteroid drug. It is marketed in the USA and Canada under the brand names Medrol and Solu-Medrol. It is also available as a generic drug....
) - EpiduralEpiduralThe term epidural is often short for epidural analgesia, a form of regional analgesia involving injection of drugs through a catheter placed into the epidural space...
(cortisoneCortisoneCortisone is a steroid hormone. It is one of the main hormones released by the adrenal gland in response to stress. In chemical structure, it is a corticosteroid closely related to corticosterone. It is used to treat a variety of ailments and can be administered intravenously, orally,...
) injection - Intravenous sedation, analgesia-assisted traction therapy (IVSAAT)
- Weight control
- Tobacco cessation
- Lumbosacral back support
Contraindicated
- Spinal manipulationSpinal manipulationSpinal manipulation is a therapeutic intervention performed on spinal articulations which are synovial joints . These articulations in the spine that are amenable to spinal manipulative therapy include the z-joints, the atlanto-occipital, atlanto-axial, lumbosacral, sacroiliac, costotransverse...
: A 2006 review of published research stated: "Contradictions in the literature exist in terms of the use of spinal manipulation in the management of disc herniation, with some authors advocating its usefulness, and others suggesting it is contraindicated. It is likely to be safe when used by appropriately-trained practitioners; however, some of the reports discussed highlight the importance of a thorough case history and physical examination." According to the WHOWhoWho may refer to:* Who , an English-language pronoun* who , a Unix command* Who?, one of the Five Ws in journalism- Art and entertainment :* Who? , a 1958 novel by Algis Budrys...
, in their guidelines on chiropracticChiropracticChiropractic is a health care profession concerned with the diagnosis, treatment and prevention of disorders of the neuromusculoskeletal system and the effects of these disorders on general health. It is generally categorized as complementary and alternative medicine...
practice, when there is a "frank disc herniation with accompanying signs of progressive neurological deficit", it is absolutely contraindicated.
Inconclusive
- Non-surgical spinal decompression: A 2007 review of published research on this treatment method found shortcomings in most published studies and concluded that there was only "very limited evidence in the scientific literatureScientific literatureScientific literature comprises scientific publications that report original empirical and theoretical work in the natural and social sciences, and within a scientific field is often abbreviated as the literature. Academic publishing is the process of placing the results of one's research into the...
to support the effectiveness of non-surgical spinal decompression therapy." Its use and marketing have been very controversial.
Surgical
Surgery should only be considered as a last resort after all conservative treatments (non-surgical therapy) have been tried, that did not alleviate the pain and heal the disc herniation. Also, surgery is indicated if a patient has a significant neurological deficit. The presence of cauda equina syndromeCauda equina syndrome
Cauda equina syndrome ' is a serious neurologic condition in which there is acute loss of function of the lumbar plexus, neurologic elements of the spinal canal below the termination of the spinal cord.-Causes:...
(in which there is incontinence, weakness and genital numbness) is considered a medical emergency requiring immediate attention and possibly surgical decompression.
Any claim of absolute contraindications for lumbar disc disease would invariably be challenged. Most spine surgeons adhere to some guidelines, including the following:
• A patient with unrelenting back pain: Patients who have back pain after a bout of sciatica has resolved are not good candidates for operative treatment. Often, these patients are the most insistent and difficult to manage. Occasionally, these are patients whose back pain improved after discectomy for a large central disc herniation.
• A patient with an incomplete workup: When diagnosis is uncertain, postpone surgery. Disc herniations are so ubiquitous that being cavalier in diagnosis is easy. Ensure the completeness of the workup prior to proceeding with the operation. All surgeons can recall several cases in which a diabetic plexopathy or an epidural metastasis was missed.
• A patient not provided adequate conservative treatment: Spine surgeons rarely commit a patient with a short period of sciatica and without bedrest and a steroid trial to an operation that will permanently alter the patient's back mechanics and strength.
Regarding the role of surgery for failed medical therapy in patients without a significant neurological deficit, a meta-analysis
Meta-analysis
In statistics, a meta-analysis combines the results of several studies that address a set of related research hypotheses. In its simplest form, this is normally by identification of a common measure of effect size, for which a weighted average might be the output of a meta-analyses. Here the...
of randomized controlled trials by the Cochrane Collaboration
Cochrane Collaboration
The Cochrane Collaboration is a group of over 28,000 volunteers in more than 100 countries who review the effects of health care interventions tested in biomedical randomized controlled trials. A few more recent reviews have also studied the results of non-randomized, observational studies...
concluded that "limited evidence is now available to support some aspects of surgical practice". More recent randomized controlled trials refine indications for surgery as follows:
- The Spine Patient Outcomes Research Trial (SPORT)
- Patients studied "intervertebral disk herniation and persistent symptoms despite some nonoperative treatment for at least 6 weeks...radicular pain (below the knee for lower lumbar herniations, into the anterior thigh for upper lumbar herniations) and evidence of nerve-root irritation with a positive nerve-root tension sign (straight leg raise–positive between 30° and 70° or positive femoral tension sign) or a corresponding neurologic deficit (asymmetrical depressed reflex, decreased sensation in a dermatomal distribution, or weakness in a myotomal distribution)
- Conclusions. "Patients in both the surgery and the nonoperative treatment groups improved substantially over a 2-year period. Because of the large numbers of patients who crossed over in both directions, conclusions about the superiority or equivalence of the treatments are not warranted based on the intent-to-treat analysis"
- The Hague Spine Intervention Prognostic Study Group
- Patients studied "had a radiologically confirmed disk herniation...incapacitating lumbosacral radicular syndrome that had lasted for 6 to 12 weeks...Patients presenting with cauda equina syndrome, muscle paralysis, or insufficient strength to move against gravity were excluded."
- Conclusions. "The 1-year outcomes were similar for patients assigned to early surgery and those assigned to conservative treatment with eventual surgery if needed, but the rates of pain relief and of perceived recovery were faster for those assigned to early surgery."
Surgical options
- ChemonucleolysisChymopapainChymopapain is a proteolytic enzyme isolated from the latex of papaya , it is a medication used to treat slipped lower lumbar discs in the spine. Chymopapain injections should preferably be given under local, rather than general, anaesthesia...
- dissolves the protruding disc - IDET (a minimally invasive surgery for disc pain)
- Discectomy/MicrodiscectomyDiscectomyA Discectomy is the surgical removal of herniated disc material that presses on a nerve root or the spinal cord. The procedure involves removing the central portion of an intervertebral disc, the nucleus pulposus, which causes pain by stressing the spinal cord or radiating nerves...
- to relieve nerve compression - Tessys methodTessys methodThe Tessys method is a minimally invasive surgical procedure for the treatment of herniated discs.- Concept :...
- a transforaminal endoscopic method to remove herniated discs - LaminectomyLaminectomyLaminectomy is a spine operation to remove the portion of the vertebral bone called the lamina. There are many variations of laminectomy. In the most minimal form small skin incisions are made, back muscles are pushed aside rather than cut, and the parts of the vertebra adjacent to the lamina are...
- to relieve spinal stenosis or nerve compression - Hemilaminectomy - to relieve spinal stenosis or nerve compression
- Lumbar fusion (lumbar fusion is only indicated for recurrent lumbar disc herniations, not primary herniations)
- Anterior cervical discectomy and fusion (for cervical disc herniation)
- Disc arthroplasty (experimental for cases of cervical disc herniation)
- Dynamic stabilization
- Artificial disc replacement, a relatively new form of surgery in the U.S. but has been in use in Europe for decades, primarily used to treat low back pain from a degenerated discDegenerative disc diseaseDegeneration of the intervertebral disc, often called "degenerative disc disease" of the spine, is a condition that can be painful and can greatly affect the quality of one's life...
. - Nucleoplasty
Surgical goals include relief of nerve compression, allowing the nerve to recover, as well as the relief of associated back pain and restoration of normal function.
Complications
- Permanent nerve injuryNerve injuryNerve injury is injury to nervous tissue. There is no single classification system that can describe all the many variations of nerve injury. Most systems attempt to correlate the degree of injury with symptoms, pathology and prognosis...
- Cauda equina syndromeCauda equina syndromeCauda equina syndrome ' is a serious neurologic condition in which there is acute loss of function of the lumbar plexus, neurologic elements of the spinal canal below the termination of the spinal cord.-Causes:...
- ParalysisParalysisParalysis is loss of muscle function for one or more muscles. Paralysis can be accompanied by a loss of feeling in the affected area if there is sensory damage as well as motor. A study conducted by the Christopher & Dana Reeve Foundation, suggests that about 1 in 50 people have been diagnosed...
- Chronic painChronic painChronic pain has several different meanings in medicine. Traditionally, the distinction between acute and chronic pain has relied upon an arbitrary interval of time from onset; the two most commonly used markers being 3 months and 6 months since the initiation of pain, though some theorists and...
Epidemiology

Sciatica
Sciatica is a set of symptoms including pain that may be caused by general compression or irritation of one of five spinal nerve roots that give rise to each sciatic nerve, or by compression or irritation of the left or right or both sciatic nerves. The pain is felt in the lower back, buttock, or...
.
Lumbar disc herniation occurs 15 times more often than cervical (neck) disc herniation, and it is one of the most common causes of lower back pain. The cervical discs are affected 8% of the time and the upper-to-mid-back (thoracic) discs only 1 - 2% of the time.
The following locations have no discs and are therefore exempt from the risk of disc herniation: the upper two cervical intervertebral spaces, the sacrum
Sacrum
In vertebrate anatomy the sacrum is a large, triangular bone at the base of the spine and at the upper and back part of the pelvic cavity, where it is inserted like a wedge between the two hip bones. Its upper part connects with the last lumbar vertebra, and bottom part with the coccyx...
, and the coccyx
Coccyx
The coccyx , commonly referred to as the tailbone, is the final segment of the vertebral column. Comprising three to five separate or fused vertebrae below the sacrum, it is attached to the sacrum by a fibrocartilaginous joint, the sacrococcygeal symphysis, which permits limited movement between...
.
Most disc herniations occur when a person is in their thirties or forties when the nucleus pulposus is still a gelatin-like substance. With age the nucleus pulposus changes ("dries out") and the risk of herniation is greatly reduced. After age 50 or 60, osteoarthritic
Osteoarthritis
Osteoarthritis also known as degenerative arthritis or degenerative joint disease, is a group of mechanical abnormalities involving degradation of joints, including articular cartilage and subchondral bone. Symptoms may include joint pain, tenderness, stiffness, locking, and sometimes an effusion...
degeneration (spondylosis) or spinal stenosis
Spinal stenosis
Lumbar spinal stenosis is a medical condition in which the spinal canal narrows and compresses the spinal cord and nerves at the level of the lumbar vertebra. This is usually due to the common occurrence of spinal degeneration that occurs with aging. It can also sometimes be caused by spinal disc...
are more likely causes of low back pain
Low back pain
Low back pain or lumbago is a common musculoskeletal disorder affecting 80% of people at some point in their lives. In the United States it is the most common cause of job-related disability, a leading contributor to missed work, and the second most common neurological ailment — only headache is...
or leg pain.
- 4.8% males and 2.5% females older than 35 experience sciaticaSciaticaSciatica is a set of symptoms including pain that may be caused by general compression or irritation of one of five spinal nerve roots that give rise to each sciatic nerve, or by compression or irritation of the left or right or both sciatic nerves. The pain is felt in the lower back, buttock, or...
during their lifetime. - Of all individuals, 60% to 80% experience back painBack painBack pain is pain felt in the back that usually originates from the muscles, nerves, bones, joints or other structures in the spine.The pain can often be divided into neck pain, upper back pain, lower back pain or tailbone pain...
during their lifetime. - In 14%, pain lasts more than 2 weeks.
- Generally, males have a slightly higher incidence than females.
Research
The identification of tumor necrosis factor-alpha (TNF) as a central cause of inflammatory spinal pain now suggests the possibility of an entirely new approach to selected patients with severe pain due to disc herniation, protrusion, bulge, or disc tear. Specific and potent inhibitors of TNFTumor necrosis factors
Tumor necrosis factors refers to a group of cytokines family that can cause cell death . The first two members of the family to be identified were:...
became available in the U.S. in 1998, and were demonstrated to be potentially effective for treating sciatica
Sciatica
Sciatica is a set of symptoms including pain that may be caused by general compression or irritation of one of five spinal nerve roots that give rise to each sciatic nerve, or by compression or irritation of the left or right or both sciatic nerves. The pain is felt in the lower back, buttock, or...
in experimental models beginning in 2001. Targeted anatomic administration of one of these anti-TNF agents, etanercept
Etanercept
Etanercept is a drug that treats autoimmune diseases by interfering with the tumor necrosis factor by acting as a TNF inhibitor. Pfizer describes in a SEC filing that the drug is used to treat rheumatoid, juvenile rheumatoid and psoriatic arthritis, plaque psoriasis and ankylosing spondylitis...
, a patented treatment method, has been suggested in published pilot studies to be effective for treating selected patients with severe pain due to disc herniation, protrusion, bulge, or disc tear. The scientific basis for pain relief in these patients is supported by the most current review articles. In the future new imaging methods may allow non-invasive identification of sites of neuronal inflammation, thereby enabling more accurate localization of the "pain generators" responsible for symptom production.
Future treatments may include stem cell therapy. Doctors Victor Y. L. Leung, Danny Chan and Kenneth M. C. Cheung have reported in the European Spine Journal that "substantial progress has been made in the field of stem cell regeneration of the intervertebral disc. Autogenic mesenchymal stem cells in animal models can arrest intervertebral disc degeneration or even partially regenerate it and the effect is suggested to be dependent on the severity of the degeneration."
External links
- Herniated Disc - WebMDWebMDWebMD is an American corporation which provides health information services. It was founded in 1996 by Jim Clark and Pavan Nigam as Healthscape, later Healtheon, and then acquired WebMD in 1999 to form Healtheon/WebMD...

