Spirometry
Encyclopedia
Spirometry is the most common of the pulmonary function tests (PFTs), measuring lung
function, specifically the measurement of the amount (volume) and/or speed (flow) of air that can be inhaled and exhaled. Spirometry is an important tool used for generating pneumotachographs which are helpful in assessing conditions such as asthma
, pulmonary fibrosis
, cystic fibrosis
, and COPD
.

 The spirometry test is performed using a device called a spirometer
The spirometry test is performed using a device called a spirometer
, which comes in several different varieties. Most spirometers display the following graphs, called spirograms:
Generally, the patient is asked to take the deepest breath they can, and then exhale into the sensor as hard as possible, for as long as possible, preferably at least 6 seconds. It is sometimes directly followed by a rapid inhalation (inspiration), in particular when assessing possible upper airway obstruction. Sometimes, the test will be preceded by a period of quiet breathing in and out from the sensor (tidal volume), or the rapid breath in (forced inspiratory part) will come before the forced exhalation.
During the test, soft nose clips may be used to prevent air escaping through the nose. Filter mouthpieces may be used to prevent the spread of microorganisms.
Due to the patient cooperation required, spirometry can only be used on children old enough to comprehend and follow the instructions given (6 years old or more), and only on patients who are able to understand and follow instructions — thus, this test is not suitable for patients who are unconscious, heavily sedated, or have limitations that would interfere with vigorous respiratory efforts. Other types of lung function tests are available for infants and unconscious persons.
Another major limitation is the fact that many intermittent or mild asthmatics have normal spirometry between acute exacerbation, limiting spirometry's usefulness as a diagnostic. It is more useful as a monitoring tool: a sudden decrease in FEV1 or other spirometric measure in the same patient can signal worsening control, even if the raw value is still normal. Patients are encouraged to record their personal best measures.
, used to determine bronchial hyperresponsiveness to either rigorous exercise, inhalation of cold/dry air, or with a pharmaceutical agent such as methacholine or histamine
.
Sometimes, to assess the reversibility of a particular condition, a bronchodilator
is administered before performing another round of tests for comparison. This is commonly referred to as a reversibility test, or a post bronchodilator test (Post BD), and is an important part in diagnosing asthma versus COPD.
Other complementary lung functions tests include plethysmography and nitrogen washout.
The most common parameters measured in spirometry are Vital capacity (VC), Forced vital capacity (FVC), Forced expiratory volume (FEV) at timed intervals of 0.5, 1.0 (FEV1), 2.0, and 3.0 seconds, Forced expiratory flow 25–75% (FEF 25–75) and Maximal voluntary ventilation (MVV), also known as Maximum breathing capacity. Other tests may be performed in certain situations.
Results are usually given in both raw data (litres, litres per second) and percent predicted — the test result as a percent of the "predicted values" for the patients of similar characteristics (height, age, sex, and sometimes race and weight). The interpretation of the results can vary depending on the physician and the source of the predicted values. Generally speaking, results nearest to 100% predicted are the most normal, and results over 80% are often considered normal. Multiple publications of predicted values have been published and may be calculated online based on age, sex, weight and ethnicity. However, review by a doctor is necessary for accurate diagnosis of any individual situation.
A bronchodilator is also given in certain circumstances and a pre/post graph comparison is done to assess the effectiveness of the bronchodilator. See the example printout.
Functional residual capacity
(FRC) cannot be measured via spirometry, but it can be measured with a plethysmograph
or dilution tests (for example, helium dilution test).
(FVC) is the volume of air that can forcibly be blown out after full inspiration, measured in liters. FVC is the most basic maneuver in spirometry tests.
Values of between 80% and 120% of the average value are considered normal. Predicted normal values for FEV1 can be calculated online and depend on age, sex, height, weight and ethnicity as well as the research study that they are based upon.
(FEV1%) is the ratio of FEV1 to FVC. In healthy adults this should be approximately 75–80%. In obstructive diseases (asthma, COPD, chronic bronchitis, emphysema) FEV1 is diminished because of increased airway resistance to expiratory flow; the FVC may be decreased as well, due to the premature closure of airway in expiration, just not in the same proportion as FEV1 (for instance, both FEV1 and FVC are reduced, but the former is more affected because of the increased airway resistance). This generates a reduced value (<80%, often ~45%). In restrictive diseases (such as pulmonary fibrosis
) the FEV1 and FVC are both reduced proportionally and the value may be normal or even increased as a result of decreased lung compliance.
A derived value of FEV1% is FEV1% predicted, which is defined as FEV1% of the patient divided by the average FEV1% in the population for any person of similar age, sex and body composition.
s, generally defined by what fraction remains of the forced vital capacity (FVC). The usual intervals are 25%, 50% and 75% (FEF25, FEF50 and FEF75), or 25% and 50% of FVC. It can also be given as a mean of the flow during an interval, also generally delimited by when specific fractions remain of FVC, usually 25–75% (FEF25–75%). Average ranges in the healthy population depend mainly on sex and age, with FEF25–75% shown in diagram at left. Values ranging from 50-60% and up to 130% of the average are considered normal. Predicted normal values for FEF can be calculated online and depend on age, sex, height, weight and ethnicity as well as the research study that they are based upon.
MMEF or MEF stands for maximal (mid-)expiratory flow and is the peak of expiratory flow as taken from the flow-volume curve and measured in liters per second. It should theoretically be identical to peak expiratory flow (PEF), which is, however, generally measured by a peak flow meter and given in liters per minute.
Recent research suggests that FEF25-75% or FEF25-50% may be a more sensitive parameter than FEV1 in the detection of obstructive small airway disease. However, in the absence of concomitant changes in the standard markers, discrepancies in mid-range expiratory flow may not be specific enough to be useful, and current practice guidelines recommend continuing to use FEV1, VC, and FEV1/VC as indicators of obstructive disease.
More rarely, forced expiratory flow may be given at intervals defined by how much remains of total lung capacity. In such cases, it is usually designated as e.g. FEF70%TLC, FEF60%TLC and FEF50%TLC.
(TV) is the volume of air inspired or expired in a single breath at rest.
)is the carbon monoxide uptake from a single inspiration in a standard time (usually 10 sec). Since air consists of very minute or trace quantities of CO, 10 seconds is considered to be the standard time for inhalation, then rapidly blow it out (exhale). The exhaled gas is tested to determine how much of the tracer gas was absorbed during the breath. This will pick up diffusion impairments, for instance in pulmonary fibrosis. This must be corrected for anemia (because rapid CO diffusion is dependent on hemoglobin in RBC's; a low hemoglobin concentration, anemia, will reduce DLCO) and pulmonary hemorrhage (excess RBC's in the interstitium or alveoli can absorb CO and artificially increase the DLCO capacity). Atmospheric pressure and/or altitude will also affect measured DLCO, and so a correction factor is needed to adjust for standard pressure. Online calculators are available to correct for hemoglobin levels and altitude and/or pressure where the measurement was taken.
. When having drawn a curve with the relations between changes in volume to changes in transpulmonary pressure, Cst is the slope of the curve during any given volume, or, mathematically, ΔV/ΔP. Static lung compliance is perhaps the most sensitive parameter for the detection of abnormal pulmonary mechanics. It is considered normal if it is 60% to 140% of the average value in the population for any person of similar age, sex and body composition.
In those with acute respiratory failure on mechanical ventilation, "the static compliance of the total respiratory system is conventionally obtained by dividing the tidal volume by the difference between the "plateau" pressure measured at the airway opening (PaO) during an occlusion at end-inspiration and positive end-expiratory pressure (PEEP) set by the ventilator".
Forced Expiratory Time (FET) measures the length of the expiration in seconds.
Slow vital capacity (SVC)
Slow vital capacity
(SVC) is the maximum volume of air that can be exhaled slowly after slow maximum inhalation.
Maximal pressure (Pmax and Pi)
Pmax is the asymptotically maximal pressure that can be developed by the respiratory muscles at any lung volume and Pi is the maximum inspiratory pressure that can be developed at specific lung volumes. This measurement also requires pressure transducers in addition. It is considered normal if it is 60% to 140% of the average value in the population for any person of similar age, sex and body composition. A derived parameter is the coefficient of retraction (CR) which is Pmax/TLC .
Mean transit time (MTT)
Mean transit time is the area under the flow-volume curve divided by the forced vital capacity.
Lung
The lung is the essential respiration organ in many air-breathing animals, including most tetrapods, a few fish and a few snails. In mammals and the more complex life forms, the two lungs are located near the backbone on either side of the heart...
function, specifically the measurement of the amount (volume) and/or speed (flow) of air that can be inhaled and exhaled. Spirometry is an important tool used for generating pneumotachographs which are helpful in assessing conditions such as asthma
Asthma
Asthma is the common chronic inflammatory disease of the airways characterized by variable and recurring symptoms, reversible airflow obstruction, and bronchospasm. Symptoms include wheezing, coughing, chest tightness, and shortness of breath...
, pulmonary fibrosis
Pulmonary fibrosis
Pulmonary fibrosis is the formation or development of excess fibrous connective tissue in the lungs. It is also described as "scarring of the lung".-Symptoms:Symptoms of pulmonary fibrosis are mainly:...
, cystic fibrosis
Cystic fibrosis
Cystic fibrosis is a recessive genetic disease affecting most critically the lungs, and also the pancreas, liver, and intestine...
, and COPD
Chronic obstructive pulmonary disease
Chronic obstructive pulmonary disease , also known as chronic obstructive lung disease , chronic obstructive airway disease , chronic airflow limitation and chronic obstructive respiratory disease , is the co-occurrence of chronic bronchitis and emphysema, a pair of commonly co-existing diseases...
.
Spirometry testing


Spirometer
A spirometer is an apparatus for measuring the volume of air inspired and expired by the lungs. It is a precision differential pressure transducer for the measurements of respiration flow rates. The spirometer records the amount of air and the rate of air that is breathed in and out over a...
, which comes in several different varieties. Most spirometers display the following graphs, called spirograms:
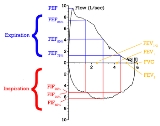
- a volume-time curve, showing volume (liters) along the Y-axis and time (seconds) along the X-axis
- a flow-volume loop, which graphically depicts the rate of airflow on the Y-axis and the total volume inspiredInhalationInhalation is the movement of air from the external environment, through the air ways, and into the alveoli....
or expiredExhalationExhalation is the movement of air out of the bronchial tubes, through the airways, to the external environment during breathing....
on the X-axis
Procedure
The basic forced volume vital capacity (FVC) test varies slightly depending on the equipment used.Generally, the patient is asked to take the deepest breath they can, and then exhale into the sensor as hard as possible, for as long as possible, preferably at least 6 seconds. It is sometimes directly followed by a rapid inhalation (inspiration), in particular when assessing possible upper airway obstruction. Sometimes, the test will be preceded by a period of quiet breathing in and out from the sensor (tidal volume), or the rapid breath in (forced inspiratory part) will come before the forced exhalation.
During the test, soft nose clips may be used to prevent air escaping through the nose. Filter mouthpieces may be used to prevent the spread of microorganisms.
Limitations of test
The maneuver is highly dependent on patient cooperation and effort, and is normally repeated at least three times to ensure reproducibility. Since results are dependent on patient cooperation, FVC can only be underestimated, never overestimated. FEV1 may sometimes be overestimated in people with some diseases — a softer blow can reduce the spasm or collapse of lung tissue to elevate the measure.Due to the patient cooperation required, spirometry can only be used on children old enough to comprehend and follow the instructions given (6 years old or more), and only on patients who are able to understand and follow instructions — thus, this test is not suitable for patients who are unconscious, heavily sedated, or have limitations that would interfere with vigorous respiratory efforts. Other types of lung function tests are available for infants and unconscious persons.
Another major limitation is the fact that many intermittent or mild asthmatics have normal spirometry between acute exacerbation, limiting spirometry's usefulness as a diagnostic. It is more useful as a monitoring tool: a sudden decrease in FEV1 or other spirometric measure in the same patient can signal worsening control, even if the raw value is still normal. Patients are encouraged to record their personal best measures.
Related tests
Spirometry can also be part of a bronchial challenge testBronchial challenge test
A bronchial challenge test is a medical test used to assist in the diagnosis of asthma. The patient breathes in nebulized methacholine or histamine. Thus the test may also be called a methacholine challenge test or histamine challenge test respectively. Both drugs provoke bronchoconstriction, or...
, used to determine bronchial hyperresponsiveness to either rigorous exercise, inhalation of cold/dry air, or with a pharmaceutical agent such as methacholine or histamine
Histamine
Histamine is an organic nitrogen compound involved in local immune responses as well as regulating physiological function in the gut and acting as a neurotransmitter. Histamine triggers the inflammatory response. As part of an immune response to foreign pathogens, histamine is produced by...
.
Sometimes, to assess the reversibility of a particular condition, a bronchodilator
Bronchodilator
A bronchodilator is a substance that dilates the bronchi and bronchioles, decreasing resistance in the respiratory airway and increasing airflow to the lungs. Bronchodilators may be endogenous , or they may be medications administered for the treatment of breathing difficulties...
is administered before performing another round of tests for comparison. This is commonly referred to as a reversibility test, or a post bronchodilator test (Post BD), and is an important part in diagnosing asthma versus COPD.
Other complementary lung functions tests include plethysmography and nitrogen washout.
Parameters
| Measurement | Approximate value | ||||||
| Male | Female >- | Forced vital capacity (FVC) |
4.8 L | >- | 500mL | >- | 6.0 L | 4.7 L |
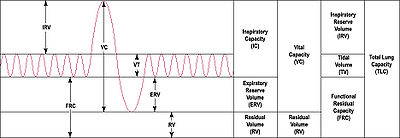
The most common parameters measured in spirometry are Vital capacity (VC), Forced vital capacity (FVC), Forced expiratory volume (FEV) at timed intervals of 0.5, 1.0 (FEV1), 2.0, and 3.0 seconds, Forced expiratory flow 25–75% (FEF 25–75) and Maximal voluntary ventilation (MVV), also known as Maximum breathing capacity. Other tests may be performed in certain situations.
Results are usually given in both raw data (litres, litres per second) and percent predicted — the test result as a percent of the "predicted values" for the patients of similar characteristics (height, age, sex, and sometimes race and weight). The interpretation of the results can vary depending on the physician and the source of the predicted values. Generally speaking, results nearest to 100% predicted are the most normal, and results over 80% are often considered normal. Multiple publications of predicted values have been published and may be calculated online based on age, sex, weight and ethnicity. However, review by a doctor is necessary for accurate diagnosis of any individual situation.
A bronchodilator is also given in certain circumstances and a pre/post graph comparison is done to assess the effectiveness of the bronchodilator. See the example printout.
Functional residual capacity
Functional residual capacity
Functional Residual Capacity is the volume of air present in the lungs, specifically the parenchyma tissues, at the end of passive expiration...
(FRC) cannot be measured via spirometry, but it can be measured with a plethysmograph
Plethysmograph
A plethysmograph is an instrument for measuring changes in volume within an organ or whole body .-Lungs:...
or dilution tests (for example, helium dilution test).
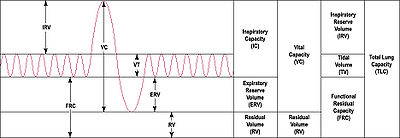
Forced vital capacity (FVC)
Forced vital capacityVital capacity
Vital capacity is the maximum amount of air a person can expel from the lungs after a maximum inspiration. It is equal to the inspiratory reserve volume plus the tidal volume plus the expiratory reserve volume....
(FVC) is the volume of air that can forcibly be blown out after full inspiration, measured in liters. FVC is the most basic maneuver in spirometry tests.
Forced expiratory volume in 1 second (FEV1)
Average values for FEV1 in healthy people depend mainly on sex and age, according to the diagram at left.Values of between 80% and 120% of the average value are considered normal. Predicted normal values for FEV1 can be calculated online and depend on age, sex, height, weight and ethnicity as well as the research study that they are based upon.
FEV1/FVC ratio (FEV1%)
FEV1/FVCFEV1/FVC ratio
The FEV1/FVC ratio, also called Tiffeneau index, is a calculated ratio used in the diagnosis of obstructive and restrictive lung disease.It represents the proportion of the forced vital capacity exhaled in the first second....
(FEV1%) is the ratio of FEV1 to FVC. In healthy adults this should be approximately 75–80%. In obstructive diseases (asthma, COPD, chronic bronchitis, emphysema) FEV1 is diminished because of increased airway resistance to expiratory flow; the FVC may be decreased as well, due to the premature closure of airway in expiration, just not in the same proportion as FEV1 (for instance, both FEV1 and FVC are reduced, but the former is more affected because of the increased airway resistance). This generates a reduced value (<80%, often ~45%). In restrictive diseases (such as pulmonary fibrosis
Pulmonary fibrosis
Pulmonary fibrosis is the formation or development of excess fibrous connective tissue in the lungs. It is also described as "scarring of the lung".-Symptoms:Symptoms of pulmonary fibrosis are mainly:...
) the FEV1 and FVC are both reduced proportionally and the value may be normal or even increased as a result of decreased lung compliance.
A derived value of FEV1% is FEV1% predicted, which is defined as FEV1% of the patient divided by the average FEV1% in the population for any person of similar age, sex and body composition.
Forced expiratory flow (FEF)
Forced expiratory flow (FEF) is the flow (or speed) of air coming out of the lung during the middle portion of a forced expiration. It can be given at discrete timeDiscrete time
Discrete time is the discontinuity of a function's time domain that results from sampling a variable at a finite interval. For example, consider a newspaper that reports the price of crude oil once every day at 6:00AM. The newspaper is described as sampling the cost at a frequency of once per 24...
s, generally defined by what fraction remains of the forced vital capacity (FVC). The usual intervals are 25%, 50% and 75% (FEF25, FEF50 and FEF75), or 25% and 50% of FVC. It can also be given as a mean of the flow during an interval, also generally delimited by when specific fractions remain of FVC, usually 25–75% (FEF25–75%). Average ranges in the healthy population depend mainly on sex and age, with FEF25–75% shown in diagram at left. Values ranging from 50-60% and up to 130% of the average are considered normal. Predicted normal values for FEF can be calculated online and depend on age, sex, height, weight and ethnicity as well as the research study that they are based upon.
MMEF or MEF stands for maximal (mid-)expiratory flow and is the peak of expiratory flow as taken from the flow-volume curve and measured in liters per second. It should theoretically be identical to peak expiratory flow (PEF), which is, however, generally measured by a peak flow meter and given in liters per minute.
Recent research suggests that FEF25-75% or FEF25-50% may be a more sensitive parameter than FEV1 in the detection of obstructive small airway disease. However, in the absence of concomitant changes in the standard markers, discrepancies in mid-range expiratory flow may not be specific enough to be useful, and current practice guidelines recommend continuing to use FEV1, VC, and FEV1/VC as indicators of obstructive disease.
More rarely, forced expiratory flow may be given at intervals defined by how much remains of total lung capacity. In such cases, it is usually designated as e.g. FEF70%TLC, FEF60%TLC and FEF50%TLC.
Forced inspiratory flow 25–75% or 25–50%
Forced inspiratory flow 25–75% or 25–50% (FIF 25–75% or 25–50%) is similar to FEF 25–75% or 25–50% except the measurement is taken during inspiration.Peak expiratory flow (PEF)
Peak expiratory flow (PEF) is the maximal flow (or speed) achieved during the maximally forced expiration initiated at full expiration, measured in liters per minute.Tidal volume (TV)
Tidal volumeTidal volume
Tidal volume is the lung volume representing the normal volume of air displaced between normal inspiration and expiration when extra effort is not applied.Typical values are around 500ml or 7ml/kg bodyweight.-Mechanical Ventilation:...
(TV) is the volume of air inspired or expired in a single breath at rest.
Total lung capacity (TLC)
Total lung capacity (TLC) is the maximum volume of air present in the lungsDiffusion capacity (DLCO)
Diffusing capacity (DLCODLCO
DLCO is the extent to which oxygen passes from the air sacs of the lungs into the blood. Commonly, it refers to the test used to determine this parameter. It was introduced in 1909....
)is the carbon monoxide uptake from a single inspiration in a standard time (usually 10 sec). Since air consists of very minute or trace quantities of CO, 10 seconds is considered to be the standard time for inhalation, then rapidly blow it out (exhale). The exhaled gas is tested to determine how much of the tracer gas was absorbed during the breath. This will pick up diffusion impairments, for instance in pulmonary fibrosis. This must be corrected for anemia (because rapid CO diffusion is dependent on hemoglobin in RBC's; a low hemoglobin concentration, anemia, will reduce DLCO) and pulmonary hemorrhage (excess RBC's in the interstitium or alveoli can absorb CO and artificially increase the DLCO capacity). Atmospheric pressure and/or altitude will also affect measured DLCO, and so a correction factor is needed to adjust for standard pressure. Online calculators are available to correct for hemoglobin levels and altitude and/or pressure where the measurement was taken.
Maximum voluntary ventilation (MVV)
Maximum voluntary ventilation (MVV) is a measure of the maximum amount of air that can be inhaled and exhaled within one minute. For the comfort of the patient this is done over a 15 second time period before being extrapolated to a value for one minute expressed as liters/minute. Average values for males and females are 140–180 and 80–120 liters per minute respectively.Static lung compliance (Cst)
When estimating static lung compliance, volume measurements by the spirometer needs to be complemented by pressure transducers in order to simultaneously measure the transpulmonary pressureTranspulmonary pressure
Transpulmonary pressure is a term used to describe the difference between the alveolar pressure and the intrapleural pressure in the lungs. During human ventilation, air flows because of pressure gradients.Ptp = Palv - Pip...
. When having drawn a curve with the relations between changes in volume to changes in transpulmonary pressure, Cst is the slope of the curve during any given volume, or, mathematically, ΔV/ΔP. Static lung compliance is perhaps the most sensitive parameter for the detection of abnormal pulmonary mechanics. It is considered normal if it is 60% to 140% of the average value in the population for any person of similar age, sex and body composition.
In those with acute respiratory failure on mechanical ventilation, "the static compliance of the total respiratory system is conventionally obtained by dividing the tidal volume by the difference between the "plateau" pressure measured at the airway opening (PaO) during an occlusion at end-inspiration and positive end-expiratory pressure (PEEP) set by the ventilator".
Others
Forced Expiratory Time (FET)Forced Expiratory Time (FET) measures the length of the expiration in seconds.
Slow vital capacity (SVC)
Slow vital capacity
Vital capacity
Vital capacity is the maximum amount of air a person can expel from the lungs after a maximum inspiration. It is equal to the inspiratory reserve volume plus the tidal volume plus the expiratory reserve volume....
(SVC) is the maximum volume of air that can be exhaled slowly after slow maximum inhalation.
Maximal pressure (Pmax and Pi)
Pmax is the asymptotically maximal pressure that can be developed by the respiratory muscles at any lung volume and Pi is the maximum inspiratory pressure that can be developed at specific lung volumes. This measurement also requires pressure transducers in addition. It is considered normal if it is 60% to 140% of the average value in the population for any person of similar age, sex and body composition. A derived parameter is the coefficient of retraction (CR) which is Pmax/TLC .
Mean transit time (MTT)
Mean transit time is the area under the flow-volume curve divided by the forced vital capacity.
Technologies used in spirometers
- Volumetric Spirometers
- Water bell
- BellowsBellowsA bellows is a device for delivering pressurized air in a controlled quantity to a controlled location.Basically, a bellows is a deformable container which has an outlet nozzle. When the volume of the bellows is decreased, the air escapes through the outlet...
wedge
- Flow measuring Spirometers
- Fleisch-pneumotach
- Lilly (screen) pneumotach
- TurbineTurbineA turbine is a rotary engine that extracts energy from a fluid flow and converts it into useful work.The simplest turbines have one moving part, a rotor assembly, which is a shaft or drum with blades attached. Moving fluid acts on the blades, or the blades react to the flow, so that they move and...
(actually a rotating vane which spins because of the air flow generated by the subject. The revolutions of the vane are counted as they break a light beam) - Pitot tubePitot tubeA pitot tube is a pressure measurement instrument used to measure fluid flow velocity. The pitot tube was invented by the French engineer Henri Pitot Ulo in the early 18th century and was modified to its modern form in the mid-19th century by French scientist Henry Darcy...
- Hot-wire anemometerAnemometerAn anemometer is a device for measuring wind speed, and is a common weather station instrument. The term is derived from the Greek word anemos, meaning wind, and is used to describe any airspeed measurement instrument used in meteorology or aerodynamics...
- UltrasoundUltrasoundUltrasound is cyclic sound pressure with a frequency greater than the upper limit of human hearing. Ultrasound is thus not separated from "normal" sound based on differences in physical properties, only the fact that humans cannot hear it. Although this limit varies from person to person, it is...

