
Hemodialysis
Encyclopedia


Medicine
Medicine is the science and art of healing. It encompasses a variety of health care practices evolved to maintain and restore health by the prevention and treatment of illness....
, hemodialysis (also haemodialysis) is a method for removing waste products such as creatinine
Creatinine
Creatinine is a break-down product of creatine phosphate in muscle, and is usually produced at a fairly constant rate by the body...
and urea
Urea
Urea or carbamide is an organic compound with the chemical formula CO2. The molecule has two —NH2 groups joined by a carbonyl functional group....
, as well as free water from the blood
Blood
Blood is a specialized bodily fluid in animals that delivers necessary substances such as nutrients and oxygen to the cells and transports metabolic waste products away from those same cells....
when the kidney
Kidney
The kidneys, organs with several functions, serve essential regulatory roles in most animals, including vertebrates and some invertebrates. They are essential in the urinary system and also serve homeostatic functions such as the regulation of electrolytes, maintenance of acid–base balance, and...
s are in renal failure
Renal failure
Renal failure or kidney failure describes a medical condition in which the kidneys fail to adequately filter toxins and waste products from the blood...
. Hemodialysis is one of three renal replacement therapies
Renal replacement therapy
Renal replacement therapy is a term used to encompass life-supporting treatments for renal failure.It includes:*hemodialysis,*peritoneal dialysis,*hemofiltration and*renal transplantation.These treatments will not cure chronic kidney disease...
(the other two being renal transplant; peritoneal dialysis
Peritoneal dialysis
Peritoneal dialysis is a treatment for patients with severe chronic kidney disease. The process uses the patient's peritoneum in the abdomen as a membrane across which fluids and dissolved substances are exchanged from the blood...
).
Hemodialysis can be an outpatient or inpatient therapy. Routine hemodialysis is conducted in a dialysis outpatient facility, either a purpose built room in a hospital
Hospital
A hospital is a health care institution providing patient treatment by specialized staff and equipment. Hospitals often, but not always, provide for inpatient care or longer-term patient stays....
or a dedicated, stand alone clinic. Less frequently hemodialysis is done at home
Home hemodialysis
Home hemodialysis , is the provision of hemodialysis in the home of people with stage 5 chronic kidney disease. In the US home hemodialysis was the most common method of renal replacement therapy in the early 1970s before the introduction of the Federal ESRD program under Medicare...
. Dialysis treatments in a clinic are initiated and managed by specialized staff made up of nurses and technicians; dialysis treatments at home can be self initiated and managed or done jointly with the assistance of a trained helper who is usually a family member.
Principle

Dialysis
In medicine, dialysis is a process for removing waste and excess water from the blood, and is primarily used to provide an artificial replacement for lost kidney function in people with renal failure...
; it involves diffusion
Diffusion
Molecular diffusion, often called simply diffusion, is the thermal motion of all particles at temperatures above absolute zero. The rate of this movement is a function of temperature, viscosity of the fluid and the size of the particles...
of solutes across a semipermeable membrane. Hemodialysis utilizes counter current flow, where the dialysate is flowing in the opposite direction to blood flow
Blood flow
Blood flow is the continuous running of blood in the cardiovascular system.The human body is made up of several processes all carrying out various functions. We have the gastrointestinal system which aids the digestion and the absorption of food...
in the extracorporeal
Extracorporeal
An extracorporeal medical procedure is a medical procedure which is performed outside the body.-Circulatory procedures:A procedure in which blood is taken from a patient's circulation to have a process applied to it before it is returned to the circulation...
circuit. Counter-current flow maintains the concentration gradient across the membrane at a maximum and increases the efficiency of the dialysis.
Fluid removal (ultrafiltration
Ultrafiltration (renal)
In biological terms, ultrafiltration occurs at the barrier between the blood and the filtrate in the renal corpuscle or Bowman's capsule in the kidneys. The Bowman's capsule contains a dense capillary network called the glomerulus. Blood flows into these capillaries through a wide afferent...
) is achieved by altering the hydrostatic pressure of the dialysate compartment, causing free water and some dissolved solutes to move across the membrane along a created pressure gradient.
The dialysis solution that is used may be a sterilized solution of mineral ions or comply with British Pharmacopoeia
British Pharmacopoeia
The British Pharmacopoeia is an annual published collection of quality standards for UK medicinal substances. It is used by individuals and organizations involved in pharmaceutical research, development, manufacture and testing....
. Urea
Urea
Urea or carbamide is an organic compound with the chemical formula CO2. The molecule has two —NH2 groups joined by a carbonyl functional group....
and other waste products, potassium
Potassium
Potassium is the chemical element with the symbol K and atomic number 19. Elemental potassium is a soft silvery-white alkali metal that oxidizes rapidly in air and is very reactive with water, generating sufficient heat to ignite the hydrogen emitted in the reaction.Potassium and sodium are...
, and phosphate
Phosphate
A phosphate, an inorganic chemical, is a salt of phosphoric acid. In organic chemistry, a phosphate, or organophosphate, is an ester of phosphoric acid. Organic phosphates are important in biochemistry and biogeochemistry or ecology. Inorganic phosphates are mined to obtain phosphorus for use in...
diffuse into the dialysis solution. However, concentrations of sodium
Sodium
Sodium is a chemical element with the symbol Na and atomic number 11. It is a soft, silvery-white, highly reactive metal and is a member of the alkali metals; its only stable isotope is 23Na. It is an abundant element that exists in numerous minerals, most commonly as sodium chloride...
and chloride are similar to those of normal plasma
Blood plasma
Blood plasma is the straw-colored liquid component of blood in which the blood cells in whole blood are normally suspended. It makes up about 55% of the total blood volume. It is the intravascular fluid part of extracellular fluid...
to prevent loss. Sodium bicarbonate
Sodium bicarbonate
Sodium bicarbonate or sodium hydrogen carbonate is the chemical compound with the formula Na HCO3. Sodium bicarbonate is a white solid that is crystalline but often appears as a fine powder. It has a slightly salty, alkaline taste resembling that of washing soda . The natural mineral form is...
is added in a higher concentration than plasma to correct blood acidity. A small amount of glucose is also commonly used.
Note that this is a different process to the related technique of hemofiltration
Hemofiltration
In medicine, hemofiltration, also haemofiltration, is a renal replacement therapy similar to hemodialysis which is used almost exclusively in the intensive care setting...
.
History
Many have played a role in developing dialysis as a practical treatment for renal failure, starting with Thomas GrahamThomas Graham (chemist)
Thomas Graham FRS was a nineteenth-century Scottish chemist who is best-remembered today for his pioneering work in dialysis and the diffusion of gases.- Life and work :...
of Glasgow
Glasgow
Glasgow is the largest city in Scotland and third most populous in the United Kingdom. The city is situated on the River Clyde in the country's west central lowlands...
, who first presented the principles of solute transport across a semipermeable membrane in 1854. The artificial kidney was first developed by Abel
John Jacob Abel
John Jacob Abel was a significant American biochemist and pharmacologist.Born near Cleveland, Ohio, he graduated with a Ph.D. in 1883 from the University of Michigan. In 1891 he founded and chaired the first department of pharmacology in the United States at the University of Michigan...
, Rountree and Turner in 1913, the first hemodialysis in a human being was by Hass
Georg Haas
George Haas a German medical doctor was born in Nuremberg, Germany. Haas performed the first human hemodialysis treatment. Haas studied medicine at the Universities of Munich and Freiburg...
(February 28, 1924) and the artificial kidney was developed into a clinically useful apparatus by Kolff
Willem Johan Kolff
Willem Johan "Pim" Kolff was a pioneer of hemodialysis as well as in the field of artificial organs. Willem is a member of the Kolff family, an old Dutch patrician family. He made his major discoveries in the field of dialysis for kidney failure during the Second World War...
in 1943 - 1945. This research showed that life could be prolonged in patients dying of renal failure
Renal failure
Renal failure or kidney failure describes a medical condition in which the kidneys fail to adequately filter toxins and waste products from the blood...
.
Dr. Willem Kolff was the first to construct a working dialyzer in 1943. The first successfully treated patient was a 67-year-old woman in uremic coma
Uremia
Uremia or uraemia is a term used to loosely describe the illness accompanying kidney failure , in particular the nitrogenous waste products associated with the failure of this organ....
who regained consciousness after 11 hours of hemodialysis with Kolff’s dialyzer in 1945. At the time of its creation, Kolff’s goal was to provide life support during recovery from acute renal failure. After World War II
World War II
World War II, or the Second World War , was a global conflict lasting from 1939 to 1945, involving most of the world's nations—including all of the great powers—eventually forming two opposing military alliances: the Allies and the Axis...
ended, Kolff donated the five dialyzers he had made to hospitals around the world, including Mount Sinai Hospital, New York
Mount Sinai Hospital, New York
Mount Sinai Hospital, founded in 1852, is one of the oldest and largest teaching hospitals in the United States. In 2011-2012, Mount Sinai Hospital was ranked as one of America's best hospitals by U.S...
. Kolff gave a set of blueprints for his hemodialysis machine to George Thorn at the Peter Bent Brigham Hospital in Boston
Boston
Boston is the capital of and largest city in Massachusetts, and is one of the oldest cities in the United States. The largest city in New England, Boston is regarded as the unofficial "Capital of New England" for its economic and cultural impact on the entire New England region. The city proper had...
. This led to the manufacture of the next generation of Kolff’s dialyzer, a stainless steel
Stainless steel
In metallurgy, stainless steel, also known as inox steel or inox from French "inoxydable", is defined as a steel alloy with a minimum of 10.5 or 11% chromium content by mass....
Kolff-Brigham dialysis machine.
By the 1950s, Willem Kolff’s invention of the dialyzer was used for acute renal failure, but it was not seen as a viable treatment for patients with stage 5 chronic kidney disease (CKD). At the time, doctors believed it was impossible for patients to have dialysis indefinitely for two reasons. First, they thought no man-made device could replace the function of kidneys over the long term. In addition, a patient undergoing dialysis suffered from damaged veins and arteries, so that after several treatments, it became difficult to find a vessel to access the patient’s blood.
Dr. Nils Alwall
Nils Alwall
Nils Alwall , a Swedish professor, was a pioneer in hemodialysis and the inventor of one of the first practical dialysis machines. Alwall pioneered the technique of ultrafiltration and introduced the principle of hemofiltration...
: The original Kolff kidney was not very useful clinically, because it did not allow for removal of excess fluid. Dr. Nils Alwall encased a modified version of this kidney inside a stainless steel canister, to which a negative pressure could be applied, in this way effecting the first truly practical application of hemodialysis, which was done in 1946 at the University of Lund. Alwall also was arguably the inventor of the arteriovenous shunt for dialysis. He reported this first in 1948 where he used such an arteriovenous shunt in rabbits. Subsequently he used such shunts, made of glass, as well as his canister-enclosed dialyzer, to treat 1500 patients in renal failure between 1946 and 1960, as reported to the First International Congress of Nephrology held in Evian in September 1960. Alwall was appointed to a newly-created Chair of Nephrology at the University of Lund in 1957. Subsequently, he collaborated with Swedish businessman Holger Crafoord
Holger Crafoord
Holger Crafoord was a Swedish industrialist and founded Gambro along with Nils Alwall, a company that would commercialize Alwall's research into artificial kidneys. He donated the initial funds for the establishment of the Crafoord Prize for scientific research.-See also:*Lund School of Economics...
to found one of the key companies that would manufacture dialysis equipment in the past 50 years, Gambro
Gambro
Gambro is a global medical technology companythat manufactures products for Dialysis treatment.The company is a global leader in developing, manufacturing andsupplying products and therapies for Kidneyand Liver Dialysis, Myeloma Kidney Therapy, and other...
. The early history of dialysis has been reviewed by Stanley Shaldon.
Dr. Belding H. Scribner
Belding H. Scribner
Belding Hibbard Scribner was a U.S. physician and a pioneer in kidney dialysis.-Biography:Scribner received his medical degree from Stanford University in 1945. After completing his postgraduate studies at the Mayo Clinic in Rochester, Minnesota, he joined the faculty of the School of Medicine at...
working with a surgeon, Dr. Wayne Quinton, modified the glass shunts used by Alwall by making them from Teflon
Polytetrafluoroethylene
Polytetrafluoroethylene is a synthetic fluoropolymer of tetrafluoroethylene that finds numerous applications. PTFE is most well known by the DuPont brand name Teflon....
. Another key improvement was to connect them to a short piece of silicone elastomer tubing. This formed the basis of the so-called Scribner shunt, perhaps more properly called the Quinton-Scribner shunt. After treatment, the circulatory access would be kept open by connecting the two tubes outside the body using a small U-shaped Teflon tube, which would shunt the blood from the tube in the artery back to the tube in the vein.
In 1962, Scribner started the world’s first outpatient dialysis facility, the Seattle Artificial Kidney Center, later renamed the Northwest Kidney Centers
Northwest Kidney Centers
The Northwest Kidney Centers in Seattle Washington was established in 1962 as the first out-of-hospital outpatient hemodialysis treatment center. The model of providing hemodialysis outside of a hospital setting has spread throughout the world...
. Immediately the problem arose of who should be given dialysis, since demand far exceeded the capacity of the six dialysis machines at the center. Scribner decided that the decision about who would receive dialysis and who wouldn’t, would not be made by him. Instead, the choices would be made by an anonymous committee, which could be viewed as one of the first bioethics
Bioethics
Bioethics is the study of controversial ethics brought about by advances in biology and medicine. Bioethicists are concerned with the ethical questions that arise in the relationships among life sciences, biotechnology, medicine, politics, law, and philosophy....
committees.
For a detailed history of successful and unsuccessful attempts at dialysis, including pioneers such as Abel and Roundtree, Haas, and Necheles, see this review by Kjellstrand.
Prescription
A prescription for dialysis by a nephrologist (a medical kidney specialist) will specify various parameters for a dialysis treatment. These include frequency (how many treatments per week), length of each treatment, and the blood and dialysis solution flow rates, as well as the size of the dialyzer. The composition of the dialysis solution is also sometimes adjusted in terms of its sodium and potassium and bicarbonate levels. In general, the larger the body size of an individual, the more dialysis he/she will need. In North AmericaNorth America
North America is a continent wholly within the Northern Hemisphere and almost wholly within the Western Hemisphere. It is also considered a northern subcontinent of the Americas...
and the UK
United Kingdom
The United Kingdom of Great Britain and Northern IrelandIn the United Kingdom and Dependencies, other languages have been officially recognised as legitimate autochthonous languages under the European Charter for Regional or Minority Languages...
, 3-4 hour treatments (sometimes up to 5 hours for larger patients) given 3 times a week are typical. Twice-a-week sessions are limited to patients who have a substantial residual kidney function. Four sessions per week are often prescribed for larger patients, as well as patients who have trouble with fluid overload. Finally, there is growing interest in short daily home hemodialysis
Home hemodialysis
Home hemodialysis , is the provision of hemodialysis in the home of people with stage 5 chronic kidney disease. In the US home hemodialysis was the most common method of renal replacement therapy in the early 1970s before the introduction of the Federal ESRD program under Medicare...
, which is 1.5 - 4 hr sessions given 5-7 times per week, usually at home. There also is interest in nocturnal dialysis
Nocturnal dialysis
In medicine, nocturnal dialysis, refers to dialysis done at night. It usually is a reference to nocturnal hemodialysis, but could also refer to peritoneal dialysis which is typically done at night....
, which involves dialyzing a patient, usually at home, for 8–10 hours per night, 3-6 nights per week. Nocturnal in-center dialysis, 3-4 times per week, is also offered at a handful of dialysis units in the United States
United States
The United States of America is a federal constitutional republic comprising fifty states and a federal district...
.
Side effects and complications
Hemodialysis often involves fluid removal (through ultrafiltrationUltrafiltration (renal)
In biological terms, ultrafiltration occurs at the barrier between the blood and the filtrate in the renal corpuscle or Bowman's capsule in the kidneys. The Bowman's capsule contains a dense capillary network called the glomerulus. Blood flows into these capillaries through a wide afferent...
), because most patients with renal failure
Renal failure
Renal failure or kidney failure describes a medical condition in which the kidneys fail to adequately filter toxins and waste products from the blood...
pass little or no urine. Side effects caused by removing too much fluid and/or removing fluid too rapidly include low blood pressure
Blood pressure
Blood pressure is the pressure exerted by circulating blood upon the walls of blood vessels, and is one of the principal vital signs. When used without further specification, "blood pressure" usually refers to the arterial pressure of the systemic circulation. During each heartbeat, BP varies...
, fatigue
Fatigue (physical)
Fatigue is a state of awareness describing a range of afflictions, usually associated with physical and/or mental weakness, though varying from a general state of lethargy to a specific work-induced burning sensation within one's muscles...
, chest pains, leg-cramps, nausea
Nausea
Nausea , is a sensation of unease and discomfort in the upper stomach with an involuntary urge to vomit. It often, but not always, precedes vomiting...
and headaches. These symptoms can occur during the treatment and can persist post treatment; they are sometimes collectively referred to as the dialysis hangover or dialysis washout. The severity of these symptoms is usually proportionate to the amount and speed of fluid removal. However, the impact of a given amount or rate of fluid removal can vary greatly from person to person and day to day. These side effects can be avoided and/or their severity lessened by limiting fluid intake between treatments or increasing the dose of dialysis e.g. dialyzing more often or longer per treatment than the standard three times a week, 3–4 hours per treatment schedule.
Since hemodialysis requires access to the circulatory system, patients undergoing hemodialysis may expose their circulatory system to microbes, which can lead to sepsis
Sepsis
Sepsis is a potentially deadly medical condition that is characterized by a whole-body inflammatory state and the presence of a known or suspected infection. The body may develop this inflammatory response by the immune system to microbes in the blood, urine, lungs, skin, or other tissues...
, an infection affecting the heart valves (endocarditis
Endocarditis
Endocarditis is an inflammation of the inner layer of the heart, the endocardium. It usually involves the heart valves . Other structures that may be involved include the interventricular septum, the chordae tendineae, the mural endocardium, or even on intracardiac devices...
) or an infection affecting the bones (osteomyelitis
Osteomyelitis
Osteomyelitis simply means an infection of the bone or bone marrow...
). The risk of infection varies depending on the type of access used (see below). Bleeding may also occur, again the risk varies depending on the type of access used. Infections can be minimized by strictly adhering to infection control
Infection control
Infection control is the discipline concerned with preventing nosocomial or healthcare-associated infection, a practical sub-discipline of epidemiology. It is an essential, though often under-recognized and under-supported, part of the infrastructure of health care...
best practices.
Heparin
Heparin
Heparin , also known as unfractionated heparin, a highly sulfated glycosaminoglycan, is widely used as an injectable anticoagulant, and has the highest negative charge density of any known biological molecule...
is the most commonly used anticoagulant in hemodialysis, as it is generally well tolerated and can be quickly reversed with protamine sulfate
Protamine sulfate
Protamine sulfate is a drug that reverses the anticoagulant effects of heparin by binding to it.Protamine was originally isolated from the sperm of salmon and other species of fish but is now produced primarily through recombinant biotechnology. It is a highly cationic peptide...
. Heparin allergy can infrequently be a problem and can cause a low platelet count. In such patients, alternative anticoagulants can be used. In patients at high risk of bleeding, dialysis can be done without anticoagulation.
First Use Syndrome is a rare but severe anaphylactic reaction
Anaphylaxis
Anaphylaxis is defined as "a serious allergic reaction that is rapid in onset and may cause death". It typically results in a number of symptoms including throat swelling, an itchy rash, and low blood pressure...
to the artificial kidney
Artificial kidney
Artificial kidney is often a synonym for hemodialysis, but may also, more generally, refer to renal replacement therapies that are in use and/or in development...
. Its symptoms include sneezing, wheezing, shortness of breath, back pain, chest pain, or sudden death. It can be caused by residual sterilant in the artificial kidney or the material of the membrane itself. In recent years, the incidence of First Use Syndrome has decreased, due to an increased use of gamma irradiation, steam sterilization, or electron-beam radiation instead of chemical sterilants, and the development of new semipermeable membranes of higher biocompatibility
Biocompatibility
Biocompatibility is related to the behavior of biomaterials in various contexts. The term may refer to specific properties of a material without specifying where or how the material is used , or to more empirical clinical success of a whole device in...
. New methods of processing previously acceptable components of dialysis must always be considered. For example, in 2008, a series of first-use type or reactions, including deaths occurred due to heparin contaminated during the manufacturing process with oversulfated chondroitin sulfate
Chondroitin sulfate
Chondroitin sulfate is a sulfated glycosaminoglycan composed of a chain of alternating sugars . It is usually found attached to proteins as part of a proteoglycan. A chondroitin chain can have over 100 individual sugars, each of which can be sulfated in variable positions and quantities...
.
Longterm complications of hemodialysis include amyloidosis
Amyloidosis
In medicine, amyloidosis refers to a variety of conditions whereby the body produces "bad proteins", denoted as amyloid proteins, which are abnormally deposited in organs and/or tissues and cause harm. A protein is described as being amyloid if, due to an alteration in its secondary structure, it...
, neuropathy and various forms of heart disease
Heart disease
Heart disease, cardiac disease or cardiopathy is an umbrella term for a variety of diseases affecting the heart. , it is the leading cause of death in the United States, England, Canada and Wales, accounting for 25.4% of the total deaths in the United States.-Types:-Coronary heart disease:Coronary...
. Increasing the frequency and length of treatments have been shown to improve fluid overload and enlargement of the heart that is commonly seen in such patients.
Listed below are specific complications associated with different types of hemodialysis access.
Access
In hemodialysis, three primary methods are used to gain access to the blood: an intravenous catheter, an arteriovenous fistulaArteriovenous fistula
An arteriovenous fistula is an abnormal connection or passageway between an artery and a vein. It may be congenital, surgically created for hemodialysis treatments, or acquired due to pathologic process, such as trauma or erosion of an arterial aneurysm....
(AV) and a synthetic graft. The type of access is influenced by factors such as the expected time course of a patient's renal failure and the condition of his or her vasculature. Patients may have multiple accesses, usually because an AV fistula or graft is maturing and a catheter is still being used. The creation of all these three major types of vascular accesses requires surgery.
Catheter
Catheter access, sometimes called a CVC (Central Venous CatheterCentral venous catheter
In medicine, a central venous catheter is a catheter placed into a large vein in the neck , chest or groin...
), consists of a plastic catheter with two lumens (or occasionally two separate catheters) which is inserted into a large vein (usually the vena cava, via the internal jugular vein
Internal jugular vein
The two internal jugular veins collect the blood from the brain, the superficial parts of the face, and the neck.-Path:On both sides and at the base of the brain, the inferior petrosal sinus and the sigmoid sinus join to form the internal jugular vein...
or the femoral vein
Femoral vein
In the human body, the femoral vein is a blood vessel that accompanies the femoral artery in the femoral sheath. It begins at the adductor canal and is a continuation of the popliteal vein...
) to allow large flows of blood to be withdrawn from one lumen, to enter the dialysis circuit, and to be returned via the other lumen. However, blood flow is almost always less than that of a well functioning fistula or graft.
Catheters are usually found in two general varieties, tunnelled and non-tunnelled.
Non-tunnelled catheter access is for short-term access (up to about 10 days, but often for one dialysis session only), and the catheter emerges from the skin at the site of entry into the vein.
Tunnelled catheter access involves a longer catheter, which is tunnelled under the skin from the point of insertion in the vein to an exit site some distance away. It is usually placed in the internal jugular vein in the neck and the exit site is usually on the chest wall. The tunnel acts as a barrier to invading microbes, and as such, tunnelled catheters are designed for short- to medium-term access (weeks to months only), because infection is still a frequent problem.
Aside from infection, venous stenosis
Stenosis
A stenosis is an abnormal narrowing in a blood vessel or other tubular organ or structure.It is also sometimes called a stricture ....
is another serious problem with catheter access. The catheter is a foreign body in the vein and often provokes an inflammatory reaction in the vein wall. This results in scarring and narrowing of the vein, often to the point of occlusion. This can cause problems with severe venous congestion in the area drained by the vein and may also render the vein, and the veins drained by it, useless for creating a fistula or graft at a later date. Patients on long-term hemodialysis can literally 'run out' of access, so this can be a fatal problem.
Catheter access is usually used for rapid access for immediate dialysis, for tunnelled access in patients who are deemed likely to recover from acute renal failure
Acute renal failure
Acute kidney injury , previously called acute renal failure , is a rapid loss of kidney function. Its causes are numerous and include low blood volume from any cause, exposure to substances harmful to the kidney, and obstruction of the urinary tract...
, and for patients with end-stage renal failure who are either waiting for alternative access to mature or who are unable to have alternative access.
Catheter access is often popular with patients, because attachment to the dialysis machine doesn't require needles. However, the serious risks of catheter access noted above mean that such access should be contemplated only as a long-term solution in the most desperate access situation.
AV fistula
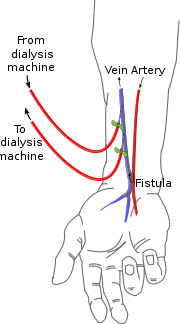
AV (arteriovenous) fistulas are recognized as the preferred access method. To create a fistula
Fistula
In medicine, a fistula is an abnormal connection or passageway between two epithelium-lined organs or vessels that normally do not connect. It is generally a disease condition, but a fistula may be surgically created for therapeutic reasons.-Locations:Fistulas can develop in various parts of the...
, a vascular surgeon joins an artery
Artery
Arteries are blood vessels that carry blood away from the heart. This blood is normally oxygenated, exceptions made for the pulmonary and umbilical arteries....
and a vein
Vein
In the circulatory system, veins are blood vessels that carry blood towards the heart. Most veins carry deoxygenated blood from the tissues back to the heart; exceptions are the pulmonary and umbilical veins, both of which carry oxygenated blood to the heart...
together through anastomosis
Anastomosis
An anastomosis is the reconnection of two streams that previously branched out, such as blood vessels or leaf veins. The term is used in medicine, biology, mycology and geology....
. Since this bypasses the capillaries, blood flows rapidly through the fistula. One can feel this by placing one's finger over a mature fistula. This is called feeling for "thrill" and produces a distinct 'buzzing' feeling over the fistula. One can also listen through a stethoscope
Stethoscope
The stethoscope is an acoustic medical device for auscultation, or listening to the internal sounds of an animal body. It is often used to listen to lung and heart sounds. It is also used to listen to intestines and blood flow in arteries and veins...
for the sound of the blood "whooshing" through the fistula, a sound called bruit
Bruit
Bruit is the term for the unusual sound that blood makes when it rushes past an obstruction in an artery when the sound is auscultated with the bell portion of a stethoscope.The term "bruit" simply refers to the sound...
.
Fistulas are usually created in the nondominant arm and may be situated on the hand (the 'snuffbox' fistula'), the forearm (usually a radiocephalic fistula, or so-called Brescia-Cimino fistula
Cimino fistula
A Cimino fistula, also Cimino-Brescia fistula, surgically created arteriovenous fistula and arteriovenous fistula , is a type of vascular access for hemodialysis...
, in which the radial artery
Radial artery
In human anatomy, the radial artery is the main blood vessel, with oxygenated blood, of the lateral aspect of the forearm.-Course:The radial artery arises from the bifurcation of the brachial artery in the cubital fossa. It runs distally on the anterior part of the forearm...
is anastomosed to the cephalic vein
Cephalic vein
In human anatomy, the cephalic vein is a superficial vein of the upper limb.It communicates with the basilic vein via the median cubital vein at the elbow and is located in the superficial fascia along the anterolateral surface of the biceps brachii muscle.Superiorly the cephalic vein passes...
), or the elbow (usually a brachiocephalic fistula, where the brachial artery
Brachial artery
The brachial artery is the major blood vessel of the arm.It is the continuation of the axillary artery beyond the lower margin of teres major muscle. It continues down the ventral surface of the arm until it reaches the cubital fossa at the elbow. It then divides into the radial and ulnar arteries...
is anastomosed to the cephalic vein
Cephalic vein
In human anatomy, the cephalic vein is a superficial vein of the upper limb.It communicates with the basilic vein via the median cubital vein at the elbow and is located in the superficial fascia along the anterolateral surface of the biceps brachii muscle.Superiorly the cephalic vein passes...
). A fistula will take a number of weeks to mature, on average perhaps 4–6 weeks. During treatment, two needles are inserted into the fistula, one to draw blood and one to return it.
The advantages of the AV fistula use are lower infection rates, because no foreign material is involved in their formation, higher blood flow rates (which translates to more effective dialysis), and a lower incidence of thrombosis
Thrombosis
Thrombosis is the formation of a blood clot inside a blood vessel, obstructing the flow of blood through the circulatory system. When a blood vessel is injured, the body uses platelets and fibrin to form a blood clot to prevent blood loss...
. The complications are few, but if a fistula has a very high blood flow and the vasculature that supplies the rest of the limb is poor, a steal syndrome
Vascular access steal syndrome
In nephrology, vascular access steal syndrome or Dialysis-associated Steal Syndrome , also known less precisely as steal syndrome, refers to vascular insufficiency resulting from an arteriovenous fistula or synthetic vascular graft-AV fistula)....
can occur, where blood entering the limb is drawn into the fistula and returned to the general circulation without entering the limb's capillaries. This results in cold extremities of that limb, cramping pains, and, if severe, tissue damage. One long-term complication of an AV fistula can be the development of an aneurysm, a bulging in the wall of the vein where it is weakened by the repeated insertion of needles over time. To a large extent the risk of developing an aneurysm can be reduced by carefully rotating needle sites over the entire fistula, or using the "buttonhole"(constant site) technique. Aneurysms may necessitate corrective surgery and may shorten the useful life of a fistula.
To prevent damage to the fistula and aneurysm or pseudoaneurysm formation, it is recommended that the needle be inserted at different points in a rotating fashion. Another approach is to cannulate the fistula with a blunted needle, in exactly the same place. This is called a 'buttonhole' approach. Often two or three buttonhole places are available on a given fistula. This also can prolong fistula life and help prevent damage to the fistula.
AV graft
.svg.png)
AV (arteriovenous) grafts are much like fistulas in most respects, except that an artificial vessel is used to join the artery and vein. The graft usually is made of a synthetic material, often PTFE
Polytetrafluoroethylene
Polytetrafluoroethylene is a synthetic fluoropolymer of tetrafluoroethylene that finds numerous applications. PTFE is most well known by the DuPont brand name Teflon....
, but sometimes chemically treated, sterilized veins from animals are used. Grafts are inserted when the patient's native vasculature does not permit a fistula. They mature faster than fistulas, and may be ready for use several weeks after formation (some newer grafts may be used even sooner). However, AV grafts are at high risk to develop narrowing, especially in the vein just downstream from where the graft has been sewn to the vein. Narrowing often leads to clotting or thrombosis. As foreign material, they are at greater risk for becoming infected. More options for sites to place a graft are available, because the graft can be made quite long. Thus a graft can be placed in the thigh or even the neck (the 'necklace graft').
Fistula First project
AV fistulas have a much better access patency and survival than do venous catheters or grafts. They also produce better patient survival and have far fewer complications compared to grafts or venous catheters. For this reason, the Centers for Medicare & Medicaid (CMS) has set up a Fistula First Initiative, whose goal is to increase the use of AV fistulas in dialysis patients.There is ongoing research to make bio-engineered blood vessels, which may be of immense importance in creating AV fistulas for patients on hemodialysis, who do not have good blood vessels for creation of one. It involves growing cells which produce collagen and other proteins on a biodegradable micromesh tube followed by removal of those cells to make the 'blood vessels' storable in refrigerators.
Types
There are three types of hemodialysis: conventional hemodialysis, daily hemodialysis, and nocturnal hemodialysis. Below is the adaption and summary from a brochure of The Ottawa Hospital.Conventional hemodialysis
Chronic hemodialysis is usually done three times per week, for about 3–4 hours for each treatment, during which the patient's blood is drawn out through a tube at a rate of 200-400 mL/min. The tube is connected to a 15, 16, or 17 gauge needle inserted in the dialysis fistula or graft, or connected to one port of a dialysis atheter] without needles]. The blood is then pumped through the dialyzer, and then the processed blood is pumped back into the patient's bloodstream through another tube (connected to a second needle or port). During the procedure, the patient's blood pressure is closely monitored, and if it becomes low, or the patient develops any other signs of low blood volume such as nausea, the dialysis attendant can administer extra fluid through the machine. During the treatment, the patient's entire blood volume (about 5000 cc) circulates through the machine every 15 minutes. During this process, the dialysis patient is exposed to a weeks worth of water for the average person.Daily hemodialysis
Daily hemodialysis is typically used by those patients who do their own dialysis at home. It is less stressful (more gentle) but does require more frequent access. This is simple with catheters, but more problematic with fistulas or grafts. The "buttonhole technique" can be used for fistulas requiring frequent access. Daily hemodialysis is usually done for 2 hours six days a week.Nocturnal hemodialysis
The procedure of nocturnal hemodialysis is similar to conventional hemodialysis except it is performed three to six nights a week and six-ten hours per session while the patient sleeps.Advantages
- Low mortality rate
- Better control of blood pressure and abdominal cramps
- Less diet restriction
- Better solute clearance effect for the daily hemodialysis: better tolerance and fewer complications with more frequent dialysis
Disadvantages
- Restricts independence, as people undergoing this procedure cannot travel around because of supplies’ availability
- Requires more supplies such as high water quality and electricity
- Requires reliable technology like dialysis machines
- The procedure is complicated and requires that care givers have more knowledge
- Requires time to set up and clean dialysis machines, and expense with machines and associated staff
Equipment

The hemodialysis machine pumps the patient's blood and the dialysate through the dialyzer. The newest dialysis machines on the market are highly computerized and continuously monitor an array of safety-critical parameters, including blood and dialysate flow rates; dialysis solution conductivity, temperature, and pH; and analysis of the dialysate for evidence of blood leakage or presence of air. Any reading that is out of normal range triggers an audible alarm to alert the patient-care technician who is monitoring the patient. Manufacturers of dialysis machines include companies such as Nipro, Fresenius
Fresenius AG
Fresenius SE & Co. KGaA is a globally diversified health care company based in Bad Homburg, Germany.The Fresenius Group provides products and services for dialysis, hospitals as well as inpatient and outpatient medical care...
, Gambro
Gambro
Gambro is a global medical technology companythat manufactures products for Dialysis treatment.The company is a global leader in developing, manufacturing andsupplying products and therapies for Kidneyand Liver Dialysis, Myeloma Kidney Therapy, and other...
, Baxter, B. Braun, NxStage and Bellco.
Water system

Water purification
Water purification is the process of removing undesirable chemicals, materials, and biological contaminants from contaminated water. The goal is to produce water fit for a specific purpose...
system is absolutely critical for hemodialysis. Since dialysis patients are exposed to vast quantities of water, which is mixed with dialysate concentrate to form the dialysate, even trace mineral contaminants or bacterial endotoxins can filter into the patient's blood. Because the damaged kidneys cannot perform their intended function of removing impurities, ions introduced into the bloodstream via water can build up to hazardous levels, causing numerous symptoms or death
Death
Death is the permanent termination of the biological functions that sustain a living organism. Phenomena which commonly bring about death include old age, predation, malnutrition, disease, and accidents or trauma resulting in terminal injury....
. Aluminum, chloramine, fluoride, copper, and zinc, as well as bacterial fragments and endotoxins, have all caused problems in this regard.
For this reason, water used in hemodialysis is carefully purified before use. Initially it is filtered and temperature-adjusted and its pH is corrected by adding an acid or base. Then it is softened. Next the water is run through a tank containing activated charcoal to adsorb organic contaminants. Primary purification is then done by forcing water through a membrane with very tiny pores, a so-called reverse osmosis
Reverse osmosis
Reverse osmosis is a membrane technical filtration method that removes many types of large molecules and ions from solutions by applying pressure to the solution when it is on one side of a selective membrane. The result is that the solute is retained on the pressurized side of the membrane and...
membrane. This lets the water pass, but holds back even very small solutes such as electrolytes. Final removal of leftover electrolytes is done by passing the water through a tank with ion-exchange resins, which remove any leftover anions or cations and replace them with hydroxyl and hydrogen molecules, respectively, leaving ultrapure water.
Even this degree of water purification may be insufficient. The trend lately is to pass this final purified water (after mixing with dialysate concentrate) through a dialyzer membrane. This provides another layer of protection by removing impurities, especially those of bacterial origin, that may have accumulated in the water after its passage through the original water purification system.
Once purified water is mixed with dialysate concentrate, its conductivity increases, since water that contains charged ions conducts electricity. During dialysis, the conductivity of dialysis solution is continuously monitored to ensure that the water and dialysate concentrate are being mixed in the proper proportions. Both excessively concentrated dialysis solution and excessively dilute solution can cause severe clinical problems.
Dialyzer
The dialyzer is the piece of equipment that actually filters the blood. Almost all dialyzers in use today are of the hollow-fiber variety. A cylindrical bundle of hollow fibers, whose walls are composed of semi-permeable membrane, is anchored at each end into potting compound (a sort of glue). This assembly is then put into a clear plastic cylindrical shell with four openings. One opening or blood port at each end of the cylinder communicates with each end of the bundle of hollow fibers. This forms the "blood compartment" of the dialyzer. Two other ports are cut into the side of the cylinder. These communicate with the space around the hollow fibers, the "dialysate compartment." Blood is pumped via the blood ports through this bundle of very thin capillaryCapillary
Capillaries are the smallest of a body's blood vessels and are parts of the microcirculation. They are only 1 cell thick. These microvessels, measuring 5-10 μm in diameter, connect arterioles and venules, and enable the exchange of water, oxygen, carbon dioxide, and many other nutrient and waste...
-like tubes, and the dialysate is pumped through the space surrounding the fibers. Pressure gradients are applied when necessary to move fluid from the blood to the dialysate compartment.
Membrane and flux
Dialyzer membranes come with different pore sizes. Those with smaller pore size are called "low-flux" and those with larger pore sizes are called "high-flux." Some larger molecules, such as beta-2-microglobulin, are not removed at all with low-flux dialyzers; lately, the trend has been to use high-flux dialyzers. However, such dialyzers require newer dialysis machines and high-quality dialysis solution to control the rate of fluid removal properly and to prevent backflow of dialysis solution impurities into the patient through the membrane.Dialyzer membranes used to be made primarily of cellulose (derived from cotton linter). The surface of such membranes was not very biocompatible, because exposed hydroxyl groups would activate complement
Complement system
The complement system helps or “complements” the ability of antibodies and phagocytic cells to clear pathogens from an organism. It is part of the immune system called the innate immune system that is not adaptable and does not change over the course of an individual's lifetime...
in the blood passing by the membrane. Therefore, the basic, "unsubstituted" cellulose membrane was modified. One change was to cover these hydroxyl groups with acetate groups (cellulose acetate); another was to mix in some compounds that would inhibit complement activation at the membrane surface (modified cellulose). The original "unsubstituted cellulose" membranes are no longer in wide use, whereas cellulose acetate and modified cellulose dialyzers are still used. Cellulosic membranes can be made in either low-flux or high-flux configuration, depending on their pore size.
Another group of membranes is made from synthetic materials, using polymer
Polymer
A polymer is a large molecule composed of repeating structural units. These subunits are typically connected by covalent chemical bonds...
s such as polyarylethersulfone, polyamide
Polyamide
A polyamide is a polymer containing monomers of amides joined by peptide bonds. They can occur both naturally and artificially, examples being proteins, such as wool and silk, and can be made artificially through step-growth polymerization or solid-phase synthesis, examples being nylons, aramids,...
, polyvinylpyrrolidone, polycarbonate, and polyacrylonitrile. These synthetic membranes activate complement to a lesser degree than unsubstituted cellulose membranes. Synthetic membranes can be made in either low- or high-flux configuration, but most are high-flux.
Nanotechnology is being used in some of the most recent high-flux membranes to create a uniform pore size. The goal of high-flux membranes is to pass relatively large molecules such as beta-2-microglobulin (MW 11,600 daltons), but not to pass albumin (MW ~66,400 daltons). Every membrane has pores in a range of sizes. As pore size increases, some high-flux dialyzers begin to let albumin pass out of the blood into the dialysate. This is thought to be undesirable, although one school of thought holds that removing some albumin may be beneficial in terms of removing protein-bound uremic toxins.
Membrane flux and outcome
Whether using a high-flux dialyzer improves patient outcomes is somewhat controversial, but several important studies have suggested that it has clinical benefits. The NIH-funded HEMO trial compared survival and hospitalizations in patients randomized to dialysis with either low-flux or high-flux membranes. Although the primary outcome (all-cause mortality) did not reach statistical significance in the group randomized to use high-flux membranes, several secondary outcomes were better in the high-flux group. A recent Cochrane analysis concluded that benefit of membrane choice on outcomes has not yet been demonstrated. A collaborative randomized trial from Europe, the MPO (Membrane Permeabilities Outcomes) study, comparing mortality in patients just starting dialysis using either high-flux or low-flux membranes, found a nonsignificant trend to improved survival in those using high-flux membranes, and a survival benefit in patients with lower serum albumin levels or in diabetics.Membrane flux and beta-2-microglobulin amyloidosis
High-flux dialysis membranes and/or intermittent on-line hemodiafiltration (IHDF) may also be beneficial in reducing complications of beta-2-microglobulin accumulation. Because beta-2-microglobulin is a large molecule, with a molecular weight of about 11,600 daltons, it does not pass at all through low-flux dialysis membranes. Beta-2-M is removed with high-flux dialysis, but is removed even more efficiently with IHDF. After several years (usually at least 5-7), patients on hemodialysis begin to develop complications from beta-2-M accumulation, including carpal tunnel syndrome, bone cysts, and deposits of this amyloid in joints and other tissues. Beta-2-M amyloidosis can cause very serious complications, including spondyloarthropathySpondyloarthropathy
Spondyloarthropathy is any joint disease of the vertebral column. Spondyloarthropathy with inflammation is called spondylarthritis. In contrast, spondylopathy is a disease of the vertebra itself, but many conditions involve both spondylopathy and spondyloarthropathy...
, and often is associated with shoulder joint problems. Observational studies from Europe and Japan have suggested that using high-flux membranes in dialysis mode, or IHDF, reduces beta-2-M complications in comparison to regular dialysis using a low-flux membrane.
Dialyzer size and efficiency
Dialyzers come in many different sizes. A larger dialyzer with a larger membrane area (A) will usually remove more solutes than a smaller dialyzer, especially at high blood flow rates. This also depends on the membrane permeability coefficient K0 for the solute in question. So dialyzer efficiency is usually expressed as the K0A - the product of permeability coefficient and area. Most dialyzers have membrane surface areas of 0.8 to 2.2 square meters, and values of K0A ranging from about 500 to 1500 mL/min. K0A, expressed in mL/min, can be thought of as the maximum clearance of a dialyzer at very high blood and dialysate flow rates.Reuse of dialyzers
The dialyzer may either be discarded after each treatment or be reused. Reuse requires an extensive procedure of high-level disinfection. Reused dialyzers are not shared between patients. There was an initial controversy about whether reusing dialyzers worsened patient outcomes. The consensus today is that reuse of dialyzers, if done carefully and properly, produces similar outcomes to single use of dialyzers.Dialyzer Reuse is a practice that has been around since the invention of the product. This practice includes the cleaning of a used dialyzer to be reused multiple times for the same patient. Dialysis clinics reuse dialyzers to become more economical and reduce the high costs of “single-use” dialysis which can be extremely expensive and wasteful. Single used dialyzers are initiated just once and then thrown out creating a large amount of bio-medical waste with no mercy for cost savings. If done right, dialyzer reuse can be very safe for dialysis patients.
There are two ways of reusing dialyzers. Firstly, there is manual reuse, which involves the cleaning of the used dialyzer by hand. The dialyzer is semi-disassembled then flushed repeatedly before being rinsed with water. It is then stored with a liquid disinfectant for 18+ hours until its next use. Secondly, there is the newer method of automated reuse by means of a medical device. These devices are beneficial to dialysis clinics that practice reuse – especially for large dialysis clinical entities – because they allow for several back to back cycles per day. The dialyzer is automatically cleaned by machine then filled with liquid disinfectant for storage. Automated reuse is more effective than manual reuse, but when reused over 15 times with current methodology, the dialyzer can lose B2m, middle molecule clearance and fiber pore structure integrity, reducing the effectiveness of the patients dialysis session.
Nursing care for hemodialysis patient
Adapt from nephrology nursing practice recommendations developed by Canadian Association of Nephrology and Technology (CANNT) based on best available evidence and clinical practice guidelines, a nephrology nurse should perform :Hemodialysis Vascular Access:
Assess the fistula/graft and arm before, after each dialysis or every shift: the access flow, complications
Assess the complication of central venous catheter: the tip placement, exit site, complications
document and notify appropriate health care provider regarding any concerns.
educates the patient with appropriate cleaning of fistula/graft and exit site; with recognizing and reporting signs and symptoms of infection and complication.
Hemodialysis adequacy:
Assesses patient constantly for signs and symptoms of inadequate dialysis.
Assesses possible causes of inadequate dialysis.
Educations patients the importance of receiving adequate dialysis.
Hemodialysis treatment and complications:
Performs head to toe physical assessment before, during and after hemodialysis regarding complications and access’s security.
Confirm and deliver dialysis prescription after review most update lab results.
Address any concerns of the patient and educate patient when recognizing the learning gap.
Medication management and infection control practice:
Collaborate with the patient to develop a medication regimen.
Follow infection control guidelines as per unit protocol.
See also
- DialysisDialysisIn medicine, dialysis is a process for removing waste and excess water from the blood, and is primarily used to provide an artificial replacement for lost kidney function in people with renal failure...
- Dialysis disequilibrium syndromeDialysis disequilibrium syndromeIn nephrology, dialysis disequilibrium syndrome, commonly abbreviated DDS, is the occurrence of neurologic signs and symptoms, attributed to cerebral edema, during or following shortly after intermittent hemodialysis....
- Home hemodialysisHome hemodialysisHome hemodialysis , is the provision of hemodialysis in the home of people with stage 5 chronic kidney disease. In the US home hemodialysis was the most common method of renal replacement therapy in the early 1970s before the introduction of the Federal ESRD program under Medicare...
- Peritoneal dialysisPeritoneal dialysisPeritoneal dialysis is a treatment for patients with severe chronic kidney disease. The process uses the patient's peritoneum in the abdomen as a membrane across which fluids and dissolved substances are exchanged from the blood...
- HemofiltrationHemofiltrationIn medicine, hemofiltration, also haemofiltration, is a renal replacement therapy similar to hemodialysis which is used almost exclusively in the intensive care setting...
- ExtracorporealExtracorporealAn extracorporeal medical procedure is a medical procedure which is performed outside the body.-Circulatory procedures:A procedure in which blood is taken from a patient's circulation to have a process applied to it before it is returned to the circulation...
therapies - Renal replacement therapyRenal replacement therapyRenal replacement therapy is a term used to encompass life-supporting treatments for renal failure.It includes:*hemodialysis,*peritoneal dialysis,*hemofiltration and*renal transplantation.These treatments will not cure chronic kidney disease...
- Step-by-step description of hemodialysisStep-by-step description of hemodialysisStarting hemodialysis is often a frightening experience. Hemodialysis machines are complicated and dialysis sessions often are punctuated by alarms. At the beginning of dialysis and at the end of dialysis a lot of things happen. Not knowing what it is can be anxiety provoking...
External links
- Your Kidneys and How They Work - (American) National Institute of Diabetes and Digestive and Kidney Diseases (NIDDK), NIH.
- Treatment Methods for Kidney Failure - (American) National Institute of Diabetes and Digestive and Kidney Diseases (NIDDK), NIH.
- Treatment Methods for Kidney Failure: Hemodialysis - (American) National Kidney and Urologic Diseases Information Clearinghouse, NIH.
- Online Community for Dialysis Patients by Dialysis Patients
- What is dialysis? - Kidney Foundation of Canada
- European Kidney Patients' Federation (CEAPIR)
- ARCH Project - European research project for development of a model to simulate hemodynamic changes induced by AVF surgery and long-term adaptation.

