
Knee replacement
Encyclopedia



Arthroplasty
Arthroplasty is an operative procedure of orthopedic surgery performed, in which the arthritic or dysfunctional joint surface is replaced with something better or by remodeling or realigning the joint by osteotomy or some other procedure.-Background:Previously, a popular form of arthroplasty was...
, is a surgical procedure to replace the weight-bearing surfaces of the knee joint to relieve the pain and disability of osteoarthritis
Osteoarthritis
Osteoarthritis also known as degenerative arthritis or degenerative joint disease, is a group of mechanical abnormalities involving degradation of joints, including articular cartilage and subchondral bone. Symptoms may include joint pain, tenderness, stiffness, locking, and sometimes an effusion...
. It may be performed for other knee diseases such as rheumatoid arthritis and psoriatic arthritis. In patients with severe deformity from advanced rheumatoid arthritis
Arthritis
Arthritis is a form of joint disorder that involves inflammation of one or more joints....
, trauma, or long standing osteoarthritis, the surgery may be more complicated and carry higher risk. Osteoporosis
Osteoporosis
Osteoporosis is a disease of bones that leads to an increased risk of fracture. In osteoporosis the bone mineral density is reduced, bone microarchitecture is deteriorating, and the amount and variety of proteins in bone is altered...
does not typically cause knee pain, deformity, or inflammation and is not a reason to perform knee replacement.
Other major causes of debilitating pain include meniscus tears, cartilage defects, and ligament tears. Debilitating pain from osteoarthritis is much more common in the elderly.
Knee replacement surgery can be performed as a partial or a total knee replacement. In general, the surgery consists of replacing the diseased or damaged joint surfaces of the knee with metal and plastic components shaped to allow continued motion of the knee.
The operation typically involves substantial postoperative pain, and includes vigorous physical rehabilitation. The recovery period may be 6 weeks or longer and may involve the use of mobility aids (e.g. walking frames, canes, crutches) to enable the patient's return to preoperative mobility.
History
The pioneer of knee replacement surgery was Leslie Gordon Percival Shiers (FRCS); his original papers were published in the Journal of Bone and Joint Surgery in 1954. Shiers refused to patent his invention, and demonstrated the operation throughout the world, inviting other surgeons to improve upon his original idea.Following John Charnley
John Charnley
Sir John Charnley was a British orthopaedic surgeon. He pioneered the hip replacement operation, which is now one of the most common operations both in the UK and elsewhere in the world...
's success with hip replacement
Hip replacement
Hip replacement is a surgical procedure in which the hip joint is replaced by a prosthetic implant. Hip replacement surgery can be performed as a total replacement or a hemi replacement. Such joint replacement orthopaedic surgery generally is conducted to relieve arthritis pain or fix severe...
in the 1960s attempts were made to design knee replacements. Gunston[Who?] and Marmor[Who?] were pioneers in North America. Marmor's design allowed for unicompartmental operations but did not always last well. In the 1970s the "Geometric" design, and John Insall's Condylar Knee design, found favor. Hinged knee replacements for salvage date back to Guepar[Who?] but did not stand up to wear. The history of knee replacement is the story of continued innovation to try to limit the problems of wear, loosening and loss of range of motion.
Indications
Knee replacement surgery is most commonly performed in people with advanced osteoarthritisOsteoarthritis
Osteoarthritis also known as degenerative arthritis or degenerative joint disease, is a group of mechanical abnormalities involving degradation of joints, including articular cartilage and subchondral bone. Symptoms may include joint pain, tenderness, stiffness, locking, and sometimes an effusion...
. It should be considered when conservative treatments have been exhausted. Total knee replacement is also an option to correct significant knee joint or bone trauma in young patients. Similarly, total knee replacement can be performed to correct serious valgus
Valgus deformity
In orthopedics, a valgus deformity is a term for outward angulation of the distal segment of a bone or joint. The opposite deformation, medial deviation of the distal bone, is called varus....
or varus deformity
Varus deformity
In orthopedics, a varus deformity is a term for the inward angulation of the distal segment of a bone or joint. The opposite of varus is called valgus.The terms varus and valgus always refer to the direction that the distal segment of the joint points....
. Physical therapy
Physical therapy
Physical therapy , often abbreviated PT, is a health care profession. Physical therapy is concerned with identifying and maximizing quality of life and movement potential within the spheres of promotion, prevention, diagnosis, treatment/intervention,and rehabilitation...
has been shown to improve function and may delay or prevent the need for knee replacement. You will notice extreme pain when performing physical activities requiring a wide range of motion in the knee joint.
Pre-operative preparation
Knee arthroplasty is major surgery. Pre-operative preparation begins immediately following surgical consultation and lasts approximately one month. Patient is to perform range of motion exercises and hip, knee and ankle strengthening as directed daily. Before the surgery is performed, pre-operative tests are done: usually a complete blood countComplete blood count
A complete blood count , also known as full blood count or full blood exam or blood panel, is a test panel requested by a doctor or other medical professional that gives information about the cells in a patient's blood...
, electrolytes, APTT and PT
Prothrombin time
The prothrombin time and its derived measures of prothrombin ratio and international normalized ratio are measures of the extrinsic pathway of coagulation. This test is also called "ProTime INR" and "INR PT". They are used to determine the clotting tendency of blood, in the measure of warfarin...
to measure blood clotting
Coagulation
Coagulation is a complex process by which blood forms clots. It is an important part of hemostasis, the cessation of blood loss from a damaged vessel, wherein a damaged blood vessel wall is covered by a platelet and fibrin-containing clot to stop bleeding and begin repair of the damaged vessel...
, chest X-ray
Chest X-ray
In medicine, a chest radiograph, commonly called a chest X-ray , is a projection radiograph of the chest used to diagnose conditions affecting the chest, its contents, and nearby structures...
s, ECG, and blood cross-matching
Cross-matching
Cross-matching blood, in transfusion medicine, refers to the complex testing that is performed prior to a blood transfusion, to determine if the donor's blood is compatible with the blood of an intended recipient, or to identify matches for organ transplants. Cross-matching is usually performed...
for possible transfusion
Blood transfusion
Blood transfusion is the process of receiving blood products into one's circulation intravenously. Transfusions are used in a variety of medical conditions to replace lost components of the blood...
. About a month before the surgery, the patient may be prescribed supplemental iron to boost the hemoglobin in their blood system. Accurate X-rays of the affected knee are needed to measure the size of components which will be needed. Medications such as warfarin
Warfarin
Warfarin is an anticoagulant. It is most likely to be the drug popularly referred to as a "blood thinner," yet this is a misnomer, since it does not affect the thickness or viscosity of blood...
and aspirin
Aspirin
Aspirin , also known as acetylsalicylic acid , is a salicylate drug, often used as an analgesic to relieve minor aches and pains, as an antipyretic to reduce fever, and as an anti-inflammatory medication. It was discovered by Arthur Eichengrun, a chemist with the German company Bayer...
will be stopped some days before surgery to reduce the amount of bleeding. Patients may be admitted on the day of surgery if the pre-op work-up is done
in the pre-anesthetic clinic or may come into hospital
Hospital
A hospital is a health care institution providing patient treatment by specialized staff and equipment. Hospitals often, but not always, provide for inpatient care or longer-term patient stays....
one or more days before surgery. Some hospitals offer a pre-operative seminar for this surgery.
Technique
The surgerySurgery
Surgery is an ancient medical specialty that uses operative manual and instrumental techniques on a patient to investigate and/or treat a pathological condition such as disease or injury, or to help improve bodily function or appearance.An act of performing surgery may be called a surgical...
involves exposure of the front of the knee, with detachment of part of the quadriceps muscle
Quadriceps muscle
The quadriceps femoris , also called simply the quadriceps, quadriceps extensor, quads, is a large muscle group that includes the four prevailing muscles on the front of the thigh...
(vastus medialis
Vastus medialis
The vastus medialis , often called the 'teardrop' muscle, is a medially located muscle of the quadriceps.-Function:The vasti appear to act largely in a co-ordinated manner throughout the control of knee extension...
) from the patella. The patella is displaced to one side of the joint allowing exposure of the distal end of the femur
Femur
The femur , or thigh bone, is the most proximal bone of the leg in tetrapod vertebrates capable of walking or jumping, such as most land mammals, birds, many reptiles such as lizards, and amphibians such as frogs. In vertebrates with four legs such as dogs and horses, the femur is found only in...
and the proximal end of the tibia
Tibia
The tibia , shinbone, or shankbone is the larger and stronger of the two bones in the leg below the knee in vertebrates , and connects the knee with the ankle bones....
. The ends of these bones are then accurately cut to shape using cutting guides oriented to the long axis of the bones. The cartilage
Cartilage
Cartilage is a flexible connective tissue found in many areas in the bodies of humans and other animals, including the joints between bones, the rib cage, the ear, the nose, the elbow, the knee, the ankle, the bronchial tubes and the intervertebral discs...
s and the anterior cruciate ligament
Anterior cruciate ligament
The anterior cruciate ligament is a cruciate ligament which is one of the four major ligaments of the human knee. In the quadruped stifle , based on its anatomical position, it is referred to as the cranial cruciate ligament.The ACL originates from deep within the notch of the distal femur...
are removed; the posterior cruciate ligament
Posterior cruciate ligament
The posterior cruciate ligament is one of the four major ligaments of the knee. It connects the posterior intercondylar area of the tibia to the medial condyle of the femur...
may also be removed but the tibial
Medial collateral ligament
The medial collateral ligament of the knee is one of the four major ligaments of the knee. It is on the medial side of the knee joint in humans and other primates. It is also known as the tibial collateral ligament, or abbreviated as the MCL.- Structure :It is a broad, flat, membranous band,...
and fibular
Fibular collateral ligament
-External links:*...
collateral ligaments are preserved. Metal components are then impacted onto the bone or fixed using polymethylmethacrylate (PMMA) cement. Alternative techniques exist that affix the implant without cement. These cement-less techniques may involve osseointegration
Osseointegration
Osseointegration derives from the Greek osteon, bone, and the Latin integrare, to make whole. The term refers to the direct structural and functional connection between living bone and the surface of a load-bearing artificial implant...
, including porous metal
Metal foam
A metal foam is a cellular structure consisting of a solid metal, frequently aluminium, containing a large volume fraction of gas-filled pores. The pores can be sealed , or they can form an interconnected network . The defining characteristic of metal foams is a very high porosity: typically...
prostheses.
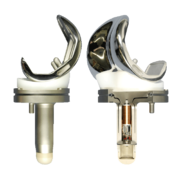
Femoral replacement
Polyethylene
Polyethylene or polythene is the most widely used plastic, with an annual production of approximately 80 million metric tons...
surface is then inserted onto the tibial component so that the weight is transferred metal to plastic not metal to metal. During the operation any deformities must be corrected, and the ligaments balanced so that the knee has a good range of movement and is stable. In some cases the articular surface of the patella is also removed and replaced by a polyethylene button cemented to the posterior surface of the patella. In other cases, the patella is replaced unaltered.
Variations
Different implant manufacturers require slightly different instrumentation and technique. No consensus has emerged over which one is the best. Clinical studies are very difficult to perform requiring large numbers of cases followed over many years. The most significant variations are between cemented and uncemented components, between operations which spare or sacrifice the posterior cruciate ligamentPosterior cruciate ligament
The posterior cruciate ligament is one of the four major ligaments of the knee. It connects the posterior intercondylar area of the tibia to the medial condyle of the femur...
and between resurfacing the patella or not. Some also study patient satisfaction data associated with pain.
Minimally invasive procedure
Minimally invasive procedure
There are three main categories which describe the invasiveness of surgical procedures. These are: non-invasive procedures, minimally invasive procedures, and invasive procedures ....
s have been developed in total knee replacement (TKR) that do not cut the quadriceps femoris muscle. There are different definitions of minimally invasive knee surgery, which may include a shorter incision length, retraction of the patella (kneecap) without eversion (rotating out), and specialized instruments. There are few randomized trials, but studies have found less postoperative pain, shorter hospital stays, and shorter recovery. However, no studies have shown long-term benefits.
Partial knee replacement
Unicompartmental arthroplasty (UKA), also called partial knee replacement,... is an option for some patients. The knee is generally divided into three "compartments": medial (the inside part of the knee), lateral (the outside), and patellofemoral (the joint between the kneecap and the thighbone). Most patients with arthritis severe enough to consider knee replacement have significant wear in two or more of the above compartments and are best treated with total knee replacement. A minority of patients (the exact percentage is hotly debated but is probably between 10 and 30 percent) have wear confined primarily to one compartment, usually the medial, and may be candidates for unicompartmental knee replacement. Advantages of UKA compared to TKA include smallier incision, easier post-op rehabilitation, better post-operative ROM, shorter hospital stay, less blood loss, lower risk of infection, stiffness, and blood clots, and easier revision if necessary. While most recent data suggests that UKA in properly selected patients has survival rates comparable to TKA, most surgeons believe that TKA is the more reliable long term procedure. Persons with infectious or inflammatory arthritis (Rheumatoid, LupusLupus erythematosus
Lupus erythematosus is a category for a collection of diseases with similar underlying problems with immunity . Symptoms of these diseases can affect many different body systems, including joints, skin, kidneys, blood cells, heart, and lungs...
, Psoriatic ), or marked deformity are not candidates for this procedure.
Post-operative rehabilitation
Post-operative hospitalization varies from one day to seven days on average, depending on the health status of the patient and the amount of support available outside the hospital setting. Protected weight bearingWeight bearing
In orthopedics, weight-bearing is the amount of weight a patient puts on the leg on which surgery has been performed. In general, it is described as a percentage of the body weight, because each leg of a healthy person carries the full body weight when walking, in an alternating fashion.After...
on crutches or a walker
Walker (tool)
A walker or walking frame is a tool for disabled or elderly people who need additional support to maintain balance or stability while walking...
is required, until the quadriceps muscle has healed and recovered its strength. Continuous Passive Motion or CPM is commonly used, but its effectiveness is questioned. Patients typically undergo several weeks of physical therapy
Physical therapy
Physical therapy , often abbreviated PT, is a health care profession. Physical therapy is concerned with identifying and maximizing quality of life and movement potential within the spheres of promotion, prevention, diagnosis, treatment/intervention,and rehabilitation...
and occupational therapy
Occupational therapy
Occupational therapy is a discipline that aims to promote health by enabling people to perform meaningful and purposeful activities. Occupational therapists work with individuals who suffer from a mentally, physically, developmentally, and/or emotionally disabling condition by utilizing treatments...
to restore motion, strength, and function. Often range-of-motion to the limits of the prosthesis is recovered over the first two weeks (the earlier the better). At six weeks, patients have usually progressed to full weight bearing with a cane. Complete recovery from the operation involving return to full normal function may take three months, and some patients notice a gradual improvement lasting many months longer than that.
Risks and complications
Risks and complications in knee replacement are similar to those associated with all joint replacements. The most serious complication is infection of the joint, which occurs in <1% of patients. Deep vein thrombosisDeep vein thrombosis
Deep vein thrombosis is the formation of a blood clot in a deep vein. Deep vein thrombosis commonly affects the leg veins or the deep veins of the pelvis. Occasionally the veins of the arm are affected...
occurs in up to 15% of patients, and is symptomatic in 2-3%. Nerve injuries occur in 1-2% of patients. Persistent pain or stiffness occurs in 8-23% of patients. Prosthesis failure occurs in approximately 2% of patients at 5 years.
A recent literature review showed that there is increased risk in complications for morbidly obese patients after going through total knee replacement, these patients should be advised to lose weight before surgery and, if suitable, would probably benefit from bariatric surgery.
Deep Vein thrombosis
According to the American Academy of Orthopedic Surgeons (AAOS), "blood clots in the leg veins are the most common complication of knee replacement surgery. Your orthopedic surgeon will outline a prevention program, which may include periodic elevation of your legs, lower leg exercises to increase circulation, support stockings and medication to thin your blood."Fractures
Periprosthetic fractures are becoming more frequent with the aging patient population and can occur intraoperatively or postoperatively.Loss of Motion
The knee at times may not recover its normal range of motion (0 - 135 degrees usually) after total knee replacement. Much of this is dependent on pre-operative function. Most patients can achieve 0 - 110 degrees, but stiffness of the joint can occur. In some situations, manipulation of the knee under anesthetic is used to improve post operative stiffness. There are also many implants from manufacturers that are designed to be "high-flex" knees, offering a greater range of motion.Instability
In some patients, the kneecap is unstable post-surgery and dislocates to the outer side of the knee. This is painful and usually needs to be treated by surgery to realign the kneecap. However this is quite rare.In the past, there was a considerable risk of the implant components loosening over time as a result of wear. As medical technology has improved however, this risk has fallen considerably. Knee replacement implants can now last up to 20 years.
Wait Period
The normal wait period for a patient that is under 70 years old and is a non-emergency is usually between three and four months. The normal wait period for someone who is over 70 years old and is a non-emergency is usually between five months and a year.Infection
The current classification of AAOS divides prosthetic infections into four types.- Type 1 (Positive intraoperative culture): 2 positive intraoperative cultures
- Type 2 (early postoperative infection): Infection occurring within first month after surgery
- Type 3 (acute hematogenous infection): Hematogenous seeding of site of previously well-functioning prosthesis
- Type 4 (late chronic infection): Chronic indolent clinical course; infection present for >1 month
While it is relatively rare, periprosthetic infection remains one of the most challenging complications of joint arthroplasty.
A detailed clinical history and physical remain the most reliable tool to recognize a potential periprosthetic infection. In some cases the classic signs of fever, chills, painful joint, and a draining sinus may be present, and diagnostic studies are simply done to confirm the diagnosis. In reality though, most patients do not present with those clinical signs, and in fact the clinical presentation may overlap with other complications such as aseptic loosening. In those cases diagnostic tests can be useful in confirming or excluding infection.
According to a recent review the following tests can be used in the diagnosis of a periprosthetic infection.
- Conventional radiograph: Rule out other conditions such as loosening and/or osteolysis.
- Radionucleotide Imaging: Technetium-99m Sulfur imaging combined with indium-111-labeled leukocytes probably offers improved specificity than either test alone. Gallium 67 scans alone have low sensitivity for infection. FDG-PET imaging has been shown to have variable specificity and sensitivity.
- Serology: Elevated serum C-reactive protein (CRP) and Erythrocyte Sedimentation Rate (ESR) more than three months following arthroplasty are good screening tests.
- Cultures: High sensitivity and specificity, but only if done two weeks following antibiotic discontinuation. Gram stains have low specificity and sensitivity. The predictive value of a positive culture increases if the culture is performed in patient with high clinical suspicion, rather than a screening test.
- Joint fluid leukocyte counts: A joint fluid white blood cell count of more than 500/μl is suggestive of an infection.
- Frozen sections of implant membranes: More than five white blood cells/High power field is indicative of infection.
- Newer tests: Polymerase chain reactions involving the bacterial 16S rRNA have high rates of false positives because they can detect necrotic bacterial debris even in the absence of active infection.
None of the above laboratory tests has 100% sensitivity or specificity for diagnosing infection. Specificity improves when the tests are performed in patients in whom clinical suspicion exists. ESR and CRP remain good 1st line tests for screening (high sensitivity, low specificity). Aspiration of the joint remains the test with the highest specificity for confirming infection.
The choice of treatment depends on the type of prosthetic infection.
- Positive intraoperative cultures: Antibiotic therapy alone
- Early post-operative infections: debridement, antibiotics, and retention of prosthesis.
- Acute hematogenous infections: debridement, antibiotic therapy, retention of prosthesis.
- Late chronic: delayed exchange arthroplasty. Surgical débridement and parenteral antibiotics alone in this group has limited success, and standard of care involves exchange arthroplasty.
Appropriate antibiotic doses can be found at the following instructional course lecture by AAOS
See also
- Autologous chondrocyte implantationAutologous chondrocyte implantationAutologous chondrocyte implantation is a biomedical treatment that repairs damages in articular cartilage. ACI provides pain relief while at the same time slowing down the progression or considerably delaying partial or total joint replacement surgery...
- Microfracture surgeryMicrofracture surgeryMicrofracture surgery is one of the articular cartilage repair surgical techniques that works by creating tiny fractures in the underlying bone. This causes new cartilage to develop from a so-called super-clot...
- Knee osteoarthritisKnee osteoarthritisKnee osteoarthritis is a degenerative disease of the knee joint. It is more common in people older than 40 years. Women have greater chance to be affected.-Signs and symptoms:Some of the signs and symptoms associated with knee osteoarthritis include:* Pain...
- OsseointegrationOsseointegrationOsseointegration derives from the Greek osteon, bone, and the Latin integrare, to make whole. The term refers to the direct structural and functional connection between living bone and the surface of a load-bearing artificial implant...
External links
- Detailed wiki page on recovery from knee replacement surgery
- Knee replacement surgery from the American Medical Videos Journal
- Knee Replacement - a simple patient guide

