
Coagulation
Encyclopedia
Coagulation is a complex process by which blood
forms clots. It is an important part of hemostasis
, the cessation of blood loss from a damaged vessel, wherein a damaged blood vessel
wall is covered by a platelet
and fibrin
-containing clot to stop bleeding and begin repair of the damaged vessel. Disorders of coagulation can lead to an increased risk of bleeding (hemorrhage) or obstructive clotting (thrombosis
).
Coagulation is highly conserved throughout biology; in all mammal
s, coagulation involves both a cellular (platelet) and a protein
(coagulation factor) component. The system in humans has been the most extensively researched and is therefore the best understood.
Coagulation begins almost instantly after an injury to the blood vessel has damaged the endothelium
lining the vessel. Exposure of the blood to proteins such as tissue factor
initiates changes to blood platelets and the plasma protein fibrinogen
, a clotting factor. Platelet
s immediately form a plug at the site of injury; this is called primary hemostasis. Secondary hemostasis occurs simultaneously: Proteins in the blood plasma
, called coagulation factors or clotting factors, respond in a complex cascade to form fibrin
strands, which strengthen the platelet plug.
(vWF), present under the endothelium
. vWF is a protein secreted by healthy endothelium, forming a layer between the endothelium and underlying basement membrane
. When the endothelium is damaged, the normally-isolated, underlying vWF is exposed to white blood cells and recruits Factor VIII
, collagen
, and other clotting factors. Circulating platelets bind to collagen with surface collagen-specific glycoprotein
Ia/IIa receptors. This adhesion is strengthened further by additional circulating proteins vWF, which forms additional links between the platelets glycoprotein Ib/IX/V and the collagen fibrils. These adhesions activate the platelets.
Activated platelets release the contents of stored granules into the blood plasma. The granules include ADP
, serotonin
, platelet-activating factor
(PAF), vWF
, platelet factor 4
, and thromboxane A2
(TXA2), which, in turn, activate additional platelets. The granules' contents activate a Gq-linked protein receptor
cascade, resulting in increased calcium concentration in the platelets' cytosol. The calcium activates protein kinase C
, which, in turn, activates phospholipase A2
(PLA2). PLA2 then modifies the integrin
membrane glycoprotein IIb/IIIa, increasing its affinity to bind fibrinogen. The activated platelets change shape from spherical to stellate, and the fibrinogen cross-links with glycoprotein IIb/IIIa aid in aggregation of adjacent platelets (completing primary hemostasis).
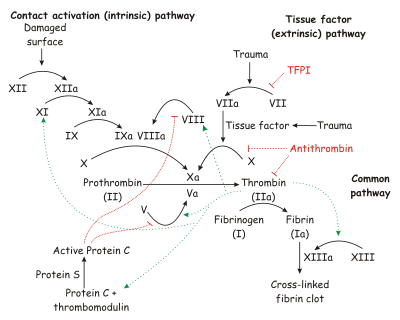
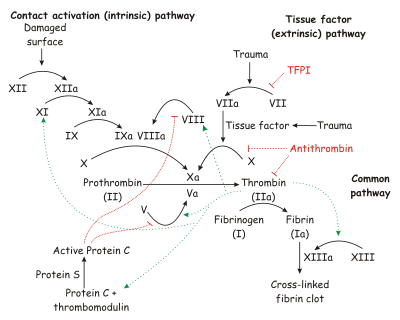 The coagulation cascade of secondary hemostasis has two pathways which lead to fibrin formation. These are the contact activation pathway (also known as the intrinsic pathway), and the tissue factor pathway (also known as the extrinsic pathway). It was previously thought that the coagulation cascade consisted of two pathways of equal importance joined to a common pathway. It is now known that the primary pathway for the initiation of blood coagulation is the tissue factor pathway. The pathways are a series of reactions, in which a zymogen
The coagulation cascade of secondary hemostasis has two pathways which lead to fibrin formation. These are the contact activation pathway (also known as the intrinsic pathway), and the tissue factor pathway (also known as the extrinsic pathway). It was previously thought that the coagulation cascade consisted of two pathways of equal importance joined to a common pathway. It is now known that the primary pathway for the initiation of blood coagulation is the tissue factor pathway. The pathways are a series of reactions, in which a zymogen
(inactive enzyme precursor) of a serine protease
and its glycoprotein
co-factor are activated to become active components that then catalyze the next reaction in the cascade, ultimately resulting in cross-linked fibrin. Coagulation factors are generally indicated by Roman numerals, with a lowercase a appended to indicate an active form.
The coagulation factors are generally serine protease
s (enzymes). There are some exceptions. For example, FVIII and FV are glycoproteins, and Factor XIII is a transglutaminase
. Serine proteases act by cleaving other proteins at specific serine residues. The coagulation factors circulate as inactive zymogens.
The coagulation cascade is classically divided into three pathways. The tissue factor and contact activation pathways both activate the "final common pathway" of factor X, thrombin and fibrin.
, the most important constituent of the coagulation cascade in terms of its feedback activation roles, is released instantaneously. FVIIa circulates in a higher amount than any other activated coagulation factor.
The contact activation pathway begins with formation of the primary complex on collagen
by high-molecular-weight kininogen (HMWK), prekallikrein
, and FXII (Hageman factor). Prekallikrein
is converted to kallikrein
and FXII becomes FXIIa. FXIIa converts FXI into FXIa. Factor XIa activates FIX, which with its co-factor FVIIIa form the tenase
complex, which activates FX to FXa. The minor role that the contact activation pathway has in initiating clot formation can be illustrated by the fact that patients with severe deficiencies of FXII, HMWK, and prekallikrein
do not have a bleeding disorder. Instead, contact activation system seems to be more involved in inflammation. Patients without FXII (Hageman factor) suffer from constant infections.
to fibrin, the building block of a hemostatic plug. In addition, it activates Factors VIII and V and their inhibitor protein C
(in the presence of thrombomodulin
), and it activates Factor XIII, which forms covalent bond
s that crosslink the fibrin polymers that form from activated monomers.
Following activation by the contact factor or tissue factor pathways, the coagulation cascade is maintained in a prothrombotic state by the continued activation of FVIII and FIX to form the tenase
complex, until it is down-regulated by the anticoagulant pathways.
. The main enzyme responsible for this process (plasmin
) is regulated by various activators and inhibitors.
. Coagulation can physically trap invading microbes in blood clots. Also, some products of the coagulation system can contribute to the innate immune system
by their ability to increase vascular permeability and act as chemotactic agents for phagocytic cells. In addition, some of the products of the coagulation system are directly antimicrobial
. For example, beta-lysine
, a protein produced by platelets during coagulation, can cause lysis
of many Gram-positive bacteria by acting as a cationic detergent. Many acute-phase proteins of inflammation
are involved in the coagulation system. In addition, pathogenic bacteria may secrete agents that alter the coagulation system, e.g. coagulase
and streptokinase
.
The contact activation (intrinsic) pathway is initiated by activation of the "contact factors" of plasma, and can be measured by the activated partial thromboplastin
time (aPTT) test.
The tissue factor (extrinsic) pathway is initiated by release of tissue factor
(a specific cellular lipoprotein), and can be measured by the prothrombin time
(PT) test. PT results are often reported as ratio (INR value) to monitor dosing of oral anticoagulants such as warfarin
.
The quantitative and qualitative screening of fibrinogen is measured by the thrombin clotting time
(TCT). Measurement of the exact amount of fibrinogen present in the blood is generally done using the Clauss method for fibrinogen testing. Many analysers are capable of measuring a "derived fibrinogen" level from the graph of the Prothrombin time clot.
If a coagulation factor is part of the contact activation or tissue factor pathway, a deficiency of that factor will affect only one of the tests: Thus hemophilia A, a deficiency of factor VIII, which is part of the contact activation pathway, results in an abnormally prolonged aPTT test but a normal PT test. The exceptions are prothrombin, fibrinogen, and some variants of FX that can be detected only by either aPTT or PT. If an abnormal PT or aPTT is present, additional testing will occur to determine which (if any) factor is present as aberrant concentrations.
Deficiencies of fibrinogen (quantitative or qualitative) will affect all screening tests.
, Bernard-Soulier syndrome
(abnormal glycoprotein Ib-IX-V complex), gray platelet syndrome
(deficient alpha granules), and delta storage pool deficiency (deficient dense granules). Most are rare conditions. Most inborn platelet pathologies predispose to hemorrhage. Von Willebrand disease
is due to deficiency or abnormal function of von Willebrand factor
, and leads to a similar bleeding pattern; its milder forms are relatively common.
Decreased platelet numbers may be due to various causes, including insufficient production (e.g., in myelodysplastic syndrome
or other bone marrow disorders), destruction by the immune system (immune thrombocytopenic purpura/ITP), and consumption due to various causes (thrombotic thrombocytopenic purpura
/TTP, hemolytic-uremic syndrome
/HUS, paroxysmal nocturnal hemoglobinuria
/PNH, disseminated intravascular coagulation
/DIC, heparin-induced thrombocytopenia
/HIT). Most consumptive conditions lead to platelet activation, and some are associated with thrombosis.
.
Von Willebrand disease
(which behaves more like a platelet disorder except in severe cases), is the most common hereditary bleeding disorder and is characterized as being inherited autosomal recessive or dominant. In this disease, there is a defect in von Willebrand factor (vWF), which mediates the binding of glycoprotein Ib (GPIb) to collagen. This binding helps mediate the activation of platelets and formation of primary hemostasis.
Bernard-Soulier syndrome is a defect or deficiency in GPIb. GPIb, the receptor for vWF, can be defective and lead to lack of primary clot formation (primary hemostasis) and increased bleeding tendency. This is an autosomal recessive inherited disorder.
Thrombasthenia of Glanzman and Naegeli (Glanzmann thrombasthenia) is extremely rare. It is characterized by a defect in GPIIb/IIIa fibrinogen receptor complex. When GPIIb/IIIa receptor is dysfunctional, fibrinogen cannot cross-link platelets, which inhibits primary hemostasis. This is an autosomal recessive inherited disorder.
In liver failure
(acute and chronic forms), there is insufficient production of coagulation factors by the liver; this may increase bleeding risk.
Deficiency of Vitamin K may also contribute to bleeding disorders because clotting factor maturation depends on Vitamin K.
Thrombosis
is the pathological development of blood clots. These clots may break free and become mobile, forming an embolus
or grow to such a size that occludes the vessel in which it developed. An embolism
is said to occur when the thrombus
(blood clot) becomes a mobile embolus and migrates to another part of the body, interfering with blood circulation and hence impairing organ function downstream of the occlusion. This causes ischemia
and often leads to ischemic necrosis
of tissue. Most cases of thrombosis are due to acquired extrinsic problems (surgery
, cancer
, immobility, obesity
, economy class syndrome), but a small proportion of people harbor predisposing conditions known collectively as thrombophilia (e.g., antiphospholipid syndrome
, factor V Leiden
, and various other rarer genetic disorders).
Mutations in factor XII
have been associated with an asymptomatic prolongation in the clotting time and possibly a tendency toward thrombophlebitis
. Other mutations have been linked with a rare form of hereditary angioedema
(type III).
s, and other hemostatic agents are also used for use in sealing severe injuries quickly (such as in traumatic bleeding secondary to gunshot wounds). Thrombin and fibrin glue
are used surgically to treat bleeding and to thrombose aneurysms.
Desmopressin
is used to improve platelet function by activating arginine vasopressin receptor 1A
.
Coagulation factor concentrates are used to treat hemophilia, to reverse the effects of anticoagulants, and to treat bleeding in patients with impaired coagulation factor synthesis or increased consumption. Prothrombin complex concentrate
, cryoprecipitate
and fresh frozen plasma
are commonly-used coagulation factor products. Recombinant activated human factor VII
is increasingly popular in the treatment of major bleeding.
Tranexamic acid
and aminocaproic acid
inhibit fibrinolysis, and lead to a de facto reduced bleeding rate. Before its withdrawal, aprotinin
was used in some forms of major surgery to decrease bleeding risk and need for blood products.
include aspirin
, clopidogrel
, dipyridamole
and ticlopidine
; the parenteral glycoprotein IIb/IIIa inhibitors
are used during angioplasty
. Of the anticoagulants, warfarin
(and related coumarin
s) and heparin
are the most commonly used. Warfarin affects the vitamin K-dependent clotting factors (II, VII, IX,X) , whereas heparin and related compounds increase the action of antithrombin on thrombin and factor Xa. A newer class of drugs, the direct thrombin inhibitor
s, is under development; some members are already in clinical use (such as lepirudin
). Also under development are other small molecular compounds that interfere directly with the enzymatic action of particular coagulation factors (e.g., rivaroxaban
, dabigatran
, apixaban
).
(1801–1858) described fibrin, the substance of a thrombus
. Its soluble precursor, fibrinogen
, was thus named by Rudolf Virchow
(1821–1902), and isolated chemically by Prosper Sylvain Denis (1799–1863). Alexander Schmidt
suggested that the conversion from fibrinogen to fibrin is the result of an enzymatic
process, and labeled the hypothetical enzyme "thrombin
" and its precursor "prothrombin". Arthus
discovered in 1890 that calcium was essential in coagulation. Platelet
s were identified in 1865, and their function was elucidated by Giulio Bizzozero
in 1882.
The theory that thrombin is generated by the presence of tissue factor
was consolidated by Paul Morawitz
in 1905. At this stage, it was known that thrombokinase/thromboplastin (factor III) is released by damaged tissues, reacting with prothrombin (II), which, together with calcium
(IV), forms thrombin, which converts fibrinogen into fibrin (I).
A first clue as to the actual complexity of the system of coagulation was the discovery of proaccelerin (initially and later called Factor V) by Paul Owren (1905–1990) in 1947. He also postulated its function to be the generation of accelerin (Factor VI), which later turned out to be the activated form of V (or Va); hence, VI is not now in active use.
Factor VII (also known as serum prothrombin conversion accelerator or proconvertin, precipitated by barium sulfate) was discovered in a young female patient in 1949 and 1951 by different groups.
Factor VIII
turned out to be deficient in the clinically recognised but etiologically elusive hemophilia A
; it was identified in the 1950s and is alternatively called antihemophilic globulin due to its capability to correct hemophilia A.
Factor IX was discovered in 1952 in a young patient with hemophilia B
named Stephen Christmas
(1947–1993). His deficiency was described by Dr. Rosemary Biggs and Professor R.G. MacFarlane in Oxford, UK. The factor is, hence, called Christmas Factor. Christmas lived in Canada, and campaigned for blood transfusion safety until succumbing to transfusion-related AIDS
at age 46. An alternative name for the factor is plasma thromboplastin component, given by an independent group in California.
Hageman factor, now known as factor XII, was identified in 1955 in an asymptomatic patient with a prolonged bleeding time named of John Hageman. Factor X, or Stuart-Prower factor, followed, in 1956. This protein was identified in a Ms. Audrey Prower of London, who had a lifelong bleeding tendency. In 1957, an American group identified the same factor in a Mr. Rufus Stuart. Factors XI and XIII were identified in 1953 and 1961, respectively.
The view that the coagulation process is a "cascade" or "waterfall" was enunciated almost simultaneously by MacFarlane in the UK and by Davie and Ratnoff in the USA, respectively.
and high-molecular-weight kininogen, respectively.
Factors III and VI are unassigned, as thromboplastin was never identified, and actually turned out to consist of ten further factors, and accelerin was found to be activated Factor V.
.
s in membrane - Discoidin domain
s of blood coagulation factors
Blood
Blood is a specialized bodily fluid in animals that delivers necessary substances such as nutrients and oxygen to the cells and transports metabolic waste products away from those same cells....
forms clots. It is an important part of hemostasis
Hemostasis
Hemostasis or haemostasis is a process which causes bleeding to stop, meaning to keep blood within a damaged blood vessel . Most of the time this includes blood changing from a liquid to a solid state. Intact blood vessels are central to moderating blood's tendency to clot...
, the cessation of blood loss from a damaged vessel, wherein a damaged blood vessel
Blood vessel
The blood vessels are the part of the circulatory system that transports blood throughout the body. There are three major types of blood vessels: the arteries, which carry the blood away from the heart; the capillaries, which enable the actual exchange of water and chemicals between the blood and...
wall is covered by a platelet
Platelet
Platelets, or thrombocytes , are small,irregularly shaped clear cell fragments , 2–3 µm in diameter, which are derived from fragmentation of precursor megakaryocytes. The average lifespan of a platelet is normally just 5 to 9 days...
and fibrin
Fibrin
Fibrin is a fibrous, non-globular protein involved in the clotting of blood. It is a fibrillar protein that is polymerised to form a "mesh" that forms a hemostatic plug or clot over a wound site....
-containing clot to stop bleeding and begin repair of the damaged vessel. Disorders of coagulation can lead to an increased risk of bleeding (hemorrhage) or obstructive clotting (thrombosis
Thrombosis
Thrombosis is the formation of a blood clot inside a blood vessel, obstructing the flow of blood through the circulatory system. When a blood vessel is injured, the body uses platelets and fibrin to form a blood clot to prevent blood loss...
).
Coagulation is highly conserved throughout biology; in all mammal
Mammal
Mammals are members of a class of air-breathing vertebrate animals characterised by the possession of endothermy, hair, three middle ear bones, and mammary glands functional in mothers with young...
s, coagulation involves both a cellular (platelet) and a protein
Protein
Proteins are biochemical compounds consisting of one or more polypeptides typically folded into a globular or fibrous form, facilitating a biological function. A polypeptide is a single linear polymer chain of amino acids bonded together by peptide bonds between the carboxyl and amino groups of...
(coagulation factor) component. The system in humans has been the most extensively researched and is therefore the best understood.
Coagulation begins almost instantly after an injury to the blood vessel has damaged the endothelium
Endothelium
The endothelium is the thin layer of cells that lines the interior surface of blood vessels, forming an interface between circulating blood in the lumen and the rest of the vessel wall. These cells are called endothelial cells. Endothelial cells line the entire circulatory system, from the heart...
lining the vessel. Exposure of the blood to proteins such as tissue factor
Tissue factor
Tissue factor, also called platelet tissue factor, factor III, thrombokinase, or CD142 is a protein present in subendothelial tissue, platelets, and leukocytes necessary for the initiation of thrombin formation from the zymogen prothrombin. An incorrect synonym is thromboplastin...
initiates changes to blood platelets and the plasma protein fibrinogen
Fibrinogen
Fibrinogen is a soluble plasma glycoprotein, synthesised by the liver, that is converted by thrombin into fibrin during blood coagulation. This is achieved through processes in the coagulation cascade that activate the zymogen prothrombin to the serine protease thrombin, which is responsible for...
, a clotting factor. Platelet
Platelet
Platelets, or thrombocytes , are small,irregularly shaped clear cell fragments , 2–3 µm in diameter, which are derived from fragmentation of precursor megakaryocytes. The average lifespan of a platelet is normally just 5 to 9 days...
s immediately form a plug at the site of injury; this is called primary hemostasis. Secondary hemostasis occurs simultaneously: Proteins in the blood plasma
Blood plasma
Blood plasma is the straw-colored liquid component of blood in which the blood cells in whole blood are normally suspended. It makes up about 55% of the total blood volume. It is the intravascular fluid part of extracellular fluid...
, called coagulation factors or clotting factors, respond in a complex cascade to form fibrin
Fibrin
Fibrin is a fibrous, non-globular protein involved in the clotting of blood. It is a fibrillar protein that is polymerised to form a "mesh" that forms a hemostatic plug or clot over a wound site....
strands, which strengthen the platelet plug.
Platelet activation
Damage to blood vessel walls exposes subendothelium proteins, most notably von Willebrand factorVon Willebrand factor
von Willebrand factor is a blood glycoprotein involved in hemostasis. It is deficient or defective in von Willebrand disease and is involved in a large number of other diseases, including thrombotic thrombocytopenic purpura, Heyde's syndrome, and possibly hemolytic-uremic syndrome...
(vWF), present under the endothelium
Endothelium
The endothelium is the thin layer of cells that lines the interior surface of blood vessels, forming an interface between circulating blood in the lumen and the rest of the vessel wall. These cells are called endothelial cells. Endothelial cells line the entire circulatory system, from the heart...
. vWF is a protein secreted by healthy endothelium, forming a layer between the endothelium and underlying basement membrane
Basement membrane
The basement membrane is a thin sheet of fibers that underlies the epithelium, which lines the cavities and surfaces of organs including skin, or the endothelium, which lines the interior surface of blood vessels.- Composition :...
. When the endothelium is damaged, the normally-isolated, underlying vWF is exposed to white blood cells and recruits Factor VIII
Factor VIII
Factor VIII is an essential blood clotting factor also known as anti-hemophilic factor . In humans, Factor VIII is encoded by the F8 gene...
, collagen
Collagen
Collagen is a group of naturally occurring proteins found in animals, especially in the flesh and connective tissues of mammals. It is the main component of connective tissue, and is the most abundant protein in mammals, making up about 25% to 35% of the whole-body protein content...
, and other clotting factors. Circulating platelets bind to collagen with surface collagen-specific glycoprotein
Glycoprotein
Glycoproteins are proteins that contain oligosaccharide chains covalently attached to polypeptide side-chains. The carbohydrate is attached to the protein in a cotranslational or posttranslational modification. This process is known as glycosylation. In proteins that have segments extending...
Ia/IIa receptors. This adhesion is strengthened further by additional circulating proteins vWF, which forms additional links between the platelets glycoprotein Ib/IX/V and the collagen fibrils. These adhesions activate the platelets.
Activated platelets release the contents of stored granules into the blood plasma. The granules include ADP
Adenosine diphosphate
Adenosine diphosphate, abbreviated ADP, is a nucleoside diphosphate. It is an ester of pyrophosphoric acid with the nucleoside adenosine. ADP consists of the pyrophosphate group, the pentose sugar ribose, and the nucleobase adenine....
, serotonin
Serotonin
Serotonin or 5-hydroxytryptamine is a monoamine neurotransmitter. Biochemically derived from tryptophan, serotonin is primarily found in the gastrointestinal tract, platelets, and in the central nervous system of animals including humans...
, platelet-activating factor
Platelet-activating factor
Platelet-activating factor, also known as a PAF, PAF-acether or AGEPC is a potent phospholipid activator and mediator of many leukocyte functions, including platelet aggregation and degranulation, inflammation, and anaphylaxis...
(PAF), vWF
Von Willebrand factor
von Willebrand factor is a blood glycoprotein involved in hemostasis. It is deficient or defective in von Willebrand disease and is involved in a large number of other diseases, including thrombotic thrombocytopenic purpura, Heyde's syndrome, and possibly hemolytic-uremic syndrome...
, platelet factor 4
Platelet factor 4
Platelet factor 4 is a small cytokine belonging to the CXC chemokine family that is also known as chemokine ligand 4 . This chemokine is released from alpha-granules of activated platelets during platelet aggregation, and promotes blood coagulation by moderating the effects of heparin-like...
, and thromboxane A2
Thromboxane A2
Thromboxane A2 is a thromboxane. It is produced by activated platelets and has prothrombotic properties: it stimulates activation of new platelets as well as increases platelet aggregation. This is achieved by mediating expression of the glycoprotein complex GP IIb/IIIa in the cell membrane of...
(TXA2), which, in turn, activate additional platelets. The granules' contents activate a Gq-linked protein receptor
G protein-coupled receptor
G protein-coupled receptors , also known as seven-transmembrane domain receptors, 7TM receptors, heptahelical receptors, serpentine receptor, and G protein-linked receptors , comprise a large protein family of transmembrane receptors that sense molecules outside the cell and activate inside signal...
cascade, resulting in increased calcium concentration in the platelets' cytosol. The calcium activates protein kinase C
Protein kinase C
Protein kinase C also known as PKC is a family of enzymes that are involved in controlling the function of other proteins through the phosphorylation of hydroxyl groups of serine and threonine amino acid residues on these proteins. PKC enzymes in turn are activated by signals such as increases in...
, which, in turn, activates phospholipase A2
Phospholipase A2
Phospholipases A2 are enzymes that release fatty acids from the second carbon group of glycerol. This particular phospholipase specifically recognizes the sn-2 acyl bond of phospholipids and catalytically hydrolyzes the bond releasing arachidonic acid and lysophospholipids...
(PLA2). PLA2 then modifies the integrin
Integrin
Integrins are receptors that mediate attachment between a cell and the tissues surrounding it, which may be other cells or the ECM. They also play a role in cell signaling and thereby regulate cellular shape, motility, and the cell cycle....
membrane glycoprotein IIb/IIIa, increasing its affinity to bind fibrinogen. The activated platelets change shape from spherical to stellate, and the fibrinogen cross-links with glycoprotein IIb/IIIa aid in aggregation of adjacent platelets (completing primary hemostasis).
The coagulation cascade
Zymogen
A zymogen is an inactive enzyme precursor. A zymogen requires a biochemical change for it to become an active enzyme. The biochemical change usually occurs in a lysosome where a specific part of the precursor enzyme is cleaved in order to activate it...
(inactive enzyme precursor) of a serine protease
Serine protease
Serine proteases are enzymes that cleave peptide bonds in proteins, in which serine serves as the nucleophilic amino acid at the active site.They are found ubiquitously in both eukaryotes and prokaryotes...
and its glycoprotein
Glycoprotein
Glycoproteins are proteins that contain oligosaccharide chains covalently attached to polypeptide side-chains. The carbohydrate is attached to the protein in a cotranslational or posttranslational modification. This process is known as glycosylation. In proteins that have segments extending...
co-factor are activated to become active components that then catalyze the next reaction in the cascade, ultimately resulting in cross-linked fibrin. Coagulation factors are generally indicated by Roman numerals, with a lowercase a appended to indicate an active form.
The coagulation factors are generally serine protease
Serine protease
Serine proteases are enzymes that cleave peptide bonds in proteins, in which serine serves as the nucleophilic amino acid at the active site.They are found ubiquitously in both eukaryotes and prokaryotes...
s (enzymes). There are some exceptions. For example, FVIII and FV are glycoproteins, and Factor XIII is a transglutaminase
Transglutaminase
Transglutaminases are a family of enzymes that catalyze the formation of a covalent bond between a free amine group and the gamma-carboxamid group of protein- or peptide-bound glutamine. Bonds formed by transglutaminase exhibit high resistance to proteolytic degradation.Transglutaminases were...
. Serine proteases act by cleaving other proteins at specific serine residues. The coagulation factors circulate as inactive zymogens.
The coagulation cascade is classically divided into three pathways. The tissue factor and contact activation pathways both activate the "final common pathway" of factor X, thrombin and fibrin.
Tissue factor pathway (extrinsic)
The main role of the tissue factor pathway is to generate a "thrombin burst," a process by which thrombinThrombin
Thrombin is a "trypsin-like" serine protease protein that in humans is encoded by the F2 gene. Prothrombin is proteolytically cleaved to form thrombin in the first step of the coagulation cascade, which ultimately results in the stemming of blood loss...
, the most important constituent of the coagulation cascade in terms of its feedback activation roles, is released instantaneously. FVIIa circulates in a higher amount than any other activated coagulation factor.
- Following damage to the blood vessel, FVII leaves the circulation and comes into contact with tissue factorTissue factorTissue factor, also called platelet tissue factor, factor III, thrombokinase, or CD142 is a protein present in subendothelial tissue, platelets, and leukocytes necessary for the initiation of thrombin formation from the zymogen prothrombin. An incorrect synonym is thromboplastin...
(TF) expressed on tissue-factor-bearing cells (stromaStromal cellIn cell biology, stromal cells are connective tissue cells of any organ, for example in the uterine mucosa , prostate, bone marrow, and the ovary. They are cells that support the function of the parenchymal cells of that organ...
l fibroblasts and leukocytes), forming an activated complex (TF-FVIIa). - TF-FVIIa activates FIX and FX.
- FVII is itself activated by thrombin, FXIa, FXII and FXa.
- The activation of FX (to form FXa) by TF-FVIIa is almost immediately inhibited by tissue factor pathway inhibitorTissue factor pathway inhibitorTissue factor pathway inhibitor is a single-chain polypeptide which can reversibly inhibit Factor Xa and Thrombin...
(TFPI). - FXa and its co-factor FVa form the prothrombinaseProthrombinaseThe prothrombinase complex consists of the serine protease, Factor Xa, and the protein cofactor, Factor Va. The complex assembles on negatively charged phospholipid membranes in the presence of calcium ions. The prothrombinase complex catalyzes the conversion of prothrombin , an inactive zymogen,...
complex, which activates prothrombin to thrombin. - Thrombin then activates other components of the coagulation cascade, including FV and FVIII (which activates FXI, which, in turn, activates FIX), and activates and releases FVIII from being bound to vWF.
- FVIIIa is the co-factor of FIXa, and together they form the "tenaseTenaseIn coagulation, the procoagulant protein factor X can be activated into factor Xa two ways. Extrinsic and intrinsic ways.The activating complexes are called tenase...
" complex, which activates FX; and so the cycle continues. ("Tenase" is a contraction of "ten" and the suffix "-ase" used for enzymes.)
Contact activation pathway (intrinsic)
The contact activation pathway begins with formation of the primary complex on collagen
Collagen
Collagen is a group of naturally occurring proteins found in animals, especially in the flesh and connective tissues of mammals. It is the main component of connective tissue, and is the most abundant protein in mammals, making up about 25% to 35% of the whole-body protein content...
by high-molecular-weight kininogen (HMWK), prekallikrein
Prekallikrein
Prekallikrein , also known as Fletcher factor, is a 85,000 Mr serine protease that complexes with High-molecular-weight kininogen. PK is the precursor of plasma kallikrein, which is a serine protease that activates kinins. PK is cleaved to produce kallikrein by activated Factor XII . -...
, and FXII (Hageman factor). Prekallikrein
Prekallikrein
Prekallikrein , also known as Fletcher factor, is a 85,000 Mr serine protease that complexes with High-molecular-weight kininogen. PK is the precursor of plasma kallikrein, which is a serine protease that activates kinins. PK is cleaved to produce kallikrein by activated Factor XII . -...
is converted to kallikrein
Kallikrein
Kallikreins are a subgroup of serine proteases, enzymes capable of cleaving peptide bonds in proteins. In humans, plasma kallikrein has no known homologue, while tissue kallikrein-related peptidases encode a family of fifteen closely related serine proteases...
and FXII becomes FXIIa. FXIIa converts FXI into FXIa. Factor XIa activates FIX, which with its co-factor FVIIIa form the tenase
Tenase
In coagulation, the procoagulant protein factor X can be activated into factor Xa two ways. Extrinsic and intrinsic ways.The activating complexes are called tenase...
complex, which activates FX to FXa. The minor role that the contact activation pathway has in initiating clot formation can be illustrated by the fact that patients with severe deficiencies of FXII, HMWK, and prekallikrein
Prekallikrein
Prekallikrein , also known as Fletcher factor, is a 85,000 Mr serine protease that complexes with High-molecular-weight kininogen. PK is the precursor of plasma kallikrein, which is a serine protease that activates kinins. PK is cleaved to produce kallikrein by activated Factor XII . -...
do not have a bleeding disorder. Instead, contact activation system seems to be more involved in inflammation. Patients without FXII (Hageman factor) suffer from constant infections.
Final common pathway
Thrombin has a large array of functions. Its primary role is the conversion of fibrinogenFibrinogen
Fibrinogen is a soluble plasma glycoprotein, synthesised by the liver, that is converted by thrombin into fibrin during blood coagulation. This is achieved through processes in the coagulation cascade that activate the zymogen prothrombin to the serine protease thrombin, which is responsible for...
to fibrin, the building block of a hemostatic plug. In addition, it activates Factors VIII and V and their inhibitor protein C
Protein C
Protein C, also known as autoprothrombin IIA and blood coagulation factor XIV, is a zymogenic protein, the activated form of which plays an important role in regulating blood clotting, inflammation, cell death and maintaining the permeability of blood vessel walls in humans and other animals...
(in the presence of thrombomodulin
Thrombomodulin
Thrombomodulin, CD141 or BDCA-3 is an integral membrane protein expressed on the surface of endothelial cells. In humans, thrombomodulin is encoded by the THBD gene...
), and it activates Factor XIII, which forms covalent bond
Covalent bond
A covalent bond is a form of chemical bonding that is characterized by the sharing of pairs of electrons between atoms. The stable balance of attractive and repulsive forces between atoms when they share electrons is known as covalent bonding....
s that crosslink the fibrin polymers that form from activated monomers.
Following activation by the contact factor or tissue factor pathways, the coagulation cascade is maintained in a prothrombotic state by the continued activation of FVIII and FIX to form the tenase
Tenase
In coagulation, the procoagulant protein factor X can be activated into factor Xa two ways. Extrinsic and intrinsic ways.The activating complexes are called tenase...
complex, until it is down-regulated by the anticoagulant pathways.
Cofactors
Various substances are required for the proper functioning of the coagulation cascade:- CalciumCalciumCalcium is the chemical element with the symbol Ca and atomic number 20. It has an atomic mass of 40.078 amu. Calcium is a soft gray alkaline earth metal, and is the fifth-most-abundant element by mass in the Earth's crust...
and phospholipidPhospholipidPhospholipids are a class of lipids that are a major component of all cell membranes as they can form lipid bilayers. Most phospholipids contain a diglyceride, a phosphate group, and a simple organic molecule such as choline; one exception to this rule is sphingomyelin, which is derived from...
(a plateletPlateletPlatelets, or thrombocytes , are small,irregularly shaped clear cell fragments , 2–3 µm in diameter, which are derived from fragmentation of precursor megakaryocytes. The average lifespan of a platelet is normally just 5 to 9 days...
membrane constituent) are required for the tenase and prothrombinase complexes to function. Calcium mediates the binding of the complexes via the terminal gamma-carboxy residues on FXa and FIXa to the phospholipid surfaces expressed by platelets, as well as procoagulant microparticles or microvesiclesMicrovesiclesMicrovesicles are fragments of plasma membrane ranging from 50 nm to 1000 nm shed from almost all cell types. Microvesicles play a role in intercellular communication and can deliver mRNA, miRNA, and proteins between cells...
shed from them. Calcium is also required at other points in the coagulation cascade. - Vitamin KVitamin KVitamin K is a group of structurally similar, fat soluble vitamins that are needed for the posttranslational modification of certain proteins required for blood coagulation and in metabolic pathways in bone and other tissue. They are 2-methyl-1,4-naphthoquinone derivatives...
is an essential factor to a hepatic gamma-glutamyl carboxylaseGamma-glutamyl carboxylaseGamma-glutamyl carboxylase is an enzyme that in humans is encoded by the GGCX gene, located on chromosome 2 at 2p12.-Function:Gamma-glutamyl carboxylase is an enzyme that catalyzes the posttranslational modification of vitamin K-dependent proteins...
that adds a carboxyl group to glutamic acidGlutamic acidGlutamic acid is one of the 20 proteinogenic amino acids, and its codons are GAA and GAG. It is a non-essential amino acid. The carboxylate anions and salts of glutamic acid are known as glutamates...
residues on factors II, VII, IX and X, as well as Protein SProtein SProtein S is a vitamin K-dependent plasma glycoprotein synthesized in the endothelium. In the circulation, Protein S exists in two forms: a free form and a complex form bound to complement protein C4b. In humans, protein S is encoded by the PROS1 gene...
, Protein C and Protein ZProtein ZProtein Z also known as PROZ is a protein which in humans is encoded by the PROZ gene.Protein Z is a member of the coagulation cascade, the group of blood proteins that leads to the formation of blood clots. It is vitamin K-dependent, and its functionality is therefore impaired in warfarin therapy...
. In adding the gamma-carboxyl group to glutamate residues on the immature clotting factors Vitamin K is itself oxidized. Another enzyme, Vitamin K epoxide reductaseVitamin K epoxide reductaseVitamin K epoxide reductase is an enzyme that reduces vitamin K after it has been oxidised in the carboxylation of glutamic acid. Its C1 subunit is the target of anticoagulant warfarin.- See also :* Oxidoreductase...
, (VKORC) reduces vitamin K back to its active form. Vitamin K epoxide reductase is pharmacologically important as a target for anticoagulant drugs warfarinWarfarinWarfarin is an anticoagulant. It is most likely to be the drug popularly referred to as a "blood thinner," yet this is a misnomer, since it does not affect the thickness or viscosity of blood...
and related coumarinCoumarinCoumarin is a fragrant chemical compound in the benzopyrone chemical class, found in many plants, notably in high concentration in the tonka bean , vanilla grass , sweet woodruff , mullein , sweet grass , cassia cinnamon and sweet clover...
s such as acenocoumarolAcenocoumarolAcenocoumarol is an anticoagulant that functions as a vitamin K antagonist . It is a derivative of coumarin and is marketed under the brand names Sintrom and Sinthrome.- Dosage :...
, phenprocoumonPhenprocoumonPhenprocoumon is an anticoagulant drug, a derivative of coumarin. It is a vitamin K antagonist that inhibits coagulation by blocking synthesis of coagulation factors II, VII, IX and X...
, and dicumarolDicumarolDicoumarol or dicumarol is an anticoagulant that functions as a vitamin K antagonist . It is also used in biochemical experiments as an inhibitor of reductases....
. These drugs create a deficiency of reduced vitamin K by blocking VKORC, thereby inhibiting maturation of clotting factors. Other deficiencies of vitamin K (e.g., in malabsorptionMalabsorptionMalabsorption is a state arising from abnormality in absorption of food nutrients across the gastrointestinal tract.Impairment can be of single or multiple nutrients depending on the abnormality...
), or disease (hepatocellular carcinomaHepatocellular carcinomaHepatocellular carcinoma is the most common type of liver cancer. Most cases of HCC are secondary to either a viral hepatitide infection or cirrhosis .Compared to other cancers, HCC is quite a rare tumor in the United States...
) impairs the function of the enzyme and leads to the formation of PIVKAs (proteins formed in vitamin K absence); this causes partial or non-gamma carboxylation, and affects the coagulation factors' ability to bind to expressed phospholipid.
Regulators
Five mechanisms keep platelet activation and the coagulation cascade in check. Abnormalities can lead to an increased tendency toward thrombosis:- Protein CProtein CProtein C, also known as autoprothrombin IIA and blood coagulation factor XIV, is a zymogenic protein, the activated form of which plays an important role in regulating blood clotting, inflammation, cell death and maintaining the permeability of blood vessel walls in humans and other animals...
is a major physiological anticoagulant. It is a vitamin K-dependent serine protease enzyme that is activated by thrombin into activated protein C (APC). Protein C is activated in a sequence that starts with Protein C and thrombin binding to a cell surface protein thrombomodulinThrombomodulinThrombomodulin, CD141 or BDCA-3 is an integral membrane protein expressed on the surface of endothelial cells. In humans, thrombomodulin is encoded by the THBD gene...
. Thrombomodulin binds these proteins in such a way that it activates Protein C. The activated form, along with protein S and a phospholipid as cofactors, degrades FVa and FVIIIa. Quantitative or qualitative deficiency of either may lead to thrombophiliaThrombophiliaThrombophilia is an abnormality of blood coagulation that increases the risk of thrombosis . Such abnormalities can be identified in 50% of people who have an episode of thrombosis that was not provoked by other causes...
(a tendency to develop thrombosis). Impaired action of Protein C (activated Protein C resistance), for example by having the "Leiden" variant of Factor VFactor V LeidenFactor V Leiden is the name given to a variant of human factor V that causes a hypercoagulability disorder. In this disorder the Leiden variant of factor V cannot be inactivated by activated protein C. Factor V Leiden is the most common hereditary hypercoagulability disorder amongst Eurasians...
or high levels of FVIII also may lead to a thrombotic tendency. - AntithrombinAntithrombinAntithrombin is a small protein molecule that inactivates several enzymes of the coagulation system. Antithrombin is a glycoprotein produced by the liver and consists of 432 amino acids. It contains three disulfide bonds and a total of four possible glycosylation sites...
is a serine protease inhibitor (serpinSerpinSerpins are a group of proteins with similar structures that were first identified as a set of proteins able to inhibit proteases. The acronym serpin was originally coined because many serpins inhibit chymotrypsin-like serine proteases .The first members of the serpin superfamily to be extensively...
) that degrades the serine proteases: thrombin, FIXa, FXa, FXIa, and FXIIa. It is constantly active, but its adhesion to these factors is increased by the presence of heparan sulfateHeparan sulfateHeparan sulfate is a linear polysaccharide found in all animal tissues. It occurs as a proteoglycan in which two or three HS chains are attached in close proximity to cell surface or extracellular matrix proteins...
(a glycosaminoglycanGlycosaminoglycanGlycosaminoglycans or mucopolysaccharides are long unbranched polysaccharides consisting of a repeating disaccharide unit. The repeating unit consists of a hexose or a hexuronic acid, linked to a hexosamine .-Production:Protein cores made in the rough endoplasmic reticulum are posttranslationally...
) or the administration of heparinHeparinHeparin , also known as unfractionated heparin, a highly sulfated glycosaminoglycan, is widely used as an injectable anticoagulant, and has the highest negative charge density of any known biological molecule...
s (different heparinoids increase affinity to FXa, thrombin, or both). Quantitative or qualitative deficiency of antithrombin (inborn or acquired, e.g., in proteinuriaProteinuriaProteinuria means the presence of anexcess of serum proteins in the urine. The protein in the urine often causes the urine to become foamy, although foamy urine may also be caused by bilirubin in the urine , retrograde ejaculation, pneumaturia due to a fistula, or drugs such as pyridium.- Causes...
) leads to thrombophilia. - Tissue factor pathway inhibitorTissue factor pathway inhibitorTissue factor pathway inhibitor is a single-chain polypeptide which can reversibly inhibit Factor Xa and Thrombin...
(TFPI) limits the action of tissue factor (TF). It also inhibits excessive TF-mediated activation of FIX and FX. - PlasminPlasminPlasmin is an important enzyme present in blood that degrades many blood plasma proteins, most notably, fibrin clots. The degradation of fibrin is termed fibrinolysis. In humans, the plasmin protein is encoded by the PLG gene.- Function :...
is generated by proteolytic cleavage of plasminogen, a plasma protein synthesized in the liver. This cleavage is catalyzed by tissue plasminogen activatorTissue plasminogen activatorTissue plasminogen activator is a protein involved in the breakdown of blood clots. It is a serine protease found on endothelial cells, the cells that line the blood vessels. As an enzyme, it catalyzes the conversion of plasminogen to plasmin, the major enzyme responsible for clot breakdown...
(t-PA), which is synthesized and secreted by endothelium. Plasmin proteolytically cleaves fibrin into fibrin degradation products that inhibit excessive fibrin formation. - ProstacyclinProstacyclinProstacyclin is a member of the family of lipid molecules known as eicosanoids.As a drug, it is also known as "epoprostenol". The terms are sometimes used interchangeably.-History:...
(PGI2) is released by endothelium and activates platelet Gs protein-linked receptors. This, in turn, activates adenylyl cyclase, which synthesizes cAMP. cAMP inhibits platelet activation by decreasing cytosolic levels of calcium and, by doing so, inhibits the release of granules that would lead to activation of additional platelets and the coagulation cascade.
Fibrinolysis
Eventually, blood clots are reorganised and resorbed by a process termed fibrinolysisFibrinolysis
Fibrinolysis is a process that prevents blood clots from growing and becoming problematic. This process has two types: primary fibrinolysis and secondary fibrinolysis...
. The main enzyme responsible for this process (plasmin
Plasmin
Plasmin is an important enzyme present in blood that degrades many blood plasma proteins, most notably, fibrin clots. The degradation of fibrin is termed fibrinolysis. In humans, the plasmin protein is encoded by the PLG gene.- Function :...
) is regulated by various activators and inhibitors.
Role in immune system
The coagulation system overlaps with the immune systemImmune system
An immune system is a system of biological structures and processes within an organism that protects against disease by identifying and killing pathogens and tumor cells. It detects a wide variety of agents, from viruses to parasitic worms, and needs to distinguish them from the organism's own...
. Coagulation can physically trap invading microbes in blood clots. Also, some products of the coagulation system can contribute to the innate immune system
Innate immune system
The innate immune system, also known as non-specific immune system and secondary line of defence, comprises the cells and mechanisms that defend the host from infection by other organisms in a non-specific manner...
by their ability to increase vascular permeability and act as chemotactic agents for phagocytic cells. In addition, some of the products of the coagulation system are directly antimicrobial
Antimicrobial
An anti-microbial is a substance that kills or inhibits the growth of microorganisms such as bacteria, fungi, or protozoans. Antimicrobial drugs either kill microbes or prevent the growth of microbes...
. For example, beta-lysine
Beta-lysine
Beta-lysine is an amino acid produced by platelets during coagulation and is directly antibacterial by causing lysis of many Gram positive bacteria by acting as a cationic detergent....
, a protein produced by platelets during coagulation, can cause lysis
Lysis
Lysis refers to the breaking down of a cell, often by viral, enzymic, or osmotic mechanisms that compromise its integrity. A fluid containing the contents of lysed cells is called a "lysate"....
of many Gram-positive bacteria by acting as a cationic detergent. Many acute-phase proteins of inflammation
Inflammation
Inflammation is part of the complex biological response of vascular tissues to harmful stimuli, such as pathogens, damaged cells, or irritants. Inflammation is a protective attempt by the organism to remove the injurious stimuli and to initiate the healing process...
are involved in the coagulation system. In addition, pathogenic bacteria may secrete agents that alter the coagulation system, e.g. coagulase
Coagulase
Coagulase is a protein produced by several microorganisms that enables the conversion of fibrinogen to fibrin. In the laboratory, it is used to distinguish between different types of Staphylococcus isolates. Coagulase negativity excludes S. aureus. That is to say, S...
and streptokinase
Streptokinase
Streptokinase , a protein secreted by several species of streptococci can bind and activate human plasminogen. SK is used as an effective and inexpensive thrombolysis medication in some cases of myocardial infarction and pulmonary embolism...
.
Testing of coagulation
Numerous tests are used to assess the function of the coagulation system:- Common: aPTTPartial thromboplastin timeThe partial thromboplastin time or activated partial thromboplastin time is a performance indicator measuring the efficacy of both the "intrinsic" and the common coagulation pathways...
, PTProthrombin timeThe prothrombin time and its derived measures of prothrombin ratio and international normalized ratio are measures of the extrinsic pathway of coagulation. This test is also called "ProTime INR" and "INR PT". They are used to determine the clotting tendency of blood, in the measure of warfarin...
(also used to determine INR), fibrinogenFibrinogenFibrinogen is a soluble plasma glycoprotein, synthesised by the liver, that is converted by thrombin into fibrin during blood coagulation. This is achieved through processes in the coagulation cascade that activate the zymogen prothrombin to the serine protease thrombin, which is responsible for...
testing (often by the Clauss method), plateletPlateletPlatelets, or thrombocytes , are small,irregularly shaped clear cell fragments , 2–3 µm in diameter, which are derived from fragmentation of precursor megakaryocytes. The average lifespan of a platelet is normally just 5 to 9 days...
count, platelet function testing (often by PFA-100PFA-100The PFA-100 is a platelet function analyser that aspirates blood in vitro from a blood specimen into disposable test cartridges through a microscopic aperture cut into a biologically active membrane at the end of a capillary...
). - Other: TCTThrombin clotting timeThe Thrombin Time , is a blood test which measures the time it takes for a clot to form in the plasma of a blood sample anticoagulant to which an excess of thrombin has been added,. This test is repeated with pooled plasma from normal patients...
, bleeding timeBleeding timeBleeding time is a medical test done on someone to assess their platelet functionThe term "template bleeding time" is used when the test is performed to standardized parameters. This makes it easier to compare data collected at different facilities....
, mixing testMixing testMixing studies are tests performed on blood plasma used to distinguish factor deficiencies from factor inhibitors, such as lupus anticoagulant, or specific factor inhibitors, such as antibodies directed against factor VIII...
(whether an abnormality corrects if the patient's plasma is mixed with normal plasma), coagulation factor assays, antiphosholipid antibodies, D-dimerD-dimerD-dimer is a fibrin degradation product , a small protein fragment present in the blood after a blood clot is degraded by fibrinolysis. It is so named because it contains two crosslinked D fragments of the fibrinogen protein....
, genetic tests (e.g. factor V LeidenFactor V LeidenFactor V Leiden is the name given to a variant of human factor V that causes a hypercoagulability disorder. In this disorder the Leiden variant of factor V cannot be inactivated by activated protein C. Factor V Leiden is the most common hereditary hypercoagulability disorder amongst Eurasians...
, prothrombin mutation G20210A), dilute Russell's viper venom timeDilute Russell's viper venom timeDilute Russell's viper venom time is a laboratory test often used for detection of lupus anticoagulant .Variations in the test can affect the results.-Mechanism:...
(dRVVT), miscellaneous platelet function tests, thromboelastographyThromboelastographyThrombelastography is a method of testing the efficiency of coagulation in the blood. It was first developed by the German Dr. Hellmut Hartert at University of Heidelberg School of Medicine in 1948...
(TEG or Sonoclot), euglobulin lysis timeEuglobulin lysis timeThe euglobulin lysis time is a test that measures overall fibrinolysis. The test is performed by mixing citrated platelet-poor plasma with acid in a glass test tube. This acidification causes the precipitation of certain clotting factors in a complex called the euglobulin fraction...
(ELT).
The contact activation (intrinsic) pathway is initiated by activation of the "contact factors" of plasma, and can be measured by the activated partial thromboplastin
Partial thromboplastin time
The partial thromboplastin time or activated partial thromboplastin time is a performance indicator measuring the efficacy of both the "intrinsic" and the common coagulation pathways...
time (aPTT) test.
The tissue factor (extrinsic) pathway is initiated by release of tissue factor
Tissue factor
Tissue factor, also called platelet tissue factor, factor III, thrombokinase, or CD142 is a protein present in subendothelial tissue, platelets, and leukocytes necessary for the initiation of thrombin formation from the zymogen prothrombin. An incorrect synonym is thromboplastin...
(a specific cellular lipoprotein), and can be measured by the prothrombin time
Prothrombin time
The prothrombin time and its derived measures of prothrombin ratio and international normalized ratio are measures of the extrinsic pathway of coagulation. This test is also called "ProTime INR" and "INR PT". They are used to determine the clotting tendency of blood, in the measure of warfarin...
(PT) test. PT results are often reported as ratio (INR value) to monitor dosing of oral anticoagulants such as warfarin
Warfarin
Warfarin is an anticoagulant. It is most likely to be the drug popularly referred to as a "blood thinner," yet this is a misnomer, since it does not affect the thickness or viscosity of blood...
.
The quantitative and qualitative screening of fibrinogen is measured by the thrombin clotting time
Thrombin clotting time
The Thrombin Time , is a blood test which measures the time it takes for a clot to form in the plasma of a blood sample anticoagulant to which an excess of thrombin has been added,. This test is repeated with pooled plasma from normal patients...
(TCT). Measurement of the exact amount of fibrinogen present in the blood is generally done using the Clauss method for fibrinogen testing. Many analysers are capable of measuring a "derived fibrinogen" level from the graph of the Prothrombin time clot.
If a coagulation factor is part of the contact activation or tissue factor pathway, a deficiency of that factor will affect only one of the tests: Thus hemophilia A, a deficiency of factor VIII, which is part of the contact activation pathway, results in an abnormally prolonged aPTT test but a normal PT test. The exceptions are prothrombin, fibrinogen, and some variants of FX that can be detected only by either aPTT or PT. If an abnormal PT or aPTT is present, additional testing will occur to determine which (if any) factor is present as aberrant concentrations.
Deficiencies of fibrinogen (quantitative or qualitative) will affect all screening tests.
Role in disease
Problems with coagulation may dispose to hemorrhage, thrombosis, and occasionally both, depending on the nature of the pathology.Platelet disorders
Platelet conditions may be congenital or acquired. Some inborn platelet pathologies are Glanzmann's thrombastheniaGlanzmann's thrombasthenia
Glanzmann's thrombasthenia is an abnormality of platelets. It is an extremely rare coagulopathy , in which the platelets lack glycoprotein IIb/IIIa...
, Bernard-Soulier syndrome
Bernard-Soulier syndrome
Bernard–Soulier syndrome , also called hemorrhagiparous thrombocytic dystrophy, is a rare autosomal recessive coagulopathy that causes a deficiency of glycoprotein Ib , the receptor for von Willebrand factor, which is important in clot formation.The incidence is estimated to be less than 1 in 1...
(abnormal glycoprotein Ib-IX-V complex), gray platelet syndrome
Gray platelet syndrome
Gray platelet syndrome , or platelet alpha-granule deficiency, is a rare congenital bleeding disorder caused by a reduction or absence of alpha-granules in blood platelets, and the release of proteins normally contained in these granules into the marrow, causing myelofibrosis.GPS is primarily...
(deficient alpha granules), and delta storage pool deficiency (deficient dense granules). Most are rare conditions. Most inborn platelet pathologies predispose to hemorrhage. Von Willebrand disease
Von Willebrand disease
von Willebrand disease is the most common hereditary coagulation abnormality described in humans, although it can also be acquired as a result of other medical conditions. It arises from a qualitative or quantitative deficiency of von Willebrand factor , a multimeric protein that is required for...
is due to deficiency or abnormal function of von Willebrand factor
Von Willebrand factor
von Willebrand factor is a blood glycoprotein involved in hemostasis. It is deficient or defective in von Willebrand disease and is involved in a large number of other diseases, including thrombotic thrombocytopenic purpura, Heyde's syndrome, and possibly hemolytic-uremic syndrome...
, and leads to a similar bleeding pattern; its milder forms are relatively common.
Decreased platelet numbers may be due to various causes, including insufficient production (e.g., in myelodysplastic syndrome
Myelodysplastic syndrome
The myelodysplastic syndromes are a diverse collection of hematological medical conditions that involve ineffective production of the myeloid class of blood cells....
or other bone marrow disorders), destruction by the immune system (immune thrombocytopenic purpura/ITP), and consumption due to various causes (thrombotic thrombocytopenic purpura
Thrombotic thrombocytopenic purpura
Thrombotic thrombocytopenic purpura is a rare disorder of the blood-coagulation system, causing extensive microscopic thromboses to form in small blood vessels throughout the body...
/TTP, hemolytic-uremic syndrome
Hemolytic-uremic syndrome
Hemolytic-uremic syndrome , abbreviated HUS, is a disease characterized by hemolytic anemia, acute renal failure and a low platelet count . It predominantly, but not exclusively, affects children. Most cases are preceded by an episode of diarrhea caused by E. coli O157:H7, which is acquired as a...
/HUS, paroxysmal nocturnal hemoglobinuria
Paroxysmal nocturnal hemoglobinuria
Paroxysmal nocturnal hemoglobinuria , sometimes referred to as Marchiafava-Micheli syndrome, is a rare, acquired, potentially life-threatening disease of the blood characterised by complement-induced intravascular hemolytic anemia , red urine and thrombosis...
/PNH, disseminated intravascular coagulation
Disseminated intravascular coagulation
Disseminated intravascular coagulation , also known as disseminated intravascular coagulopathy or consumptive coagulopathy, is a pathological activation of coagulation mechanisms that happens in response to a variety of diseases. DIC leads to the formation of small blood clots inside the blood...
/DIC, heparin-induced thrombocytopenia
Heparin-induced thrombocytopenia
Heparin-induced thrombocytopenia is the development of thrombocytopenia , due to the administration of various forms of heparin, an anticoagulant...
/HIT). Most consumptive conditions lead to platelet activation, and some are associated with thrombosis.
Disease and clinical significance of thrombosis
The best-known coagulation factor disorders are the hemophilias. The three main forms are hemophilia A (factor VIII deficiency), hemophilia B (factor IX deficiency or "Christmas disease") and hemophilia C (factor XI deficiency, mild bleeding tendency). Hemophilia A and B are X-linked recessive disorders, whereas Hemophilia C is much more rare autosomal recessive disorder most commonly seen in Ashkenazi JewsAshkenazi Jews
Ashkenazi Jews, also known as Ashkenazic Jews or Ashkenazim , are the Jews descended from the medieval Jewish communities along the Rhine in Germany from Alsace in the south to the Rhineland in the north. Ashkenaz is the medieval Hebrew name for this region and thus for Germany...
.
Von Willebrand disease
Von Willebrand disease
von Willebrand disease is the most common hereditary coagulation abnormality described in humans, although it can also be acquired as a result of other medical conditions. It arises from a qualitative or quantitative deficiency of von Willebrand factor , a multimeric protein that is required for...
(which behaves more like a platelet disorder except in severe cases), is the most common hereditary bleeding disorder and is characterized as being inherited autosomal recessive or dominant. In this disease, there is a defect in von Willebrand factor (vWF), which mediates the binding of glycoprotein Ib (GPIb) to collagen. This binding helps mediate the activation of platelets and formation of primary hemostasis.
Bernard-Soulier syndrome is a defect or deficiency in GPIb. GPIb, the receptor for vWF, can be defective and lead to lack of primary clot formation (primary hemostasis) and increased bleeding tendency. This is an autosomal recessive inherited disorder.
Thrombasthenia of Glanzman and Naegeli (Glanzmann thrombasthenia) is extremely rare. It is characterized by a defect in GPIIb/IIIa fibrinogen receptor complex. When GPIIb/IIIa receptor is dysfunctional, fibrinogen cannot cross-link platelets, which inhibits primary hemostasis. This is an autosomal recessive inherited disorder.
In liver failure
Liver failure
Acute liver failure is the appearance of severe complications rapidly after the first signs of liver disease , and indicates that the liver has sustained severe damage . The complications are hepatic encephalopathy and impaired protein synthesis...
(acute and chronic forms), there is insufficient production of coagulation factors by the liver; this may increase bleeding risk.
Deficiency of Vitamin K may also contribute to bleeding disorders because clotting factor maturation depends on Vitamin K.
Thrombosis
Thrombosis
Thrombosis is the formation of a blood clot inside a blood vessel, obstructing the flow of blood through the circulatory system. When a blood vessel is injured, the body uses platelets and fibrin to form a blood clot to prevent blood loss...
is the pathological development of blood clots. These clots may break free and become mobile, forming an embolus
Embolism
In medicine, an embolism is the event of lodging of an embolus into a narrow capillary vessel of an arterial bed which causes a blockage in a distant part of the body.Embolization is...
or grow to such a size that occludes the vessel in which it developed. An embolism
Embolism
In medicine, an embolism is the event of lodging of an embolus into a narrow capillary vessel of an arterial bed which causes a blockage in a distant part of the body.Embolization is...
is said to occur when the thrombus
Thrombus
A thrombus , or blood clot, is the final product of the blood coagulation step in hemostasis. It is achieved via the aggregation of platelets that form a platelet plug, and the activation of the humoral coagulation system...
(blood clot) becomes a mobile embolus and migrates to another part of the body, interfering with blood circulation and hence impairing organ function downstream of the occlusion. This causes ischemia
Ischemia
In medicine, ischemia is a restriction in blood supply, generally due to factors in the blood vessels, with resultant damage or dysfunction of tissue. It may also be spelled ischaemia or ischæmia...
and often leads to ischemic necrosis
Necrosis
Necrosis is the premature death of cells in living tissue. Necrosis is caused by factors external to the cell or tissue, such as infection, toxins, or trauma. This is in contrast to apoptosis, which is a naturally occurring cause of cellular death...
of tissue. Most cases of thrombosis are due to acquired extrinsic problems (surgery
Surgery
Surgery is an ancient medical specialty that uses operative manual and instrumental techniques on a patient to investigate and/or treat a pathological condition such as disease or injury, or to help improve bodily function or appearance.An act of performing surgery may be called a surgical...
, cancer
Cancer
Cancer , known medically as a malignant neoplasm, is a large group of different diseases, all involving unregulated cell growth. In cancer, cells divide and grow uncontrollably, forming malignant tumors, and invade nearby parts of the body. The cancer may also spread to more distant parts of the...
, immobility, obesity
Obesity
Obesity is a medical condition in which excess body fat has accumulated to the extent that it may have an adverse effect on health, leading to reduced life expectancy and/or increased health problems...
, economy class syndrome), but a small proportion of people harbor predisposing conditions known collectively as thrombophilia (e.g., antiphospholipid syndrome
Antiphospholipid syndrome
Antiphospholipid syndrome or antiphospholipid antibody syndrome , often also Hughes syndrome, is an autoimmune, hypercoagulable state caused by antibodies against cell-membrane phospholipids that provokes blood clots in both arteries and veins as well as pregnancy-related complications such as...
, factor V Leiden
Factor V Leiden
Factor V Leiden is the name given to a variant of human factor V that causes a hypercoagulability disorder. In this disorder the Leiden variant of factor V cannot be inactivated by activated protein C. Factor V Leiden is the most common hereditary hypercoagulability disorder amongst Eurasians...
, and various other rarer genetic disorders).
Mutations in factor XII
Factor XII
Coagulation factor XII also known as Hageman factor is a plasma protein. It is the zymogen form of factor XIIa, an enzyme of the serine protease class. In humans, factor XII is encoded by the F12 gene.- Function :...
have been associated with an asymptomatic prolongation in the clotting time and possibly a tendency toward thrombophlebitis
Thrombophlebitis
Thrombophlebitis is phlebitis related to a thrombus . When it occurs repeatedly in different locations, it is known as "Thrombophlebitis migrans" or "migrating thrombophlebitis".-Signs and symptoms:...
. Other mutations have been linked with a rare form of hereditary angioedema
Angioedema
Angioedema or Quincke's edema is the rapid swelling of the dermis, subcutaneous tissue, mucosa and submucosal tissues. It is very similar to urticaria, but urticaria, commonly known as hives, occurs in the upper dermis...
(type III).
Procoagulants
The use of adsorbent chemicals, such as zeoliteZeolite
Zeolites are microporous, aluminosilicate minerals commonly used as commercial adsorbents. The term zeolite was originally coined in 1756 by Swedish mineralogist Axel Fredrik Cronstedt, who observed that upon rapidly heating the material stilbite, it produced large amounts of steam from water that...
s, and other hemostatic agents are also used for use in sealing severe injuries quickly (such as in traumatic bleeding secondary to gunshot wounds). Thrombin and fibrin glue
Glue
This is a list of various types of glue. Historically, the term "glue" only referred to protein colloids prepared from animal flesh. The meaning has been extended to refer to any fluid adhesive....
are used surgically to treat bleeding and to thrombose aneurysms.
Desmopressin
Desmopressin
Desmopressin is a synthetic replacement for vasopressin, the hormone that reduces urine production. It may be taken nasally, intravenously, or as a tablet...
is used to improve platelet function by activating arginine vasopressin receptor 1A
Arginine vasopressin receptor 1A
Arginine vasopressin receptor 1A is one of the three major receptor types for arginine vasopressin , and is present throughout the brain, as well as in the periphery in the liver, kidney, and vasculature.Arginine vasopressin receptor 1A is also known as:* V1a vasopressin receptor* antidiuretic...
.
Coagulation factor concentrates are used to treat hemophilia, to reverse the effects of anticoagulants, and to treat bleeding in patients with impaired coagulation factor synthesis or increased consumption. Prothrombin complex concentrate
Prothrombin complex concentrate
Prothrombin Complex Concentrate is a combination of blood clotting factors II, VII, IX and X, as well as protein C and S. It reverses the effect of warfarin and is used in cases of significant bleeding in patients with a coagulopathy...
, cryoprecipitate
Cryoprecipitate
Cryoprecipitate, also called "Cryoprecipitated Antihemophilic Factor", "Cryoprecipitated AHF", and most commonly just "cryo", is a frozen blood product prepared from plasma.It is often transfused as a four to six unit pool instead of as a single product...
and fresh frozen plasma
Fresh frozen plasma
The term fresh frozen plasma refers to the liquid portion of human blood that has been frozen and preserved after a blood donation and will be used for blood transfusion...
are commonly-used coagulation factor products. Recombinant activated human factor VII
Factor VII
Factor VII is one of the proteins that causes blood to clot in the coagulation cascade. It is an enzyme of the serine protease class. A recombinant form of human factor VIIa has U.S. Food and Drug Administration approval for uncontrolled bleeding in hemophilia patients...
is increasingly popular in the treatment of major bleeding.
Tranexamic acid
Tranexamic acid
Tranexamic acid is a drug used to treat or prevent excessive blood loss during surgery and in certain other conditions...
and aminocaproic acid
Aminocaproic acid
Aminocaproic acid is a derivative and analogue of the amino acid lysine, which makes it an effective inhibitor for enzymes that bind that particular residue. Such enzymes include proteolytic enzymes like plasmin, the enzyme responsible for fibrinolysis...
inhibit fibrinolysis, and lead to a de facto reduced bleeding rate. Before its withdrawal, aprotinin
Aprotinin
The drug aprotinin , is the bovine version of the small protein basic pancreatic trypsin inhibitor, or BPTI, which inhibits trypsin and related proteolytic enzymes. Under the trade name Trasylol, aprotinin was used as a medication administered by injection to reduce bleeding during complex surgery,...
was used in some forms of major surgery to decrease bleeding risk and need for blood products.
Anticoagulants
Anticoagulants and anti-platelet agents are amongst the most commonly used medications. Anti-platelet agentsAntiplatelet drug
An antiplatelet drug is a member of a class of pharmaceuticals that decrease platelet aggregation and inhibit thrombus formation...
include aspirin
Aspirin
Aspirin , also known as acetylsalicylic acid , is a salicylate drug, often used as an analgesic to relieve minor aches and pains, as an antipyretic to reduce fever, and as an anti-inflammatory medication. It was discovered by Arthur Eichengrun, a chemist with the German company Bayer...
, clopidogrel
Clopidogrel
Clopidogrel is an oral, thienopyridine class antiplatelet agent used to inhibit blood clots in coronary artery disease, peripheral vascular disease, and cerebrovascular disease. It is marketed by Bristol-Myers Squibb and Sanofi-Aventis under the trade name Plavix. The drug works by irreversibly...
, dipyridamole
Dipyridamole
Dipyridamole is a drug that inhibits thrombus formation when given chronically and causes vasodilation when given at high doses over a short time.-Mechanism and effects:...
and ticlopidine
Ticlopidine
Ticlopidine is an antiplatelet drug in the thienopyridine family. Like clopidogrel, it is an adenosine diphosphate receptor inhibitor. It is used in patients in whom aspirin is not tolerated, or in whom dual antiplatelet therapy is desirable...
; the parenteral glycoprotein IIb/IIIa inhibitors
Glycoprotein IIb/IIIa inhibitors
In medicine, glycoprotein IIb/IIIa inhibitors, also GpIIb/IIIa inhibitors, is a class of antiplatelet agents.Several GpIIb/IIIa inhibitors exist:*abciximab *eptifibatide *tirofiban -Use:...
are used during angioplasty
Angioplasty
Angioplasty is the technique of mechanically widening a narrowed or obstructed blood vessel, the latter typically being a result of atherosclerosis. An empty and collapsed balloon on a guide wire, known as a balloon catheter, is passed into the narrowed locations and then inflated to a fixed size...
. Of the anticoagulants, warfarin
Warfarin
Warfarin is an anticoagulant. It is most likely to be the drug popularly referred to as a "blood thinner," yet this is a misnomer, since it does not affect the thickness or viscosity of blood...
(and related coumarin
Coumarin
Coumarin is a fragrant chemical compound in the benzopyrone chemical class, found in many plants, notably in high concentration in the tonka bean , vanilla grass , sweet woodruff , mullein , sweet grass , cassia cinnamon and sweet clover...
s) and heparin
Heparin
Heparin , also known as unfractionated heparin, a highly sulfated glycosaminoglycan, is widely used as an injectable anticoagulant, and has the highest negative charge density of any known biological molecule...
are the most commonly used. Warfarin affects the vitamin K-dependent clotting factors (II, VII, IX,X) , whereas heparin and related compounds increase the action of antithrombin on thrombin and factor Xa. A newer class of drugs, the direct thrombin inhibitor
Direct thrombin inhibitor
Direct thrombin inhibitors are a class of medication that act as anticoagulants by directly inhibiting the enzyme thrombin. Some are in clinical use, while others are undergoing clinical development...
s, is under development; some members are already in clinical use (such as lepirudin
Lepirudin
Lepirudin is an anticoagulant that functions as a direct thrombin inhibitor.Brand name: Refludan, Generic: Lepirudin rDNA for injection.Lepirudin is a recombinant hirudin derived from yeast cells. It is almost identical to...
). Also under development are other small molecular compounds that interfere directly with the enzymatic action of particular coagulation factors (e.g., rivaroxaban
Rivaroxaban
Rivaroxaban is an oral anticoagulant invented and manufactured by Bayer; in a number of countries it is marketed as Xarelto. In the United States, it is marketed by Janssen Pharmaceutica. It is the first available orally active direct factor Xa inhibitor. Rivaroxaban is well absorbed from the gut...
, dabigatran
Dabigatran
Dabigatran is an oral anticoagulant from the class of the direct thrombin inhibitors...
, apixaban
Apixaban
Apixaban is a compound being investigated as an anticoagulant. It is a direct factor Xa inhibitor. It is presently undergoing phase III trials in the prevention of venous thromboembolism, together with a number of related competing compounds, such as rivaroxaban...
).
Coagulation factors
| Number and/or name | Function | Associated genetic disorders |
|---|---|---|
| I (fibrinogen Fibrinogen Fibrinogen is a soluble plasma glycoprotein, synthesised by the liver, that is converted by thrombin into fibrin during blood coagulation. This is achieved through processes in the coagulation cascade that activate the zymogen prothrombin to the serine protease thrombin, which is responsible for... ) |
Forms clot (fibrin) | Congenital afibrinogenemia Congenital afibrinogenemia Congenital afibrinogenemia is a rare inherited blood disorder in which the blood does not clot normally due to a lack of or a malfunction involving fibrinogen, a protein necessary for coagulation.... , Familial renal amyloidosis Familial renal amyloidosis Familial renal amyloidosis is a form of amyloidosis primarily presenting in the kidney.It is associated with fibrinogen alpha chain, apolipoprotein A1, and lysozyme.... |
| II (prothrombin) | Its active form (IIa) activates I, V, VII, VIII, XI, XIII, protein C Protein C Protein C, also known as autoprothrombin IIA and blood coagulation factor XIV, is a zymogenic protein, the activated form of which plays an important role in regulating blood clotting, inflammation, cell death and maintaining the permeability of blood vessel walls in humans and other animals... , platelets |
Hypoprothrombinemia Hypoprothrombinemia Hypoprothrombinemia is a blood disorder in which a deficiency of prothrombin results in impaired blood clotting, leading to an increased physiological risk for bleeding, especially in the gastrointestinal system, cranial vault, and superficial integumentary system.-Causes:Hypoprothrombinemia can... , Thrombophilia Thrombophilia Thrombophilia is an abnormality of blood coagulation that increases the risk of thrombosis . Such abnormalities can be identified in 50% of people who have an episode of thrombosis that was not provoked by other causes... |
| III Tissue factor Tissue factor Tissue factor, also called platelet tissue factor, factor III, thrombokinase, or CD142 is a protein present in subendothelial tissue, platelets, and leukocytes necessary for the initiation of thrombin formation from the zymogen prothrombin. An incorrect synonym is thromboplastin... |
Co-factor of VIIa (formerly known as factor III) | |
| IV Calcium Calcium Calcium is the chemical element with the symbol Ca and atomic number 20. It has an atomic mass of 40.078 amu. Calcium is a soft gray alkaline earth metal, and is the fifth-most-abundant element by mass in the Earth's crust... |
Required for coagulation factors to bind to phospholipid (formerly known as factor IV) | |
| V Factor V Factor V is a protein of the coagulation system, rarely referred to as proaccelerin or labile factor. In contrast to most other coagulation factors, it is not enzymatically active but functions as a cofactor... (proaccelerin, labile factor) |
Co-factor of X with which it forms the prothrombinase Prothrombinase The prothrombinase complex consists of the serine protease, Factor Xa, and the protein cofactor, Factor Va. The complex assembles on negatively charged phospholipid membranes in the presence of calcium ions. The prothrombinase complex catalyzes the conversion of prothrombin , an inactive zymogen,... complex |
Activated protein C resistance Activated protein C resistance Activated protein C resistance is a hemostatic disorder characterized by a poor anticoagulant response to activated protein C . This results in an increased risk of venous thrombosis, which can cause heart attacks, strokes, and other problems with circulation.The disorder can be acquired or... |
| VI | Unassigned – old name of Factor Va | |
| VII Factor VII Factor VII is one of the proteins that causes blood to clot in the coagulation cascade. It is an enzyme of the serine protease class. A recombinant form of human factor VIIa has U.S. Food and Drug Administration approval for uncontrolled bleeding in hemophilia patients... (stable factor, proconvertin) |
Activates IX, X | congenital proconvertin/factor VII deficiency |
| VIII Factor VIII Factor VIII is an essential blood clotting factor also known as anti-hemophilic factor . In humans, Factor VIII is encoded by the F8 gene... (Antihemophilic factor A) |
Co-factor of IX with which it forms the tenase Tenase In coagulation, the procoagulant protein factor X can be activated into factor Xa two ways. Extrinsic and intrinsic ways.The activating complexes are called tenase... complex |
Haemophilia A Haemophilia A Haemophilia A is a deficiency in clotting factor VIII.Haemophilia A is inherited as an X-linked recessive trait, and thus occurs in males and in homozygous females. However, mild haemophilia A has been described in heterozygous females, presumably due to extremely unfavourable lyonization... |
| IX Factor IX Factor IX is one of the serine proteases of the coagulation system; it belongs to peptidase family S1. Deficiency of this protein causes hemophilia B. It was discovered in 1952 after a young boy named Stephen Christmas was found to be lacking this exact factor, leading to... (Antihemophilic factor B or Christmas factor) |
Activates X: forms tenase Tenase In coagulation, the procoagulant protein factor X can be activated into factor Xa two ways. Extrinsic and intrinsic ways.The activating complexes are called tenase... complex with factor VIII |
Haemophilia B Haemophilia B Haemophilia B is a blood clotting disorder caused by a mutation of the Factor IX gene, leading to a deficiency of Factor IX. It is the second most common form of haemophilia, rarer than haemophilia A. It is sometimes called Christmas disease after Stephen Christmas, the first patient described... |
| X Factor X Factor X, also known by the eponym Stuart-Prower factor or as prothrombinase, is an enzyme of the coagulation cascade. It is a serine endopeptidase .-Physiology:... (Stuart-Prower factor) |
Activates II: forms prothrombinase Prothrombinase The prothrombinase complex consists of the serine protease, Factor Xa, and the protein cofactor, Factor Va. The complex assembles on negatively charged phospholipid membranes in the presence of calcium ions. The prothrombinase complex catalyzes the conversion of prothrombin , an inactive zymogen,... complex with factor V |
Congenital Factor X deficiency |
| XI Factor XI Factor XI or plasma thromboplastin antecedent is the zymogen form of factor XIa, one of the enzymes of the coagulation cascade. Like many other coagulation factors, it is a serine protease. In humans, Factor XI is encoded by the F11 gene.... (plasma thromboplastin antecedent) |
Activates IX | Haemophilia C Haemophilia C Haemophilia C is a mild form of haemophilia affecting both sexes. However, it predominantly occurs in Jews of Ashkenazi descent. It is the fourth most common coagulation disorder after von Willebrand's disease and haemophilia A and B... |
| XII Factor XII Coagulation factor XII also known as Hageman factor is a plasma protein. It is the zymogen form of factor XIIa, an enzyme of the serine protease class. In humans, factor XII is encoded by the F12 gene.- Function :... (Hageman factor) |
Activates factor XI, VII and prekallikrein | Hereditary angioedema Hereditary angioedema Hereditary angioedema presents in the second to fourth decade, and is characterized by local swelling in subcutaneous tissues.... type III |
| XIII Factor XIII Factor XIII or fibrin stabilizing factor is an enzyme of the blood coagulation system that crosslinks fibrin.- Function :Factor XIII is a transglutaminase that circulates in the plasma as a heterotetramer of two catalytic A subunits and two carrier B subunits... (fibrin-stabilizing factor) |
Congenital Factor XIIIa/b deficiency | |
| von Willebrand factor Von Willebrand factor von Willebrand factor is a blood glycoprotein involved in hemostasis. It is deficient or defective in von Willebrand disease and is involved in a large number of other diseases, including thrombotic thrombocytopenic purpura, Heyde's syndrome, and possibly hemolytic-uremic syndrome... |
Binds to VIII, mediates platelet adhesion | von Willebrand disease Von Willebrand disease von Willebrand disease is the most common hereditary coagulation abnormality described in humans, although it can also be acquired as a result of other medical conditions. It arises from a qualitative or quantitative deficiency of von Willebrand factor , a multimeric protein that is required for... |
| prekallikrein Prekallikrein Prekallikrein , also known as Fletcher factor, is a 85,000 Mr serine protease that complexes with High-molecular-weight kininogen. PK is the precursor of plasma kallikrein, which is a serine protease that activates kinins. PK is cleaved to produce kallikrein by activated Factor XII . -... (Fletcher factor) |
Activates XII and prekallikrein; cleaves HMWK | Prekallikrein/Fletcher Factor deficiency |
| high-molecular-weight kininogen (HMWK) (Fitzgerald factor) | Supports reciprocal activation of XII, XI, and prekallikrein | Kininogen deficiency |
| fibronectin Fibronectin Fibronectin is a high-molecular weight glycoprotein of the extracellular matrix that binds to membrane-spanning receptor proteins called integrins. In addition to integrins, fibronectin also binds extracellular matrix components such as collagen, fibrin and heparan sulfate proteoglycans... |
Mediates cell adhesion | Glomerulopathy Glomerulopathy Glomerulopathy is a term used to describe a disease affecting the glomeruli of the nephron.It can refer to a process that is inflammatory or noninflammatory. Because the term "glomerulitis" exists for inflammatory conditions, "glomerulopathy" sometimes carries a noninflammatory implication.... with fibronectin deposits |
| antithrombin Antithrombin Antithrombin is a small protein molecule that inactivates several enzymes of the coagulation system. Antithrombin is a glycoprotein produced by the liver and consists of 432 amino acids. It contains three disulfide bonds and a total of four possible glycosylation sites... III |
Inhibits IIa, Xa, and other proteases | Antithrombin III deficiency Antithrombin III deficiency Antithrombin III deficiency is a rare hereditary disorder that generally comes to light when a patient suffers recurrent venous thrombosis and pulmonary embolism... |
| heparin cofactor II Heparin cofactor II Heparin cofactor II, a protein encoded by the SERPIND1 gene, is a coagulation factor that inhibits IIa, and is a cofactor for heparin and dermatan sulfate... |
Inhibits IIa, cofactor for heparin and dermatan sulfate Dermatan sulfate Dermatan sulfate is a glycosaminoglycan found mostly in skin, but also in blood vessels, heart valves, tendons, and lungs.... ("minor antithrombin") |
Heparin cofactor II deficiency |
| protein C Protein C Protein C, also known as autoprothrombin IIA and blood coagulation factor XIV, is a zymogenic protein, the activated form of which plays an important role in regulating blood clotting, inflammation, cell death and maintaining the permeability of blood vessel walls in humans and other animals... |
Inactivates Va and VIIIa | Protein C deficiency Protein C deficiency Protein C deficiency is a rare genetic trait that predisposes to thrombotic disease. It was first described in 1981. The disease belongs to a group of genetic disorders known as thrombophilias. The prevalence of protein C deficiency has been estimated to about 0.2% to 0.5% of the general population... |
| protein S Protein S Protein S is a vitamin K-dependent plasma glycoprotein synthesized in the endothelium. In the circulation, Protein S exists in two forms: a free form and a complex form bound to complement protein C4b. In humans, protein S is encoded by the PROS1 gene... |
Cofactor for activated protein C (APC, inactive when bound to C4b-binding protein) | Protein S deficiency Protein S deficiency Protein S deficiency is a disorder associated with increased risk of venous thrombosis. Protein S, a vitamin K-dependent physiological anticoagulant, acts as a nonenzymatic cofactor to activated protein C in the proteolytic degradation of factor Va and factor VIIIa... |
| protein Z Protein Z Protein Z also known as PROZ is a protein which in humans is encoded by the PROZ gene.Protein Z is a member of the coagulation cascade, the group of blood proteins that leads to the formation of blood clots. It is vitamin K-dependent, and its functionality is therefore impaired in warfarin therapy... |
Mediates thrombin adhesion to phospholipids and stimulates degradation of factor X by ZPI | Protein Z deficiency |
| Protein Z-related protease inhibitor Protein Z-related protease inhibitor Protein Z-dependent protease inhibitor is a protein circulating in the blood which inhibits factors Xa and XIa of the coagulation cascade. It is a member of the class of the serine protease inhibitors... (ZPI) |
Degrades factors X (in presence of protein Z) and XI (independently) | |
| plasminogen | Converts to plasmin, lyses fibrin and other proteins | Plasminogen deficiency, type I (ligneous conjunctivitis) |
| alpha 2-antiplasmin Alpha 2-antiplasmin Alpha 2-antiplasmin is a serine protease inhibitor responsible for inactivating plasmin, an important enzyme that participates in fibrinolysis and degradation of various other proteins... |
Inhibits plasmin | Antiplasmin deficiency |
| tissue plasminogen activator Tissue plasminogen activator Tissue plasminogen activator is a protein involved in the breakdown of blood clots. It is a serine protease found on endothelial cells, the cells that line the blood vessels. As an enzyme, it catalyzes the conversion of plasminogen to plasmin, the major enzyme responsible for clot breakdown... (tPA) |
Activates plasminogen | Familial hyperfibrinolysis Hyperfibrinolysis The fibrinolysis system is responsible for removing blood clots. Hyperfibrinolysis describes a situation with markedly enhanced fibrinolytic activity, resulting in increased, sometimes catastrophic bleeding. Hyperfibrinolysis can be caused by acquired or congenital reasons... and thrombophilia Thrombophilia Thrombophilia is an abnormality of blood coagulation that increases the risk of thrombosis . Such abnormalities can be identified in 50% of people who have an episode of thrombosis that was not provoked by other causes... |
| urokinase Urokinase Urokinase , also called urokinase-type plasminogen activator , is a serine protease . Urokinase was originally isolated from human urine, but is present in several physiological locations, such as blood stream and the extracellular matrix... |
Activates plasminogen | Quebec platelet disorder Quebec Platelet Disorder Quebec Platelet Disorder is a rare, autosomal dominant bleeding disorder described in a family from the province of Quebec in Canada.-Pathophysiology:... |
| plasminogen activator inhibitor-1 Plasminogen activator inhibitor-1 Plasminogen activator inhibitor-1 also known as endothelial plasminogen activator inhibitor or serpin E1 is a protein that in humans is encoded by the SERPINE1 gene.... (PAI1) |
Inactivates tPA & urokinase (endothelial PAI) | Plasminogen activator inhibitor-1 deficiency |
| plasminogen activator inhibitor-2 Plasminogen activator inhibitor-2 Plasminogen activator inhibitor-2 is a coagulation factor that inactivates tPA and urokinase. It is present in most cells, especially monocytes/macrophages... (PAI2) |
Inactivates tPA & urokinase (placenta Placenta The placenta is an organ that connects the developing fetus to the uterine wall to allow nutrient uptake, waste elimination, and gas exchange via the mother's blood supply. "True" placentas are a defining characteristic of eutherian or "placental" mammals, but are also found in some snakes and... l PAI) |
|
| cancer procoagulant Cancer procoagulant Cancer procoagulant is a hypothesised protein, most likely a cysteine protease enzyme , that occurs only in fetal and malignant cells. Its activity appears to be the activation of factor X, one of the coagulation factors, and would account for the increased incidence of thrombosis in cancer patients... |
Pathological factor X Factor X Factor X, also known by the eponym Stuart-Prower factor or as prothrombinase, is an enzyme of the coagulation cascade. It is a serine endopeptidase .-Physiology:... activator linked to thrombosis in cancer Cancer Cancer , known medically as a malignant neoplasm, is a large group of different diseases, all involving unregulated cell growth. In cancer, cells divide and grow uncontrollably, forming malignant tumors, and invade nearby parts of the body. The cancer may also spread to more distant parts of the... |
Initial discoveries
Theories on the coagulation of blood have existed since antiquity. Physiologist Johannes MüllerJohannes Peter Müller
Johannes Peter Müller , was a German physiologist, comparative anatomist, and ichthyologist not only known for his discoveries but also for his ability to synthesize knowledge.-Early years and education:...
(1801–1858) described fibrin, the substance of a thrombus
Thrombus
A thrombus , or blood clot, is the final product of the blood coagulation step in hemostasis. It is achieved via the aggregation of platelets that form a platelet plug, and the activation of the humoral coagulation system...
. Its soluble precursor, fibrinogen
Fibrinogen
Fibrinogen is a soluble plasma glycoprotein, synthesised by the liver, that is converted by thrombin into fibrin during blood coagulation. This is achieved through processes in the coagulation cascade that activate the zymogen prothrombin to the serine protease thrombin, which is responsible for...
, was thus named by Rudolf Virchow
Rudolf Virchow
Rudolph Carl Virchow was a German doctor, anthropologist, pathologist, prehistorian, biologist and politician, known for his advancement of public health...
(1821–1902), and isolated chemically by Prosper Sylvain Denis (1799–1863). Alexander Schmidt
Alexander Schmidt (physiologist)
Alexander Schmidt was a Livonian physiologist. He was born on the Island of Mohn, which today is called Muhu, Estonia. In 1858, he received his medical doctorate from the University of Dorpat, and later was an assistant to Felix Hoppe-Seyler in Berlin, and Carl Ludwig in Leipzig...
suggested that the conversion from fibrinogen to fibrin is the result of an enzymatic
Enzyme
Enzymes are proteins that catalyze chemical reactions. In enzymatic reactions, the molecules at the beginning of the process, called substrates, are converted into different molecules, called products. Almost all chemical reactions in a biological cell need enzymes in order to occur at rates...
process, and labeled the hypothetical enzyme "thrombin
Thrombin
Thrombin is a "trypsin-like" serine protease protein that in humans is encoded by the F2 gene. Prothrombin is proteolytically cleaved to form thrombin in the first step of the coagulation cascade, which ultimately results in the stemming of blood loss...
" and its precursor "prothrombin". Arthus
Nicolas Maurice Arthus
Nicolas Maurice Arthus was a French immunologist and physiologist. The Arthus reaction, a localized inflammatory response, is named after him.Arthus was born January 9, 1862 in Angers, France....
discovered in 1890 that calcium was essential in coagulation. Platelet
Platelet
Platelets, or thrombocytes , are small,irregularly shaped clear cell fragments , 2–3 µm in diameter, which are derived from fragmentation of precursor megakaryocytes. The average lifespan of a platelet is normally just 5 to 9 days...
s were identified in 1865, and their function was elucidated by Giulio Bizzozero
Giulio Bizzozero
Giulio Bizzozero was an Italian doctor and medical researcher. He is known as the original discoverer of Helicobacter pylori, the bacteria which is responsible for peptic ulcer disease...
in 1882.
The theory that thrombin is generated by the presence of tissue factor
Tissue factor
Tissue factor, also called platelet tissue factor, factor III, thrombokinase, or CD142 is a protein present in subendothelial tissue, platelets, and leukocytes necessary for the initiation of thrombin formation from the zymogen prothrombin. An incorrect synonym is thromboplastin...
was consolidated by Paul Morawitz
Paul Morawitz
Paul Oskar Morawitz was a German internist and physiologist whose most important work was in studying the coagulation of blood....
in 1905. At this stage, it was known that thrombokinase/thromboplastin (factor III) is released by damaged tissues, reacting with prothrombin (II), which, together with calcium
Calcium in biology
Calcium plays a pivotal role in the physiology and biochemistry of organisms and the cell. It plays an important role in signal transduction pathways, where it acts as a second messenger, in neurotransmitter release from neurons, contraction of all muscle cell types, and fertilization...
(IV), forms thrombin, which converts fibrinogen into fibrin (I).
Coagulation factors
The remainder of the biochemical factors in the process of coagulation were largely discovered in the 20th century.A first clue as to the actual complexity of the system of coagulation was the discovery of proaccelerin (initially and later called Factor V) by Paul Owren (1905–1990) in 1947. He also postulated its function to be the generation of accelerin (Factor VI), which later turned out to be the activated form of V (or Va); hence, VI is not now in active use.
Factor VII (also known as serum prothrombin conversion accelerator or proconvertin, precipitated by barium sulfate) was discovered in a young female patient in 1949 and 1951 by different groups.
Factor VIII
Factor VIII
Factor VIII is an essential blood clotting factor also known as anti-hemophilic factor . In humans, Factor VIII is encoded by the F8 gene...
turned out to be deficient in the clinically recognised but etiologically elusive hemophilia A
Haemophilia A
Haemophilia A is a deficiency in clotting factor VIII.Haemophilia A is inherited as an X-linked recessive trait, and thus occurs in males and in homozygous females. However, mild haemophilia A has been described in heterozygous females, presumably due to extremely unfavourable lyonization...
; it was identified in the 1950s and is alternatively called antihemophilic globulin due to its capability to correct hemophilia A.
Factor IX was discovered in 1952 in a young patient with hemophilia B
Haemophilia B
Haemophilia B is a blood clotting disorder caused by a mutation of the Factor IX gene, leading to a deficiency of Factor IX. It is the second most common form of haemophilia, rarer than haemophilia A. It is sometimes called Christmas disease after Stephen Christmas, the first patient described...
named Stephen Christmas
Stephen Christmas
Stephen Christmas was the first patient described to have Christmas disease in 1952 by a group of British doctors.-Biography:...
(1947–1993). His deficiency was described by Dr. Rosemary Biggs and Professor R.G. MacFarlane in Oxford, UK. The factor is, hence, called Christmas Factor. Christmas lived in Canada, and campaigned for blood transfusion safety until succumbing to transfusion-related AIDS
AIDS
Acquired immune deficiency syndrome or acquired immunodeficiency syndrome is a disease of the human immune system caused by the human immunodeficiency virus...
at age 46. An alternative name for the factor is plasma thromboplastin component, given by an independent group in California.
Hageman factor, now known as factor XII, was identified in 1955 in an asymptomatic patient with a prolonged bleeding time named of John Hageman. Factor X, or Stuart-Prower factor, followed, in 1956. This protein was identified in a Ms. Audrey Prower of London, who had a lifelong bleeding tendency. In 1957, an American group identified the same factor in a Mr. Rufus Stuart. Factors XI and XIII were identified in 1953 and 1961, respectively.
The view that the coagulation process is a "cascade" or "waterfall" was enunciated almost simultaneously by MacFarlane in the UK and by Davie and Ratnoff in the USA, respectively.
Nomenclature
The usage of Roman numerals rather than eponyms or systematic names was agreed upon during annual conferences (starting in 1955) of hemostasis experts. In 1962, consensus was achieved on the numbering of factors I-XII. This committee evolved into the present-day International Committee on Thrombosis and Hemostasis (ICTH). Assignment of numerals ceased in 1963 after the naming of Factor XIII. The names Fletcher Factor and Fitzgerald Factor were given to further coagulation-related proteins, namely prekallikreinPrekallikrein
Prekallikrein , also known as Fletcher factor, is a 85,000 Mr serine protease that complexes with High-molecular-weight kininogen. PK is the precursor of plasma kallikrein, which is a serine protease that activates kinins. PK is cleaved to produce kallikrein by activated Factor XII . -...
and high-molecular-weight kininogen, respectively.
Factors III and VI are unassigned, as thromboplastin was never identified, and actually turned out to consist of ten further factors, and accelerin was found to be activated Factor V.
Other species
All mammals have an extremely closely related blood coagulation process, using a combined cellular and serine protease process. In fact, it is possible for any mammalian coagulation factor to "cleave" its equivalent target in any other mammal. The only nonmammalian animal known to use serine proteases for blood coagulation is the horseshoe crabHorseshoe crab
The Atlantic horseshoe crab, Limulus polyphemus, is a marine chelicerate arthropod. Despite its name, it is more closely related to spiders, ticks, and scorpions than to crabs. Horseshoe crabs are most commonly found in the Gulf of Mexico and along the northern Atlantic coast of North America...
.
3D structures
- Calculated orientations of complexes with GLA domainGla domain
Vitamin K-dependent carboxylation/gamma-carboxyglutamic domain is a protein domain that contains post-translational modifications ofmany glutamate residues by vitamin K-dependent carboxylation to form gamma-carboxyglutamate . The Gla residues are responsible for the high-affinity binding of...
s in membrane - Discoidin domain
Discoidin domain
Discoidin domain is major domain of many blood coagulation factors.Blood coagulation factors V and VIII contain a C-terminal, twice repeated, domain of about 150 amino acids, which is often called "C2-like domain"...
s of blood coagulation factors

