
Disseminated intravascular coagulation
Encyclopedia
Disseminated intravascular coagulation (DIC), also known as disseminated intravascular coagulopathy or consumptive coagulopathy, is a pathological activation of coagulation
(blood clotting) mechanisms that happens in response to a variety of diseases. DIC leads to the formation of small blood clots inside the blood vessels throughout the body. As the small clots consume coagulation proteins and platelets, normal coagulation is disrupted and abnormal bleeding
occurs from the skin (e.g. from sites where blood samples were taken), the gastrointestinal tract
, the respiratory tract
and surgical wounds. The small clots also disrupt normal blood flow to organs (such as the kidney
s), which may malfunction as a result.
DIC can occur acutely but also on a slower, chronic basis, depending on the underlying problem. It is common in the critically ill, and may participate in the development of multiple organ failure
, which may lead to death.
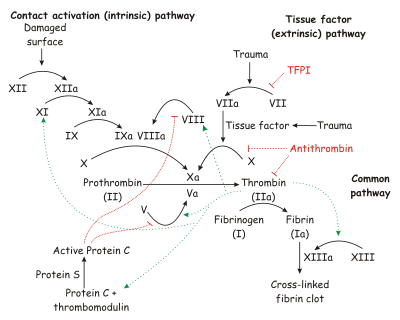
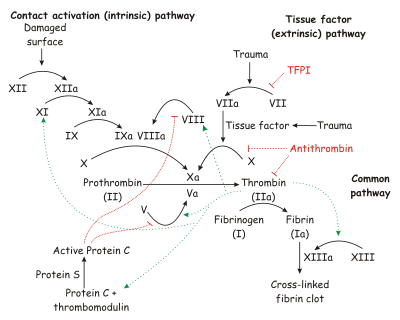 Under homeostatic conditions, the body is maintained in a finely tuned balance of coagulation and fibrinolysis. The activation of the coagulation cascade yields thrombin that converts fibrinogen to fibrin; the stable fibrin clot being the final product of hemostasis
Under homeostatic conditions, the body is maintained in a finely tuned balance of coagulation and fibrinolysis. The activation of the coagulation cascade yields thrombin that converts fibrinogen to fibrin; the stable fibrin clot being the final product of hemostasis
. The fibrinolytic system then functions to break down fibrinogen and fibrin. Activation of the fibrinolytic system generates plasmin (in the presence of thrombin), which is responsible for the lysis of fibrin clots. The breakdown of fibrinogen and fibrin results in polypeptides called fibrin degradation products (FDPs) or fibrin split products (FSPs). In a state of homeostasis, the presence of plasmin is critical, as it is the central proteolytic enzyme of coagulation and is also necessary for the breakdown of clots, or fibrinolysis.
In DIC, the processes of coagulation and fibrinolysis are dysregulated, and the result is widespread clotting with resultant bleeding. Regardless of the triggering event of DIC, once initiated, the pathophysiology of DIC is similar in all conditions. One critical mediator of DIC is the release of a transmembrane glycoprotein called tissue factor
(TF). TF is present on the surface of many cell types (including endothelial cells, macrophages, and monocytes) and is not normally in contact with the general circulation, but is exposed to the circulation after vascular damage. For example, TF is released in response to exposure to cytokines (particularly interleukin 1), tumor necrosis factor, and endotoxin
. This plays a major role in the development of DIC in septic conditions. TF is also abundant in tissues of the lungs, brain, and placenta. This helps to explain why DIC readily develops in patients with extensive trauma. Upon activation, TF binds with coagulation factors that then triggers the extrinsic pathway (via Factor VII) which subsequently triggers the intrinsic pathway (XII to XI to IX) of coagulation.
The release of endotoxin is the mechanism by which Gram-negative sepsis provokes DIC. In acute promyelocytic leukemia, treatment causes the destruction of leukemic granulocyte precursors, resulting in the release of large amounts of proteolytic enzymes from their storage granules, causing microvascular damage. Other malignancies may enhance the expression of various oncogenes that result in the release of TF and plasminogen activator inhibitor-1
(PAI-1), which prevents fibrinolysis.
Excess circulating thrombin results from the excess activation of the coagulation cascade. The excess thrombin cleaves fibrinogen, which ultimately leaves behind multiple fibrin clots in the circulation. These excess clots trap platelets to become larger clots, which leads to microvascular and macrovascular thrombosis. This lodging of clots in the microcirculation, in the large vessels, and in the organs is what leads to the ischemia, impaired organ perfusion, and end-organ damage that occurs with DIC.
Coagulation inhibitors are also consumed in this process. Decreased inhibitor levels will permit more clotting so that a feedback system develops in which increased clotting leads to more clotting. At the same time, thrombocytopenia occurs and this has been attributed to the entrapment and consumption of platelets. Clotting factors are consumed in the development of multiple clots, which contributes to the bleeding seen with DIC.
Simultaneously, excess circulating thrombin assists in the conversion of plasminogen to plasmin, resulting in fibrinolysis. The breakdown of clots results in excess amounts of FDPs, which have powerful anticoagulant properties, contributing to hemorrhage. The excess plasmin also activates the complement and kinin systems. Activation of these systems leads to many of the clinical symptoms that patients experiencing DIC exhibit, such as shock, hypotension, and increased vascular permeability. The acute form of DIC is considered an extreme expression of the intravascular coagulation process with a complete breakdown of the normal homeostatic boundaries. DIC is associated with a poor prognosis and a high mortality rate.
There has been a recent challenge however to the basic assumptions and interpretations of the pathophysiology of DIC. A study of sepsis and DIC in animal models has shown that a highly-expressed receptor on the surface of hepatocytes, termed the Ashwell-Morell receptor, is responsible for thrombocytopenia in bacteremia and sepsis due to streptococcal pneumoniae (SPN) and possibly other pathogens. The thrombocytopenia
observed in SPN sepsis was not due to increased consumption of coagulation factors such as platelets, but instead was the result of this receptor's activity enabling hepatocytes to ingest and rapidly clear platelets from circulation. By removing pro-thrombotic components before they participate in the coagulopathy of DIC, the Ashwell-Morell receptor lessens the severity of DIC, reducing thrombosis and tissue necrosis, and promoting survival. The hemorrhage observed in DIC and among some tissues lacking this receptor may thereby be secondary to increased thrombosis with loss of the mechanical vascular barrier. This discovery has possible significant clinical implications in devising new approaches to reducing the pathophysiology of DIC.
, as in endotoxic shock or amnioitic fluid embolism, or it may be insidious and chronic, as in cases of carcinomatosis.
Definitive diagnosis depends on the result of:
if counts are less than 5,000-10,000/mm3 and massive hemorrhage is occurring, and fresh frozen plasma
may be administered in an attempt to replenish coagulation factors and anti-thrombotic factors, although these are only temporizing measures and may result in the increased development of thrombosis.
DIC results in lower fibrinogen
levels (as it has all been converted to fibrin), and this can be tested for in the hospital lab
. A more specific test is for "fibrin split products" (FSPs) or "fibrin degradation products" (FDPs) which are produced when fibrin undergoes degradation when blood clots are dissolved by fibrinolysis
.
In some situations, infusion with antithrombin
may be necessary.
(clotting). The prognosis for those with DIC, regardless of cause, is often grim: Between 10% and 50% of patients will die. DIC with sepsis
(infection) has a significantly higher rate of death than DIC associated with trauma.
One alternative interpretation of the acronym, "death is coming," refers to the lack of effective treatment options, and to the significant mortality associated with severe DIC.
Coagulation
Coagulation is a complex process by which blood forms clots. It is an important part of hemostasis, the cessation of blood loss from a damaged vessel, wherein a damaged blood vessel wall is covered by a platelet and fibrin-containing clot to stop bleeding and begin repair of the damaged vessel...
(blood clotting) mechanisms that happens in response to a variety of diseases. DIC leads to the formation of small blood clots inside the blood vessels throughout the body. As the small clots consume coagulation proteins and platelets, normal coagulation is disrupted and abnormal bleeding
Bleeding
Bleeding, technically known as hemorrhaging or haemorrhaging is the loss of blood or blood escape from the circulatory system...
occurs from the skin (e.g. from sites where blood samples were taken), the gastrointestinal tract
Gastrointestinal tract
The human gastrointestinal tract refers to the stomach and intestine, and sometimes to all the structures from the mouth to the anus. ....
, the respiratory tract
Respiratory tract
In humans the respiratory tract is the part of the anatomy involved with the process of respiration.The respiratory tract is divided into 3 segments:*Upper respiratory tract: nose and nasal passages, paranasal sinuses, and throat or pharynx...
and surgical wounds. The small clots also disrupt normal blood flow to organs (such as the kidney
Kidney
The kidneys, organs with several functions, serve essential regulatory roles in most animals, including vertebrates and some invertebrates. They are essential in the urinary system and also serve homeostatic functions such as the regulation of electrolytes, maintenance of acid–base balance, and...
s), which may malfunction as a result.
DIC can occur acutely but also on a slower, chronic basis, depending on the underlying problem. It is common in the critically ill, and may participate in the development of multiple organ failure
Multiple organ dysfunction syndrome
Multiple organ dysfunction syndrome ', previously known as multiple organ failure or multisystem organ failure , is altered organ function in an acutely ill patient requiring medical intervention to achieve homeostasis...
, which may lead to death.
Pathophysiology
Hemostasis
Hemostasis or haemostasis is a process which causes bleeding to stop, meaning to keep blood within a damaged blood vessel . Most of the time this includes blood changing from a liquid to a solid state. Intact blood vessels are central to moderating blood's tendency to clot...
. The fibrinolytic system then functions to break down fibrinogen and fibrin. Activation of the fibrinolytic system generates plasmin (in the presence of thrombin), which is responsible for the lysis of fibrin clots. The breakdown of fibrinogen and fibrin results in polypeptides called fibrin degradation products (FDPs) or fibrin split products (FSPs). In a state of homeostasis, the presence of plasmin is critical, as it is the central proteolytic enzyme of coagulation and is also necessary for the breakdown of clots, or fibrinolysis.
In DIC, the processes of coagulation and fibrinolysis are dysregulated, and the result is widespread clotting with resultant bleeding. Regardless of the triggering event of DIC, once initiated, the pathophysiology of DIC is similar in all conditions. One critical mediator of DIC is the release of a transmembrane glycoprotein called tissue factor
Tissue factor
Tissue factor, also called platelet tissue factor, factor III, thrombokinase, or CD142 is a protein present in subendothelial tissue, platelets, and leukocytes necessary for the initiation of thrombin formation from the zymogen prothrombin. An incorrect synonym is thromboplastin...
(TF). TF is present on the surface of many cell types (including endothelial cells, macrophages, and monocytes) and is not normally in contact with the general circulation, but is exposed to the circulation after vascular damage. For example, TF is released in response to exposure to cytokines (particularly interleukin 1), tumor necrosis factor, and endotoxin
Endotoxin
Endotoxins are toxins associated with some Gram-negative bacteria. An "endotoxin" is a toxin that is a structural molecule of the bacteria that is recognized by the immune system.-Gram negative:...
. This plays a major role in the development of DIC in septic conditions. TF is also abundant in tissues of the lungs, brain, and placenta. This helps to explain why DIC readily develops in patients with extensive trauma. Upon activation, TF binds with coagulation factors that then triggers the extrinsic pathway (via Factor VII) which subsequently triggers the intrinsic pathway (XII to XI to IX) of coagulation.
The release of endotoxin is the mechanism by which Gram-negative sepsis provokes DIC. In acute promyelocytic leukemia, treatment causes the destruction of leukemic granulocyte precursors, resulting in the release of large amounts of proteolytic enzymes from their storage granules, causing microvascular damage. Other malignancies may enhance the expression of various oncogenes that result in the release of TF and plasminogen activator inhibitor-1
Plasminogen activator inhibitor-1
Plasminogen activator inhibitor-1 also known as endothelial plasminogen activator inhibitor or serpin E1 is a protein that in humans is encoded by the SERPINE1 gene....
(PAI-1), which prevents fibrinolysis.
Excess circulating thrombin results from the excess activation of the coagulation cascade. The excess thrombin cleaves fibrinogen, which ultimately leaves behind multiple fibrin clots in the circulation. These excess clots trap platelets to become larger clots, which leads to microvascular and macrovascular thrombosis. This lodging of clots in the microcirculation, in the large vessels, and in the organs is what leads to the ischemia, impaired organ perfusion, and end-organ damage that occurs with DIC.
Coagulation inhibitors are also consumed in this process. Decreased inhibitor levels will permit more clotting so that a feedback system develops in which increased clotting leads to more clotting. At the same time, thrombocytopenia occurs and this has been attributed to the entrapment and consumption of platelets. Clotting factors are consumed in the development of multiple clots, which contributes to the bleeding seen with DIC.
Simultaneously, excess circulating thrombin assists in the conversion of plasminogen to plasmin, resulting in fibrinolysis. The breakdown of clots results in excess amounts of FDPs, which have powerful anticoagulant properties, contributing to hemorrhage. The excess plasmin also activates the complement and kinin systems. Activation of these systems leads to many of the clinical symptoms that patients experiencing DIC exhibit, such as shock, hypotension, and increased vascular permeability. The acute form of DIC is considered an extreme expression of the intravascular coagulation process with a complete breakdown of the normal homeostatic boundaries. DIC is associated with a poor prognosis and a high mortality rate.
There has been a recent challenge however to the basic assumptions and interpretations of the pathophysiology of DIC. A study of sepsis and DIC in animal models has shown that a highly-expressed receptor on the surface of hepatocytes, termed the Ashwell-Morell receptor, is responsible for thrombocytopenia in bacteremia and sepsis due to streptococcal pneumoniae (SPN) and possibly other pathogens. The thrombocytopenia
Thrombocytopenia
Thrombocytopenia is a relative decrease of platelets in blood.A normal human platelet count ranges from 150,000 to 450,000 platelets per microliter of blood. These limits are determined by the 2.5th lower and upper percentile, so values outside this range do not necessarily indicate disease...
observed in SPN sepsis was not due to increased consumption of coagulation factors such as platelets, but instead was the result of this receptor's activity enabling hepatocytes to ingest and rapidly clear platelets from circulation. By removing pro-thrombotic components before they participate in the coagulopathy of DIC, the Ashwell-Morell receptor lessens the severity of DIC, reducing thrombosis and tissue necrosis, and promoting survival. The hemorrhage observed in DIC and among some tissues lacking this receptor may thereby be secondary to increased thrombosis with loss of the mechanical vascular barrier. This discovery has possible significant clinical implications in devising new approaches to reducing the pathophysiology of DIC.
Causes
DIC can occur in the following conditions:- Cancers of lungLungThe lung is the essential respiration organ in many air-breathing animals, including most tetrapods, a few fish and a few snails. In mammals and the more complex life forms, the two lungs are located near the backbone on either side of the heart...
, pancreasPancreasThe pancreas is a gland organ in the digestive and endocrine system of vertebrates. It is both an endocrine gland producing several important hormones, including insulin, glucagon, and somatostatin, as well as a digestive organ, secreting pancreatic juice containing digestive enzymes that assist...
, prostateProstateThe prostate is a compound tubuloalveolar exocrine gland of the male reproductive system in most mammals....
and stomachStomachThe stomach is a muscular, hollow, dilated part of the alimentary canal which functions as an important organ of the digestive tract in some animals, including vertebrates, echinoderms, insects , and molluscs. It is involved in the second phase of digestion, following mastication .The stomach is...
, as well as acute myeloid leukemiaAcute myeloid leukemiaAcute myeloid leukemia , also known as acute myelogenous leukemia, is a cancer of the myeloid line of blood cells, characterized by the rapid growth of abnormal white blood cells that accumulate in the bone marrow and interfere with the production of normal blood cells. AML is the most common acute...
(particularly APMLAcute promyelocytic leukemiaAcute promyelocytic leukemia is a subtype of acute myelogenous leukemia , a cancer of the blood and bone marrow. It is also known as acute progranulocytic leukemia; APL; AML with t, PML-RARA and variants; FAB subtype M3 and M3 variant.In APL, there is an abnormal accumulation of immature...
) - Obstetric: abruptio placentae, pre-eclampsiaPre-eclampsiaPre-eclampsia or preeclampsia is a medical condition in which hypertension arises in pregnancy in association with significant amounts of protein in the urine....
, amniotic fluid embolismAmniotic fluid embolismAmniotic fluid embolism is a rare and incompletely understood obstetric emergency in which amniotic fluid, fetal cells, hair, or other debris enters the mother's blood stream via the placental bed of the uterus and triggers an allergic reaction. This reaction then results in cardiorespiratory ... - Massive tissue injury: Trauma, burns, extensive surgery
- Infections: Gram-negativeGram-negativeGram-negative bacteria are bacteria that do not retain crystal violet dye in the Gram staining protocol. In a Gram stain test, a counterstain is added after the crystal violet, coloring all Gram-negative bacteria with a red or pink color...
sepsis, Neisseria meningitidisNeisseria meningitidisNeisseria meningitidis, often referred to as meningococcus, is a bacterium that can cause meningitis and other forms of meningococcal disease such as meningococcemia, a life threatening sepsis. N. meningitidis is a major cause of morbidity and mortality during childhood in industrialized countries...
, Streptococcus pneumoniaeStreptococcus pneumoniaeStreptococcus pneumoniae, or pneumococcus, is Gram-positive, alpha-hemolytic, aerotolerant anaerobic member of the genus Streptococcus. A significant human pathogenic bacterium, S...
, malariaMalariaMalaria is a mosquito-borne infectious disease of humans and other animals caused by eukaryotic protists of the genus Plasmodium. The disease results from the multiplication of Plasmodium parasites within red blood cells, causing symptoms that typically include fever and headache, in severe cases...
, histoplasmosisHistoplasmosisHistoplasmosis is a disease caused by the fungus Histoplasma capsulatum. Symptoms of this infection vary greatly, but the disease primarily affects the lungs...
, aspergillosisAspergillosisAspergillosis is the name given to a wide variety of diseases caused by fungi of the genus Aspergillus. The most common forms are allergic bronchopulmonary aspergillosis, pulmonary aspergilloma and invasive aspergillosis. Most humans inhale Aspergillus spores every day...
, Rocky mountain spotted feverRocky Mountain spotted feverRocky Mountain spotted fever is the most lethal and most frequently reported rickettsial illness in the United States. It has been diagnosed throughout the Americas. Some synonyms for Rocky Mountain spotted fever in other countries include “tick typhus,” “Tobia fever” , “São Paulo fever” or “febre... - Miscellaneous: LiverLiverThe liver is a vital organ present in vertebrates and some other animals. It has a wide range of functions, including detoxification, protein synthesis, and production of biochemicals necessary for digestion...
disease, snake bite, giant hemangiomaHemangiomaA hemangioma of infancy is a benign self-involuting tumor of endothelial cells, the cells that line blood vessels. It usually appears during the first weeks of life and sometimes resolves by age 10. In more severe case hemangioma may have permanency, if not treated by a physician...
, shock, heat stroke, vasculitisVasculitisVasculitis refers to a heterogeneous group of disorders that are characterized by inflammatory destruction of blood vessels. Both arteries and veins are affected. Lymphangitis is sometimes considered a type of vasculitis...
, aortic aneurysmAortic aneurysmAn aortic aneurysm is a general term for any swelling of the aorta to greater than 1.5 times normal, usually representing an underlying weakness in the wall of the aorta at that location...
, Serotonin syndromeSerotonin syndromeSerotonin syndrome is a potentially life-threatening adverse drug reaction that may occur following therapeutic drug use, inadvertent interactions between drugs, overdose of particular drugs, or the recreational use of certain drugs... - Viral: ArenavirusArenavirusArenavirus is a genus of virus that infects rodents and occasionally humans. At least eight Arenaviruses are known to cause human disease. The diseases derived from Arenaviruses range in severity. Aseptic meningitis, a severe human disease that causes inflammation covering the brain and spinal...
es causing Argentine hemorrhagic feverArgentine hemorrhagic feverArgentine hemorrhagic fever or O'Higgins disease, also known in Argentina as mal de los rastrojos, stubble disease, is a hemorrhagic fever and zoonotic infectious disease occurring in Argentina. It is caused by the Junín virus...
or Bolivian Hemorrhagic FeverBolivian hemorrhagic feverBolivian hemorrhagic fever , also known as black typhus or Ordog Fever, is a hemorrhagic fever and zoonotic infectious disease originating in Bolivia after infection by Machupo virus....
Signs and symptoms
The affected person is often acutely ill and shocked with widespread haemorrhage (common bleeding sites are mouth, nose and venepuncture sites), extensive bruising, renal failure and gangrene. The onset of DIC can be fulminantFulminant
Fulminant is any event or process that occurs suddenly and quickly, and is intense and severe to the point of lethality, i.e., it has an explosive character. The word comes from Latin fulmināre, to strike with lightning...
, as in endotoxic shock or amnioitic fluid embolism, or it may be insidious and chronic, as in cases of carcinomatosis.
Diagnosis
Diagnosis is usually suggested by following conditions:- Severe cases with hemorrhage: The PT and APTT are usually very prolonged and the fibrinogen level markedly reduced. High levels of fibrin degradation products, including D-dimerD-dimerD-dimer is a fibrin degradation product , a small protein fragment present in the blood after a blood clot is degraded by fibrinolysis. It is so named because it contains two crosslinked D fragments of the fibrinogen protein....
, are found owing to the intense fibrinolytic activity stimulated by the presence of fibrin in the circulation. There is severe thrombocytopenia. The blood film may show fragmented red blood cells (schistocytes). - Mild cases without bleeding: There is increased synthesis of coagulation factors and platelets. PT, APTT, and platelet counts are normal. fibrin degradation products are raised.
Definitive diagnosis depends on the result of:
- ThrombocytopeniaThrombocytopeniaThrombocytopenia is a relative decrease of platelets in blood.A normal human platelet count ranges from 150,000 to 450,000 platelets per microliter of blood. These limits are determined by the 2.5th lower and upper percentile, so values outside this range do not necessarily indicate disease...
- Prolongation of prothrombin timeProthrombin timeThe prothrombin time and its derived measures of prothrombin ratio and international normalized ratio are measures of the extrinsic pathway of coagulation. This test is also called "ProTime INR" and "INR PT". They are used to determine the clotting tendency of blood, in the measure of warfarin...
and activated partial thromboplastin time - A low fibrinogenFibrinogenFibrinogen is a soluble plasma glycoprotein, synthesised by the liver, that is converted by thrombin into fibrin during blood coagulation. This is achieved through processes in the coagulation cascade that activate the zymogen prothrombin to the serine protease thrombin, which is responsible for...
concentration - Increased levels of fibrin degradation products
Treatment
The only effective treatment is the reversal of the underlying cause. Anticoagulants are given exceedingly rarely when thrombus formation is likely to lead to imminent death (such as in coronary artery thrombosis or cerebrovascular thrombosis). Platelets may be transfusedBlood transfusion
Blood transfusion is the process of receiving blood products into one's circulation intravenously. Transfusions are used in a variety of medical conditions to replace lost components of the blood...
if counts are less than 5,000-10,000/mm3 and massive hemorrhage is occurring, and fresh frozen plasma
Fresh frozen plasma
The term fresh frozen plasma refers to the liquid portion of human blood that has been frozen and preserved after a blood donation and will be used for blood transfusion...
may be administered in an attempt to replenish coagulation factors and anti-thrombotic factors, although these are only temporizing measures and may result in the increased development of thrombosis.
DIC results in lower fibrinogen
Fibrinogen
Fibrinogen is a soluble plasma glycoprotein, synthesised by the liver, that is converted by thrombin into fibrin during blood coagulation. This is achieved through processes in the coagulation cascade that activate the zymogen prothrombin to the serine protease thrombin, which is responsible for...
levels (as it has all been converted to fibrin), and this can be tested for in the hospital lab
Medical laboratory
A medical laboratory or clinical laboratory is a laboratory where tests are done on clinical specimens in order to get information about the health of a patient as pertaining to the diagnosis, treatment, and prevention of disease.-Departments:...
. A more specific test is for "fibrin split products" (FSPs) or "fibrin degradation products" (FDPs) which are produced when fibrin undergoes degradation when blood clots are dissolved by fibrinolysis
Fibrinolysis
Fibrinolysis is a process that prevents blood clots from growing and becoming problematic. This process has two types: primary fibrinolysis and secondary fibrinolysis...
.
In some situations, infusion with antithrombin
Antithrombin
Antithrombin is a small protein molecule that inactivates several enzymes of the coagulation system. Antithrombin is a glycoprotein produced by the liver and consists of 432 amino acids. It contains three disulfide bonds and a total of four possible glycosylation sites...
may be necessary.
Prognosis
and the extent of the intravascular thrombosisThrombosis
Thrombosis is the formation of a blood clot inside a blood vessel, obstructing the flow of blood through the circulatory system. When a blood vessel is injured, the body uses platelets and fibrin to form a blood clot to prevent blood loss...
(clotting). The prognosis for those with DIC, regardless of cause, is often grim: Between 10% and 50% of patients will die. DIC with sepsis
Sepsis
Sepsis is a potentially deadly medical condition that is characterized by a whole-body inflammatory state and the presence of a known or suspected infection. The body may develop this inflammatory response by the immune system to microbes in the blood, urine, lungs, skin, or other tissues...
(infection) has a significantly higher rate of death than DIC associated with trauma.
One alternative interpretation of the acronym, "death is coming," refers to the lack of effective treatment options, and to the significant mortality associated with severe DIC.

