
Psychiatric emergency services
Encyclopedia
Emergency psychiatry is the clinical application of psychiatry
in emergency
settings. Conditions requiring psychiatric interventions may include attempted suicide
, substance abuse
, depression
, psychosis
, violence or other rapid changes in behavior
. Psychiatric emergency services are rendered by professionals in the fields of medicine
, nursing
, psychology
and social work
. The demand for emergency psychiatric services has rapidly increased throughout the world
since the 1960s
, especially in urban area
s. Care for patients in situations involving emergency psychiatry is complex.
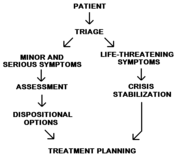
Individuals may arrive in psychiatric emergency service settings through their own voluntary request, a referral from another health professional, or through involuntary commitment
. Care of patients requiring psychiatric intervention usually encompasses crisis stabilization of many serious and potentially life-threatening conditions which could include acute or chronic mental disorders
or symptoms similar to those conditions.


suicide
, substance dependence
, alcohol intoxication, acute depression
, presence of delusion
s, violence, panic attack
s, and significant, rapid changes in behavior. Emergency psychiatry exists to identify and/or treat
these symptoms and psychiatric conditions. In addition, several rapidly lethal medical conditions present themselves with common psychiatric symptoms. A physician
's or a nurse's ability to identify and intervene with these and other medical conditions is critical.
s from a wide area of disciplines, including medicine
, nursing
, psychology
, and social work
work in these settings alongside psychiatrist
s and emergency physician
s. The facilities, sometimes housed in a psychiatric hospital
, psychiatric ward, or emergency room, provide immediate treatment to both voluntary and involuntary patients 24 hours a day, 7 days a week. Within a protected environment, psychiatric emergency services exist to provide brief stay of two or three days to gain a diagnostic clarity, find appropriate alternatives to psychiatric hospitalization for the patient, and to treat those patients whose symptoms can be improved within that brief period of time. Even precise psychiatric diagnoses are a secondary priority compared with interventions in a crisis setting. The functions of psychiatric emergency services are to assess patients' problems, implement a short-term treatment consisting of no more than ten meetings with the patient, procure a 24-hour holding area, mobilize teams to carry out interventions at patients' residences, utilize emergency management services to prevent further crises, be aware of inpatient and outpatient psychiatric resources, and provide 24/7 telephone counseling
.
the demand for emergency psychiatric services has endured a rapid growth due to deinstitutionalization both in Europe
and the United States
, increases in the number of medical specialties, and the multiplication of transitory treatment options, such as psychiatric medication
. The actual number of psychiatric emergencies has also increased significantly, especially in psychiatric emergency service settings located in urban area
s. Psychiatric emergency services attracted unemployed, homeless and other disenfranchised populations due to its characteristics of accessibility, convenience, and anonymity policies. While many of the patients who used psychiatric emergency services shared common sociological and demographic characteristics, the symptoms and needs expressed did not conform to any single psychiatric profile. The individualized care needed for patients utilizing psychiatric emergency services is evolving, requiring an always changing and sometimes complex treatment approach.
estimated one million suicides each year in the world. There are countless more suicide attempts. Psychiatric emergency service settings exist to treat the mental disorders associated with an increased risk of completed suicide or suicide attempts. Mental health professionals in these settings are expected to predict acts of violence patients may commit against themselves (or others), even though the complex factors leading to a suicide stem from so many sources, including psychosocial, biological, interpersonal, anthropological and religious. These mental health professionals will use any resources available to them to determine risk factors, make an overall assessment, and decide on any necessary treatment.
. This activation can become evident through symptoms such as the clenching of fists or jaw, pacing, slamming doors, hitting palms of hands with fists, or being easily startled. It is estimated that 17% of visits to psychiatric emergency service settings are homicidal
in origin and an additional 5% involve both suicide and homicide. Violence is also associated with many conditions such as acute intoxication, acute psychosis paranoid personality disorder
, antisocial personality disorder
, narcissistic personality disorder
, and borderline personality disorder
. Additional risk factors have also been identified which may lead to violent behavior. Such risk factors may include prior arrests, presence of hallucinations, delusions, or other neurological impairment, being uneducated, unmarried etc.. Mental health professionals complete violence risk assessments to determine both security measures and treatments for the patient.
An individual could also be suffering from an acute onset of psychosis. Such conditions can be prepared for diagnosis by obtaining a medical or psychopathological history of a patient, performing a mental status examination
, conducting psychological testing
, obtaining neuroimages
, and obtaining other neurophysiologic measurements. Following this, the mental health professional can perform a differential diagnosis
and prepare the patient for treatment. As with other patient care considerations, the origins of acute psychosis can be difficult to determine because of the mental state of the patient. However, acute psychosis is classified as a medical emergency requiring immediate and complete attention. The lack of identification and treatment can result in suicide, homicide, or other violence.
 Another common cause of psychotic symptoms is substance intoxication. These acute symptoms may resolve after a period of observation or limited psychopharmacological treatment. However the underlying issues, such as substance dependence or abuse, is difficult to treat in the emergency room. Both acute alcohol intoxication as well as other forms of substance abuse can require psychiatric interventions. Acting as a depressant
Another common cause of psychotic symptoms is substance intoxication. These acute symptoms may resolve after a period of observation or limited psychopharmacological treatment. However the underlying issues, such as substance dependence or abuse, is difficult to treat in the emergency room. Both acute alcohol intoxication as well as other forms of substance abuse can require psychiatric interventions. Acting as a depressant
of the central nervous system
, the early effects of alcohol
are usually desired for and characterized by increased talkativeness, giddiness, and a loosening of social inhibitions. Besides considerations of impaired concentration, verbal and motor performance, insight, judgment and short term memory loss which could result in behavioral change
causing injury or death, levels of alcohol below 60 milligrams per deciliter of blood are usually considered non-lethal. However, individuals at 200 milligrams per deciliter of blood are considered grossly intoxicated and concentration levels at 400 milligrams per deciliter of blood are lethal, causing complete anesthesia
of the respiratory system
. Beyond the dangerous behavioral changes that occur after the consumption of certain amounts of alcohol, idioyncratic intoxication could occur in some individuals even after the consumption of relatively small amounts of alcohol. Episodes of this impairment usually consist of confusion, disorientation, delusions and visual hallucination
s, increased aggressiveness, rage, agitation and violence. Chronic alcoholics may also suffer from alcoholic hallucinosis, wherein the cessation of prolonged drinking may trigger auditory hallucinations. Such episodes can last for a few hours or an entire week. Antipsychotic
s are often used to treat these symptoms.
Patients may also be treated for substance abuse following the administration
of psychoactive substances containing amphetamine
, caffeine
, tetrahydrocannabinol
, cocaine
, phencyclidine
s, or other inhalant
s, opioid
s, sedative
s, hypnotic
s, anxiolytic
s, psychedelics, dissociatives and deliriants
. Clinicians assessing and treating substance abusers must establish therapeutic rapport to counter denial
and other negative attitudes directed towards treatment. In addition, the clinician must determine substances used, the route of administration, dosage, and time of last use to determine the necessary short and long term treatments. An appropriate choice of treatment setting must also be determined. These settings may include outpatient facilities, partial hospitals, residential treatment centers, or hospitals. Both the immediate and long term treatment and setting is determined by the severity of dependency and seriousness of physiological complications arising from the abuse.
s, drug interaction
s, and dangerous reactions from psychiatric medications, especially antipsychotics, are considered psychiatric emergencies. Neuroleptic malignant syndrome
is a potentially lethal complication of first or second generation antipsychotics. If untreated, neuroleptic malignant syndrome can result in fever, muscle rigidity, confusion, unstable vital signs, or even death. Serotonin syndrome
can result when selective serotonin reuptake inhibitor
s or monoamine oxidase inhibitor
s mix with buspirone
. Severe symptoms of serotonin syndrome include hyperthermia
, delirium, and tachycardia
that may lead to shock. Often patients with severe general medical symptoms, such as unstable vital signs, will be transferred to a general medical emergency room or medicine service for increased monitoring.
, affectivity
, interpersonal functioning and impulse control can be considered personality disorder
s. Patients suffering from a personality disorder will usually not complain about symptoms resulting from their disorder. Patients suffering an emergency phase of a personality disorder may showcase combative or suspicious behavior, suffer from brief psychotic episodes, or be delusional. Compared with outpatient settings and the general population, the prevalence of individuals suffering from personality disorders in inpatient psychiatric settings is usually 7–25% higher. Clinicians working with such patients attempt to stabilize the individual to their baseline level of function.
or generalized anxiety disorder, or as a result of stress from such conditions as adjustment disorder
or post-traumatic stress disorder
. Clinicians usually attempt to first provide a "safe harbor" for the patient so that assessment processes and treatments can be adequately facilitated. The initiation of treatments for mood and anxiety disorders are important as patients suffering from anxiety disorders have a higher risk of premature death.
s and man-made hazards can cause severe psychological stress in victims surrounding the event. Emergency management
often includes psychiatric emergency services designed to help victims cope with the situation. The impact of disasters can cause people to feel shocked, overwhelmed, immobilized, panic-stricken, or confused. Hours, days, months and even years after a disaster, individuals can experience tormenting memories, vivid nightmares, develop apathy, withdrawal, memory lapses, fatigue, loss of appetite, insomnia, depression, irritability, panic attacks, or dysphoria. Due to the typically disorganized and hazardous environment following a disaster, mental health professionals typically assess and treat patients as rapidly as possible. Unless a condition is threatening life of the patient, or others around the patient, other medical and basic survival considerations are managed first. Soon after a disaster clinicians may make themselves available to allow individuals to ventilate to relieve feelings of isolation, helplessness and vulnerability. Dependent upon the scale of the disaster, many victims may suffer from both chronic or acute post-traumatic stress disorder
. Patients suffering severely from this disorder often are admitted to psychiatric hospitals to stabilize the individual.
, sexual abuse
or rape
can result in dangerous outcomes to the victim of the criminal act. Victims may suffer from extreme anxiety, fear, helplessness, confusion, eating or sleeping disorders, hostility, guilt and shame. Managing the response usually encompasses coordinating psychological, medical and legal considerations. Dependent upon legal requirements in the region, mental health professionals may be required to report criminal activity to a police force. Mental health professionals will usually gather identifying data during the initial assessment and refer the patient, if necessary, to receive medical treatment. Medical treatment may include a physical examination
, collection of medicolegal evidence, and determination of the risk of pregnancy
, if applicable.
. Prescribed treatments within the emergency service setting vary dependent upon the patient's condition. Different forms of psychiatric medication, psychotherapy
, or electroconvulsive therapy
may be used in the emergency setting. The introduction and efficacy of psychiatric medication as a treatment option in psychiatry has reduced the utilization of physical restraints in emergency settings, by reducing dangerous symptoms resulting from acute exacerbation of mental illness or substance intoxication.
is the movement of drugs through the body with time and is at least partially reliant upon the route of administration
, absorption
, distribution
and metabolism
of the medication. A common route of administration is oral administration, however if this method is to work the drug must be able to get to the stomach and stay there. In cases of vomiting
and nausea this method of administration is not an option. Suppositories can, in some situations, be administered instead. Medication can also be administered through intramuscular injection
, or through intravenous injection
. The amount of time required for absorption varies dependent upon many factors including drug solubility
, gastrointestinal motility
and pH
. If a medication is administered orally the amount of food
in the stomach may also affect the rate of absorption. Once absorbed medications must be distributed throughout the body, or usually with the case of psychiatric medication, past the blood-brain barrier
to the brain
. With all of these factors affecting the rapidity of effect, the time until the effects are evident varies. Generally, though, the timing with medications is relatively fast and can occur within several minutes. As an example, physicians usually expect to see a remission of symptoms thirty minutes after haloperidol
, an antipsychotic, is administered intramuscularly.
can be used to treat acute conditions or immediate problems as long as the patient understands his or her issues are psychological, the patient trusts the physician, the physician can encourage hope for change, the patient has motivation to change, the physician is aware of the psychopathological history of the patient, and the patient understands that their confidentiality will be respected. The process of brief therapy under emergency psychiatric conditions includes the establishment of a primary complaint from the patient, realizing psychosocial factors, formulating an accurate representation of the problem, coming up with ways to solve the problem, and setting specific goals. The information gathering aspect of brief psychotherapy is therapeutic because it helps the patient place his or her problem in the proper perspective. If the physician determines that deeper psychotherapy sessions are required, he or she can transition the patient out of the emergency setting and into an appropriate clinic or center.
is a controversial form of treatment which cannot be involuntarily applied in psychiatric emergency service settings. Instances wherein a patient is depressed to such a severe degree that the patient cannot be stopped from hurting himself or herself or when a patient refuses to swallow, eat or drink medication, electroconvulsive therapy could be suggested as a therapeutic alternative. While preliminary research suggests that electroconvulsive therapy may be an effective treatment for depression, it usually requires a course of six to twelve sessions of convulsions lasting at least 20 seconds for those antidepressant effects to occur.
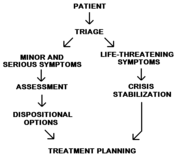 The staff will need to determine if the patient needs to be admitted to a psychiatric inpatient facility or if they can be safely discharged to the community after a period of observation and/or brief treatment. Initial emergency psychiatric evaluations usually involve patients who are acutely agitated, paranoid, or who are suicidal. Initial evaluations to determine admission and interventions are designed to be as therapeutic as possible.
The staff will need to determine if the patient needs to be admitted to a psychiatric inpatient facility or if they can be safely discharged to the community after a period of observation and/or brief treatment. Initial emergency psychiatric evaluations usually involve patients who are acutely agitated, paranoid, or who are suicidal. Initial evaluations to determine admission and interventions are designed to be as therapeutic as possible.
, or sectioning, refers to situations where police officer
s, health officers, or health professional
s classify an individual as dangerous to themselves, others, gravely disabled, or mentally ill according to the applicable government law for the region. After an individual is transported to a psychiatric emergency service setting, a preliminary professional assessment is completed which may or may not result in involuntary treatment
. Some patients may be discharged shortly after being brought to psychiatric emergency services while others will require longer observation and the need for continued involuntary commitment will exist. While some patients may initially come voluntarily, it may be realized that they pose a risk to themselves or others and involuntary commitment may be initiated at that point.
centers.
Psychiatry
Psychiatry is the medical specialty devoted to the study and treatment of mental disorders. These mental disorders include various affective, behavioural, cognitive and perceptual abnormalities...
in emergency
Emergency medicine
Emergency medicine is a medical specialty in which physicians care for patients with acute illnesses or injuries which require immediate medical attention. While not usually providing long-term or continuing care, emergency medicine physicians diagnose a variety of illnesses and undertake acute...
settings. Conditions requiring psychiatric interventions may include attempted suicide
Failed suicide attempt
Failed suicide attempts comprise a large portion of suicide attempts. Some are regarded as not true attempts at all, but rather parasuicide. The usual attempt may be a wish to affect another person by the behaviour. Consequently, it occurs in a social context and may represent a request for help....
, substance abuse
Substance abuse
A substance-related disorder is an umbrella term used to describe several different conditions associated with several different substances .A substance related disorder is a condition in which an individual uses or abuses a...
, depression
Clinical depression
Major depressive disorder is a mental disorder characterized by an all-encompassing low mood accompanied by low self-esteem, and by loss of interest or pleasure in normally enjoyable activities...
, psychosis
Psychosis
Psychosis means abnormal condition of the mind, and is a generic psychiatric term for a mental state often described as involving a "loss of contact with reality"...
, violence or other rapid changes in behavior
Behavior change
Many health conditions are caused by risk behaviors, such as problem drinking, substance use, smoking, reckless driving, overeating, or unprotected sexual intercourse. The key question in health behavior research is how to predict and modify the adoption and maintenance of health behaviors....
. Psychiatric emergency services are rendered by professionals in the fields of medicine
Medicine
Medicine is the science and art of healing. It encompasses a variety of health care practices evolved to maintain and restore health by the prevention and treatment of illness....
, nursing
Nursing
Nursing is a healthcare profession focused on the care of individuals, families, and communities so they may attain, maintain, or recover optimal health and quality of life from conception to death....
, psychology
Psychology
Psychology is the study of the mind and behavior. Its immediate goal is to understand individuals and groups by both establishing general principles and researching specific cases. For many, the ultimate goal of psychology is to benefit society...
and social work
Social work
Social Work is a professional and academic discipline that seeks to improve the quality of life and wellbeing of an individual, group, or community by intervening through research, policy, community organizing, direct practice, and teaching on behalf of those afflicted with poverty or any real or...
. The demand for emergency psychiatric services has rapidly increased throughout the world
World
World is a common name for the whole of human civilization, specifically human experience, history, or the human condition in general, worldwide, i.e. anywhere on Earth....
since the 1960s
1960s
The 1960s was the decade that started on January 1, 1960, and ended on December 31, 1969. It was the seventh decade of the 20th century.The 1960s term also refers to an era more often called The Sixties, denoting the complex of inter-related cultural and political trends across the globe...
, especially in urban area
Urban area
An urban area is characterized by higher population density and vast human features in comparison to areas surrounding it. Urban areas may be cities, towns or conurbations, but the term is not commonly extended to rural settlements such as villages and hamlets.Urban areas are created and further...
s. Care for patients in situations involving emergency psychiatry is complex.
Individuals may arrive in psychiatric emergency service settings through their own voluntary request, a referral from another health professional, or through involuntary commitment
Involuntary commitment
Involuntary commitment or civil commitment is a legal process through which an individual with symptoms of severe mental illness is court-ordered into treatment in a hospital or in the community ....
. Care of patients requiring psychiatric intervention usually encompasses crisis stabilization of many serious and potentially life-threatening conditions which could include acute or chronic mental disorders
Mental illness
A mental disorder or mental illness is a psychological or behavioral pattern generally associated with subjective distress or disability that occurs in an individual, and which is not a part of normal development or culture. Such a disorder may consist of a combination of affective, behavioural,...
or symptoms similar to those conditions.


Definition
Symptoms and conditions behind psychiatric emergencies may include attemptedParasuicide
Parasuicide refers to suicide attempts or gestures and self-harm where there is no result in death. It is a non-fatal act in which a person deliberately causes injury to himself or ingests any prescribed or generally recognised therapeutic dose in excess...
suicide
Suicide
Suicide is the act of intentionally causing one's own death. Suicide is often committed out of despair or attributed to some underlying mental disorder, such as depression, bipolar disorder, schizophrenia, alcoholism, or drug abuse...
, substance dependence
Substance dependence
The section about substance dependence in the Diagnostic and Statistical Manual of Mental Disorders does not use the word addiction at all. It explains:...
, alcohol intoxication, acute depression
Clinical depression
Major depressive disorder is a mental disorder characterized by an all-encompassing low mood accompanied by low self-esteem, and by loss of interest or pleasure in normally enjoyable activities...
, presence of delusion
Delusion
A delusion is a false belief held with absolute conviction despite superior evidence. Unlike hallucinations, delusions are always pathological...
s, violence, panic attack
Panic attack
Panic attacks are periods of intense fear or apprehension that are of sudden onset and of relatively brief duration. Panic attacks usually begin abruptly, reach a peak within 10 minutes, and subside over the next several hours...
s, and significant, rapid changes in behavior. Emergency psychiatry exists to identify and/or treat
Treatment of mental illness
Mental disorders are classified as a psychological condition marked primarily by sufficient disorganization of personality, mind, and emotions to seriously impair the normal psychological and often social functioning of the individual. Individuals diagnosed with mental disorders are typically...
these symptoms and psychiatric conditions. In addition, several rapidly lethal medical conditions present themselves with common psychiatric symptoms. A physician
Physician
A physician is a health care provider who practices the profession of medicine, which is concerned with promoting, maintaining or restoring human health through the study, diagnosis, and treatment of disease, injury and other physical and mental impairments...
's or a nurse's ability to identify and intervene with these and other medical conditions is critical.
Delivery of services
The place where emergency psychiatric services are delivered are most commonly referred to as Psychiatric Emergency Services, Psychiatric Emergency Care Centers, or Comprehensive Psychiatric Emergency Programs. Mental health professionalMental health professional
A mental health professional is a health care practitioner who offers services for the purpose of improving an individual's mental health or to treat mental illness. This broad category includes psychiatrists, clinical psychologists, clinical social workers, psychiatric nurses, mental health...
s from a wide area of disciplines, including medicine
Medicine
Medicine is the science and art of healing. It encompasses a variety of health care practices evolved to maintain and restore health by the prevention and treatment of illness....
, nursing
Nursing
Nursing is a healthcare profession focused on the care of individuals, families, and communities so they may attain, maintain, or recover optimal health and quality of life from conception to death....
, psychology
Psychology
Psychology is the study of the mind and behavior. Its immediate goal is to understand individuals and groups by both establishing general principles and researching specific cases. For many, the ultimate goal of psychology is to benefit society...
, and social work
Social work
Social Work is a professional and academic discipline that seeks to improve the quality of life and wellbeing of an individual, group, or community by intervening through research, policy, community organizing, direct practice, and teaching on behalf of those afflicted with poverty or any real or...
work in these settings alongside psychiatrist
Psychiatrist
A psychiatrist is a physician who specializes in the diagnosis and treatment of mental disorders. All psychiatrists are trained in diagnostic evaluation and in psychotherapy...
s and emergency physician
Physician
A physician is a health care provider who practices the profession of medicine, which is concerned with promoting, maintaining or restoring human health through the study, diagnosis, and treatment of disease, injury and other physical and mental impairments...
s. The facilities, sometimes housed in a psychiatric hospital
Psychiatric hospital
Psychiatric hospitals, also known as mental hospitals, are hospitals specializing in the treatment of serious mental disorders. Psychiatric hospitals vary widely in their size and grading. Some hospitals may specialise only in short-term or outpatient therapy for low-risk patients...
, psychiatric ward, or emergency room, provide immediate treatment to both voluntary and involuntary patients 24 hours a day, 7 days a week. Within a protected environment, psychiatric emergency services exist to provide brief stay of two or three days to gain a diagnostic clarity, find appropriate alternatives to psychiatric hospitalization for the patient, and to treat those patients whose symptoms can be improved within that brief period of time. Even precise psychiatric diagnoses are a secondary priority compared with interventions in a crisis setting. The functions of psychiatric emergency services are to assess patients' problems, implement a short-term treatment consisting of no more than ten meetings with the patient, procure a 24-hour holding area, mobilize teams to carry out interventions at patients' residences, utilize emergency management services to prevent further crises, be aware of inpatient and outpatient psychiatric resources, and provide 24/7 telephone counseling
Telephone counseling
Telephone counseling refers to any type of psychological service performed over the telephone. Telephone counseling ranges from individual, couple or group psychotherapy with a professional therapist to psychological first aid provided by para-professional counselors...
.
History
Since the 1960s1960s
The 1960s was the decade that started on January 1, 1960, and ended on December 31, 1969. It was the seventh decade of the 20th century.The 1960s term also refers to an era more often called The Sixties, denoting the complex of inter-related cultural and political trends across the globe...
the demand for emergency psychiatric services has endured a rapid growth due to deinstitutionalization both in Europe
Europe
Europe is, by convention, one of the world's seven continents. Comprising the westernmost peninsula of Eurasia, Europe is generally 'divided' from Asia to its east by the watershed divides of the Ural and Caucasus Mountains, the Ural River, the Caspian and Black Seas, and the waterways connecting...
and the United States
United States
The United States of America is a federal constitutional republic comprising fifty states and a federal district...
, increases in the number of medical specialties, and the multiplication of transitory treatment options, such as psychiatric medication
Psychiatric medication
A psychiatric medication is a licensed psychoactive drug taken to exert an effect on the mental state and used to treat mental disorders. Usually prescribed in psychiatric settings, these medications are typically made of synthetic chemical compounds, although some are naturally occurring, or at...
. The actual number of psychiatric emergencies has also increased significantly, especially in psychiatric emergency service settings located in urban area
Urban area
An urban area is characterized by higher population density and vast human features in comparison to areas surrounding it. Urban areas may be cities, towns or conurbations, but the term is not commonly extended to rural settlements such as villages and hamlets.Urban areas are created and further...
s. Psychiatric emergency services attracted unemployed, homeless and other disenfranchised populations due to its characteristics of accessibility, convenience, and anonymity policies. While many of the patients who used psychiatric emergency services shared common sociological and demographic characteristics, the symptoms and needs expressed did not conform to any single psychiatric profile. The individualized care needed for patients utilizing psychiatric emergency services is evolving, requiring an always changing and sometimes complex treatment approach.
Suicide attempts and suicidal thoughts
As of 2000, the World Health OrganizationWorld Health Organization
The World Health Organization is a specialized agency of the United Nations that acts as a coordinating authority on international public health. Established on 7 April 1948, with headquarters in Geneva, Switzerland, the agency inherited the mandate and resources of its predecessor, the Health...
estimated one million suicides each year in the world. There are countless more suicide attempts. Psychiatric emergency service settings exist to treat the mental disorders associated with an increased risk of completed suicide or suicide attempts. Mental health professionals in these settings are expected to predict acts of violence patients may commit against themselves (or others), even though the complex factors leading to a suicide stem from so many sources, including psychosocial, biological, interpersonal, anthropological and religious. These mental health professionals will use any resources available to them to determine risk factors, make an overall assessment, and decide on any necessary treatment.
Violent behavior
Aggression can be the result of both internal and external factors that create a measurable activation in the autonomic nervous systemAutonomic nervous system
The autonomic nervous system is the part of the peripheral nervous system that acts as a control system functioning largely below the level of consciousness, and controls visceral functions. The ANS affects heart rate, digestion, respiration rate, salivation, perspiration, diameter of the pupils,...
. This activation can become evident through symptoms such as the clenching of fists or jaw, pacing, slamming doors, hitting palms of hands with fists, or being easily startled. It is estimated that 17% of visits to psychiatric emergency service settings are homicidal
Homicide
Homicide refers to the act of a human killing another human. Murder, for example, is a type of homicide. It can also describe a person who has committed such an act, though this use is rare in modern English...
in origin and an additional 5% involve both suicide and homicide. Violence is also associated with many conditions such as acute intoxication, acute psychosis paranoid personality disorder
Paranoid personality disorder
Paranoid personality disorder is a psychiatric diagnosis characterized by paranoia and a pervasive, long-standing suspiciousness and generalized mistrust of others....
, antisocial personality disorder
Antisocial personality disorder
Antisocial personality disorder is described by the American Psychiatric Association's Diagnostic and Statistical Manual, fourth edition , as an Axis II personality disorder characterized by "...a pervasive pattern of disregard for, and violation of, the rights of others that begins in childhood...
, narcissistic personality disorder
Narcissistic personality disorder
Narcissistic personality disorder is a personality disorder in which the individual is described as being excessively preoccupied with issues of personal adequacy, power, prestige and vanity...
, and borderline personality disorder
Borderline personality disorder
Borderline personality disorder is a personality disorder described as a prolonged disturbance of personality function in a person , characterized by depth and variability of moods.The disorder typically involves unusual levels of instability in mood; black and white thinking, or splitting; the...
. Additional risk factors have also been identified which may lead to violent behavior. Such risk factors may include prior arrests, presence of hallucinations, delusions, or other neurological impairment, being uneducated, unmarried etc.. Mental health professionals complete violence risk assessments to determine both security measures and treatments for the patient.
Psychosis
Patients with psychotic symptoms are common in psychiatric emergency service settings. The determination of the source of the psychosis can be difficult. Sometimes patients brought into the setting in a psychotic state have been disconnected from their previous treatment plan. While the psychiatric emergency service setting will not be able to provide long term care for these types of patients, it can exist to provide a brief respite and reconnect the patient to their case manager and/or reintroduce necessary psychiatric medication. A visit to a crisis unit by a patient suffering from a chronic mental disorder may also indicate the existence of an undiscovered precipitant, such as change in the lifestyle of the individual, or a shifting medical condition. These considerations can play a part in an improvement to an existing treatment plan.An individual could also be suffering from an acute onset of psychosis. Such conditions can be prepared for diagnosis by obtaining a medical or psychopathological history of a patient, performing a mental status examination
Mental status examination
The mental status examination in the USA or mental state examination in the rest of the world, abbreviated MSE, is an important part of the clinical assessment process in psychiatric practice...
, conducting psychological testing
Psychological testing
Psychological testing is a field characterized by the use of samples of behavior in order to assess psychological construct, such as cognitive and emotional functioning, about a given individual. The technical term for the science behind psychological testing is psychometrics...
, obtaining neuroimages
Neuroimaging
Neuroimaging includes the use of various techniques to either directly or indirectly image the structure, function/pharmacology of the brain...
, and obtaining other neurophysiologic measurements. Following this, the mental health professional can perform a differential diagnosis
Differential diagnosis
A differential diagnosis is a systematic diagnostic method used to identify the presence of an entity where multiple alternatives are possible , and may also refer to any of the included candidate alternatives A differential diagnosis (sometimes abbreviated DDx, ddx, DD, D/Dx, or ΔΔ) is a...
and prepare the patient for treatment. As with other patient care considerations, the origins of acute psychosis can be difficult to determine because of the mental state of the patient. However, acute psychosis is classified as a medical emergency requiring immediate and complete attention. The lack of identification and treatment can result in suicide, homicide, or other violence.
Substance dependence, abuse and intoxication

Depressant
A depressant, or central depressant, is a drug or endogenous compound that depresses the function or activity of a specific part of the brain...
of the central nervous system
Central nervous system
The central nervous system is the part of the nervous system that integrates the information that it receives from, and coordinates the activity of, all parts of the bodies of bilaterian animals—that is, all multicellular animals except sponges and radially symmetric animals such as jellyfish...
, the early effects of alcohol
Ethanol
Ethanol, also called ethyl alcohol, pure alcohol, grain alcohol, or drinking alcohol, is a volatile, flammable, colorless liquid. It is a psychoactive drug and one of the oldest recreational drugs. Best known as the type of alcohol found in alcoholic beverages, it is also used in thermometers, as a...
are usually desired for and characterized by increased talkativeness, giddiness, and a loosening of social inhibitions. Besides considerations of impaired concentration, verbal and motor performance, insight, judgment and short term memory loss which could result in behavioral change
Behavior change
Many health conditions are caused by risk behaviors, such as problem drinking, substance use, smoking, reckless driving, overeating, or unprotected sexual intercourse. The key question in health behavior research is how to predict and modify the adoption and maintenance of health behaviors....
causing injury or death, levels of alcohol below 60 milligrams per deciliter of blood are usually considered non-lethal. However, individuals at 200 milligrams per deciliter of blood are considered grossly intoxicated and concentration levels at 400 milligrams per deciliter of blood are lethal, causing complete anesthesia
Anesthesia
Anesthesia, or anaesthesia , traditionally meant the condition of having sensation blocked or temporarily taken away...
of the respiratory system
Respiratory system
The respiratory system is the anatomical system of an organism that introduces respiratory gases to the interior and performs gas exchange. In humans and other mammals, the anatomical features of the respiratory system include airways, lungs, and the respiratory muscles...
. Beyond the dangerous behavioral changes that occur after the consumption of certain amounts of alcohol, idioyncratic intoxication could occur in some individuals even after the consumption of relatively small amounts of alcohol. Episodes of this impairment usually consist of confusion, disorientation, delusions and visual hallucination
Hallucination
A hallucination, in the broadest sense of the word, is a perception in the absence of a stimulus. In a stricter sense, hallucinations are defined as perceptions in a conscious and awake state in the absence of external stimuli which have qualities of real perception, in that they are vivid,...
s, increased aggressiveness, rage, agitation and violence. Chronic alcoholics may also suffer from alcoholic hallucinosis, wherein the cessation of prolonged drinking may trigger auditory hallucinations. Such episodes can last for a few hours or an entire week. Antipsychotic
Antipsychotic
An antipsychotic is a tranquilizing psychiatric medication primarily used to manage psychosis , particularly in schizophrenia and bipolar disorder. A first generation of antipsychotics, known as typical antipsychotics, was discovered in the 1950s...
s are often used to treat these symptoms.
Patients may also be treated for substance abuse following the administration
Route of administration
A route of administration in pharmacology and toxicology is the path by which a drug, fluid, poison, or other substance is taken into the body.-Classification:Routes of administration are usually classified by application location...
of psychoactive substances containing amphetamine
Amphetamine
Amphetamine or amfetamine is a psychostimulant drug of the phenethylamine class which produces increased wakefulness and focus in association with decreased fatigue and appetite.Brand names of medications that contain, or metabolize into, amphetamine include Adderall, Dexedrine, Dextrostat,...
, caffeine
Caffeine
Caffeine is a bitter, white crystalline xanthine alkaloid that acts as a stimulant drug. Caffeine is found in varying quantities in the seeds, leaves, and fruit of some plants, where it acts as a natural pesticide that paralyzes and kills certain insects feeding on the plants...
, tetrahydrocannabinol
Tetrahydrocannabinol
Tetrahydrocannabinol , also known as delta-9-tetrahydrocannabinol , Δ1-THC , or dronabinol, is the main chemical psychoactive substance found in the cannabis plant. It was first isolated in 1964. In pure form, it is a glassy solid when cold, and becomes viscous and sticky if warmed...
, cocaine
Cocaine
Cocaine is a crystalline tropane alkaloid that is obtained from the leaves of the coca plant. The name comes from "coca" in addition to the alkaloid suffix -ine, forming cocaine. It is a stimulant of the central nervous system, an appetite suppressant, and a topical anesthetic...
, phencyclidine
Phencyclidine
Phencyclidine , commonly initialized as PCP and known colloquially as angel dust, is a recreational dissociative drug...
s, or other inhalant
Inhalant
Inhalants are a broad range of drugs whose volatile vapors are taken in via the nose and trachea. They are taken by volatilization, and do not include drugs that are inhaled after burning or heating...
s, opioid
Opioid
An opioid is a psychoactive chemical that works by binding to opioid receptors, which are found principally in the central and peripheral nervous system and the gastrointestinal tract...
s, sedative
Sedative
A sedative or tranquilizer is a substance that induces sedation by reducing irritability or excitement....
s, hypnotic
Hypnotic
Hypnotic drugs are a class of psychoactives whose primary function is to induce sleep and to be used in the treatment of insomnia and in surgical anesthesia...
s, anxiolytic
Anxiolytic
An anxiolytic is a drug used for the treatment of anxiety, and its related psychological and physical symptoms...
s, psychedelics, dissociatives and deliriants
Psychedelics, dissociatives and deliriants
This general group of pharmacological agents can be divided into three broad categories: psychedelics, dissociatives, and deliriants. These classes of psychoactive drugs have in common that they can cause subjective changes in perception, thought, emotion and consciousness...
. Clinicians assessing and treating substance abusers must establish therapeutic rapport to counter denial
Denial
Denial is a defense mechanism postulated by Sigmund Freud, in which a person is faced with a fact that is too uncomfortable to accept and rejects it instead, insisting that it is not true despite what may be overwhelming evidence.The subject may use:* simple denial: deny the reality of the...
and other negative attitudes directed towards treatment. In addition, the clinician must determine substances used, the route of administration, dosage, and time of last use to determine the necessary short and long term treatments. An appropriate choice of treatment setting must also be determined. These settings may include outpatient facilities, partial hospitals, residential treatment centers, or hospitals. Both the immediate and long term treatment and setting is determined by the severity of dependency and seriousness of physiological complications arising from the abuse.
Hazardous drug reactions and interactions
OverdoseDrug overdose
The term drug overdose describes the ingestion or application of a drug or other substance in quantities greater than are recommended or generally practiced...
s, drug interaction
Drug interaction
A drug interaction is a situation in which a substance affects the activity of a drug, i.e. the effects are increased or decreased, or they produce a new effect that neither produces on its own. Typically, interaction between drugs come to mind...
s, and dangerous reactions from psychiatric medications, especially antipsychotics, are considered psychiatric emergencies. Neuroleptic malignant syndrome
Neuroleptic malignant syndrome
Neuroleptic malignant syndrome is a life- threatening neurological disorder most often caused by an adverse reaction to neuroleptic or antipsychotic drugs...
is a potentially lethal complication of first or second generation antipsychotics. If untreated, neuroleptic malignant syndrome can result in fever, muscle rigidity, confusion, unstable vital signs, or even death. Serotonin syndrome
Serotonin syndrome
Serotonin syndrome is a potentially life-threatening adverse drug reaction that may occur following therapeutic drug use, inadvertent interactions between drugs, overdose of particular drugs, or the recreational use of certain drugs...
can result when selective serotonin reuptake inhibitor
Selective serotonin reuptake inhibitor
Selective serotonin re-uptake inhibitors or serotonin-specific reuptake inhibitor are a class of compounds typically used as antidepressants in the treatment of depression, anxiety disorders, and some personality disorders. The efficacy of SSRIs is disputed...
s or monoamine oxidase inhibitor
Monoamine oxidase inhibitor
Monoamine oxidase inhibitors are a class of antidepressant drugs prescribed for the treatment of depression. They are particularly effective in treating atypical depression....
s mix with buspirone
Buspirone
Buspirone is an anxiolytic psychoactive drug of the azapirone chemical class, and is primarily used to treat generalized anxiety disorder Bristol-Myers Squibb gained FDA approval of buspirone in 1986 for treatment of GAD...
. Severe symptoms of serotonin syndrome include hyperthermia
Hyperthermia
Hyperthermia is an elevated body temperature due to failed thermoregulation. Hyperthermia occurs when the body produces or absorbs more heat than it can dissipate...
, delirium, and tachycardia
Tachycardia
Tachycardia comes from the Greek words tachys and kardia . Tachycardia typically refers to a heart rate that exceeds the normal range for a resting heart rate...
that may lead to shock. Often patients with severe general medical symptoms, such as unstable vital signs, will be transferred to a general medical emergency room or medicine service for increased monitoring.
Personality disorders
Disorders manifesting dysfunction in areas related to cognitionCognition
In science, cognition refers to mental processes. These processes include attention, remembering, producing and understanding language, solving problems, and making decisions. Cognition is studied in various disciplines such as psychology, philosophy, linguistics, and computer science...
, affectivity
Affect (psychology)
Affect refers to the experience of feeling or emotion. Affect is a key part of the process of an organism's interaction with stimuli. The word also refers sometimes to affect display, which is "a facial, vocal, or gestural behavior that serves as an indicator of affect" .The affective domain...
, interpersonal functioning and impulse control can be considered personality disorder
Personality disorder
Personality disorders, formerly referred to as character disorders, are a class of personality types and behaviors. Personality disorders are noted on Axis II of the Diagnostic and Statistical Manual of Mental Disorders or DSM-IV-TR of the American Psychiatric Association.Personality disorders are...
s. Patients suffering from a personality disorder will usually not complain about symptoms resulting from their disorder. Patients suffering an emergency phase of a personality disorder may showcase combative or suspicious behavior, suffer from brief psychotic episodes, or be delusional. Compared with outpatient settings and the general population, the prevalence of individuals suffering from personality disorders in inpatient psychiatric settings is usually 7–25% higher. Clinicians working with such patients attempt to stabilize the individual to their baseline level of function.
Anxiety
Patients suffering from an extreme case of anxiety may seek treatment when all support systems have been exhausted and they are unable to bear the anxiety. Feelings of anxiety may present in different ways from an underlying medical illness or psychiatric disorder, a secondary functional disturbance from another psychiatric disorder, from a primary psychiatric disorder such as panic disorderPanic disorder
Panic disorder is an anxiety disorder characterized by recurring severe panic attacks. It may also include significant behavioral change lasting at least a month and of ongoing worry about the implications or concern about having other attacks. The latter are called anticipatory attacks...
or generalized anxiety disorder, or as a result of stress from such conditions as adjustment disorder
Adjustment disorder
Adjustment disorder is a psychological response to an identifiable stressor or group of stressors that cause significant emotional or behavioral symptoms that do not meet criteria for anxiety disorder, PTSD, or acute stress disorder...
or post-traumatic stress disorder
Post-traumatic stress disorder
Posttraumaticstress disorder is a severe anxiety disorder that can develop after exposure to any event that results in psychological trauma. This event may involve the threat of death to oneself or to someone else, or to one's own or someone else's physical, sexual, or psychological integrity,...
. Clinicians usually attempt to first provide a "safe harbor" for the patient so that assessment processes and treatments can be adequately facilitated. The initiation of treatments for mood and anxiety disorders are important as patients suffering from anxiety disorders have a higher risk of premature death.
Disasters
Natural disasterNatural disaster
A natural disaster is the effect of a natural hazard . It leads to financial, environmental or human losses...
s and man-made hazards can cause severe psychological stress in victims surrounding the event. Emergency management
Emergency management
Emergency management is the generic name of an interdisciplinary field dealing with the strategic organizational management processes used to protect critical assets of an organization from hazard risks that can cause events like disasters or catastrophes and to ensure the continuance of the...
often includes psychiatric emergency services designed to help victims cope with the situation. The impact of disasters can cause people to feel shocked, overwhelmed, immobilized, panic-stricken, or confused. Hours, days, months and even years after a disaster, individuals can experience tormenting memories, vivid nightmares, develop apathy, withdrawal, memory lapses, fatigue, loss of appetite, insomnia, depression, irritability, panic attacks, or dysphoria. Due to the typically disorganized and hazardous environment following a disaster, mental health professionals typically assess and treat patients as rapidly as possible. Unless a condition is threatening life of the patient, or others around the patient, other medical and basic survival considerations are managed first. Soon after a disaster clinicians may make themselves available to allow individuals to ventilate to relieve feelings of isolation, helplessness and vulnerability. Dependent upon the scale of the disaster, many victims may suffer from both chronic or acute post-traumatic stress disorder
Post-traumatic stress disorder
Posttraumaticstress disorder is a severe anxiety disorder that can develop after exposure to any event that results in psychological trauma. This event may involve the threat of death to oneself or to someone else, or to one's own or someone else's physical, sexual, or psychological integrity,...
. Patients suffering severely from this disorder often are admitted to psychiatric hospitals to stabilize the individual.
Abuse
Incidents of physical abusePhysical abuse
Physical abuse is abuse involving contact intended to cause feelings of intimidation, injury, or other physical suffering or bodily harm.-Forms of physical abuse:*Striking*Punching*Belting*Pushing, pulling*Slapping*Whipping*Striking with an object...
, sexual abuse
Sexual abuse
Sexual abuse, also referred to as molestation, is the forcing of undesired sexual behavior by one person upon another. When that force is immediate, of short duration, or infrequent, it is called sexual assault. The offender is referred to as a sexual abuser or molester...
or rape
Rape
Rape is a type of sexual assault usually involving sexual intercourse, which is initiated by one or more persons against another person without that person's consent. The act may be carried out by physical force, coercion, abuse of authority or with a person who is incapable of valid consent. The...
can result in dangerous outcomes to the victim of the criminal act. Victims may suffer from extreme anxiety, fear, helplessness, confusion, eating or sleeping disorders, hostility, guilt and shame. Managing the response usually encompasses coordinating psychological, medical and legal considerations. Dependent upon legal requirements in the region, mental health professionals may be required to report criminal activity to a police force. Mental health professionals will usually gather identifying data during the initial assessment and refer the patient, if necessary, to receive medical treatment. Medical treatment may include a physical examination
Physical examination
Physical examination or clinical examination is the process by which a doctor investigates the body of a patient for signs of disease. It generally follows the taking of the medical history — an account of the symptoms as experienced by the patient...
, collection of medicolegal evidence, and determination of the risk of pregnancy
Pregnancy
Pregnancy refers to the fertilization and development of one or more offspring, known as a fetus or embryo, in a woman's uterus. In a pregnancy, there can be multiple gestations, as in the case of twins or triplets...
, if applicable.
Treatment
Treatments in psychiatric emergency service settings are typically transitory in nature and only exist to provide dispositional solutions and/or to stabilize life-threatening conditions. Once stabilized, patients suffering chronic conditions may be transferred to a setting which can provide long term psychiatric rehabilitationPsychiatric rehabilitation
Psychiatric rehabilitation, also known as psychosocial rehabilitation, and usually simplified to psych rehab, is the process of restoration of community functioning and well-being of an individual who has a psychiatric disability...
. Prescribed treatments within the emergency service setting vary dependent upon the patient's condition. Different forms of psychiatric medication, psychotherapy
Psychotherapy
Psychotherapy is a general term referring to any form of therapeutic interaction or treatment contracted between a trained professional and a client or patient; family, couple or group...
, or electroconvulsive therapy
Electroconvulsive therapy
Electroconvulsive therapy , formerly known as electroshock, is a psychiatric treatment in which seizures are electrically induced in anesthetized patients for therapeutic effect. Its mode of action is unknown...
may be used in the emergency setting. The introduction and efficacy of psychiatric medication as a treatment option in psychiatry has reduced the utilization of physical restraints in emergency settings, by reducing dangerous symptoms resulting from acute exacerbation of mental illness or substance intoxication.
Medications
With time as a critical aspect of emergency psychiatry, the rapidity of effect is an important consideration. PharmacokineticsPharmacokinetics
Pharmacokinetics, sometimes abbreviated as PK, is a branch of pharmacology dedicated to the determination of the fate of substances administered externally to a living organism...
is the movement of drugs through the body with time and is at least partially reliant upon the route of administration
Route of administration
A route of administration in pharmacology and toxicology is the path by which a drug, fluid, poison, or other substance is taken into the body.-Classification:Routes of administration are usually classified by application location...
, absorption
Absorption (Pharmacokinetics)
In pharmacology , absorption is the movement of a drug into the bloodstream.Absorption involves several phases...
, distribution
Distribution (pharmacology)
Distribution in pharmacology is a branch of pharmacokinetics which describes the reversible transfer of drug from one location to another within the body....
and metabolism
Metabolism
Metabolism is the set of chemical reactions that happen in the cells of living organisms to sustain life. These processes allow organisms to grow and reproduce, maintain their structures, and respond to their environments. Metabolism is usually divided into two categories...
of the medication. A common route of administration is oral administration, however if this method is to work the drug must be able to get to the stomach and stay there. In cases of vomiting
Vomiting
Vomiting is the forceful expulsion of the contents of one's stomach through the mouth and sometimes the nose...
and nausea this method of administration is not an option. Suppositories can, in some situations, be administered instead. Medication can also be administered through intramuscular injection
Intramuscular injection
Intramuscular injection is the injection of a substance directly into a muscle. In medicine, it is one of several alternative methods for the administration of medications . It is used for particular forms of medication that are administered in small amounts...
, or through intravenous injection
Intravenous therapy
Intravenous therapy or IV therapy is the infusion of liquid substances directly into a vein. The word intravenous simply means "within a vein". Therapies administered intravenously are often called specialty pharmaceuticals...
. The amount of time required for absorption varies dependent upon many factors including drug solubility
Solubility
Solubility is the property of a solid, liquid, or gaseous chemical substance called solute to dissolve in a solid, liquid, or gaseous solvent to form a homogeneous solution of the solute in the solvent. The solubility of a substance fundamentally depends on the used solvent as well as on...
, gastrointestinal motility
Motility
Motility is a biological term which refers to the ability to move spontaneously and actively, consuming energy in the process. Most animals are motile but the term applies to single-celled and simple multicellular organisms, as well as to some mechanisms of fluid flow in multicellular organs, in...
and pH
PH
In chemistry, pH is a measure of the acidity or basicity of an aqueous solution. Pure water is said to be neutral, with a pH close to 7.0 at . Solutions with a pH less than 7 are said to be acidic and solutions with a pH greater than 7 are basic or alkaline...
. If a medication is administered orally the amount of food
Food
Food is any substance consumed to provide nutritional support for the body. It is usually of plant or animal origin, and contains essential nutrients, such as carbohydrates, fats, proteins, vitamins, or minerals...
in the stomach may also affect the rate of absorption. Once absorbed medications must be distributed throughout the body, or usually with the case of psychiatric medication, past the blood-brain barrier
Blood-brain barrier
The blood–brain barrier is a separation of circulating blood and the brain extracellular fluid in the central nervous system . It occurs along all capillaries and consists of tight junctions around the capillaries that do not exist in normal circulation. Endothelial cells restrict the diffusion...
to the brain
Brain
The brain is the center of the nervous system in all vertebrate and most invertebrate animals—only a few primitive invertebrates such as sponges, jellyfish, sea squirts and starfishes do not have one. It is located in the head, usually close to primary sensory apparatus such as vision, hearing,...
. With all of these factors affecting the rapidity of effect, the time until the effects are evident varies. Generally, though, the timing with medications is relatively fast and can occur within several minutes. As an example, physicians usually expect to see a remission of symptoms thirty minutes after haloperidol
Haloperidol
Haloperidol is a typical antipsychotic. It is in the butyrophenone class of antipsychotic medications and has pharmacological effects similar to the phenothiazines....
, an antipsychotic, is administered intramuscularly.
Psychotherapy
Other treatment methods may be used in psychiatric emergency service settings. Brief psychotherapyBrief therapy
Brief psychotherapy or Brief therapy is an umbrella term for a variety of approaches to psychotherapy. It differs from other schools of therapy in that it emphasises a focus on a specific problem and direct intervention...
can be used to treat acute conditions or immediate problems as long as the patient understands his or her issues are psychological, the patient trusts the physician, the physician can encourage hope for change, the patient has motivation to change, the physician is aware of the psychopathological history of the patient, and the patient understands that their confidentiality will be respected. The process of brief therapy under emergency psychiatric conditions includes the establishment of a primary complaint from the patient, realizing psychosocial factors, formulating an accurate representation of the problem, coming up with ways to solve the problem, and setting specific goals. The information gathering aspect of brief psychotherapy is therapeutic because it helps the patient place his or her problem in the proper perspective. If the physician determines that deeper psychotherapy sessions are required, he or she can transition the patient out of the emergency setting and into an appropriate clinic or center.
ECT
Electroconvulsive therapyElectroconvulsive therapy
Electroconvulsive therapy , formerly known as electroshock, is a psychiatric treatment in which seizures are electrically induced in anesthetized patients for therapeutic effect. Its mode of action is unknown...
is a controversial form of treatment which cannot be involuntarily applied in psychiatric emergency service settings. Instances wherein a patient is depressed to such a severe degree that the patient cannot be stopped from hurting himself or herself or when a patient refuses to swallow, eat or drink medication, electroconvulsive therapy could be suggested as a therapeutic alternative. While preliminary research suggests that electroconvulsive therapy may be an effective treatment for depression, it usually requires a course of six to twelve sessions of convulsions lasting at least 20 seconds for those antidepressant effects to occur.
Hospital admission
Involuntary commitment
Involuntary commitmentInvoluntary commitment
Involuntary commitment or civil commitment is a legal process through which an individual with symptoms of severe mental illness is court-ordered into treatment in a hospital or in the community ....
, or sectioning, refers to situations where police officer
Police officer
A police officer is a warranted employee of a police force...
s, health officers, or health professional
Health care provider
A health care provider is an individual or an institution that provides preventive, curative, promotional or rehabilitative health care services in a systematic way to individuals, families or communities....
s classify an individual as dangerous to themselves, others, gravely disabled, or mentally ill according to the applicable government law for the region. After an individual is transported to a psychiatric emergency service setting, a preliminary professional assessment is completed which may or may not result in involuntary treatment
Involuntary treatment
Involuntary treatment refers to medical treatment undertaken without a person's consent. In almost all circumstances, involuntary treatment refers to psychiatric treatment administered despite an individual's objections...
. Some patients may be discharged shortly after being brought to psychiatric emergency services while others will require longer observation and the need for continued involuntary commitment will exist. While some patients may initially come voluntarily, it may be realized that they pose a risk to themselves or others and involuntary commitment may be initiated at that point.
Referrals and voluntary hospitalization
Voluntary hospitalizations are outnumbered by involuntary commitments partly due to the fact insurance companies tend not to pay for hospitalization unless an imminent danger exists to the individual or community. In addition, psychiatric emergency service settings admit approximately one third of patients from assertive community treatmentAssertive Community Treatment
Assertive community treatment, or ACT, is an intensive and highly integrated approach for community mental health service delivery. ACT programs serve people whose symptoms of mental illness result in severe functional difficulties that interfere with their ability to achieve personally meaningful...
centers.
Controversies
Similar to other fields of medicine, malpractice in the treatment of brain illnesses can occur as psychiatrists an neurologists make mistakes. Patients have died under treatment in emergency situations. However, lawsuits in the medical psychiatric profession are much fewer than other medical complaints.See also
- Emergency medicineEmergency medicineEmergency medicine is a medical specialty in which physicians care for patients with acute illnesses or injuries which require immediate medical attention. While not usually providing long-term or continuing care, emergency medicine physicians diagnose a variety of illnesses and undertake acute...
- Mental health first aidMental health first aidMental health first aid has been defined as "the help provided to a person developing a mental health problem or in a mental health crisis. The first aid is given until appropriate professional treatment is received or until the crisis resolves"....
- PsychiatryPsychiatryPsychiatry is the medical specialty devoted to the study and treatment of mental disorders. These mental disorders include various affective, behavioural, cognitive and perceptual abnormalities...
- Psychiatric hospitalPsychiatric hospitalPsychiatric hospitals, also known as mental hospitals, are hospitals specializing in the treatment of serious mental disorders. Psychiatric hospitals vary widely in their size and grading. Some hospitals may specialise only in short-term or outpatient therapy for low-risk patients...
Further reading
- Nurius, P.S. (1983). Emergency psychiatric services: a study of changing utilization patterns and issues. International Journal of Psychiatry in Medicine, 13, 239–254.
- Otong-Antai, D. (2001). Psychiatric Emergencies. Eau Claire: PESI Healthcare.
- Sanchez, Federico, (2007), "Suicide Explained, A Neuropsychological Approach."
- Glick RL, Berlin JS, Fishkind AB, Zeller SL (2008) "Emergency Psychiatry: Principles and Practice." Baltimore: Lippincott Williams & Wilkins
External links
- American Association of Emergency Psychiatry
- ATSDR - Psychological Responses to Hazardous Substances U.S. Department of Health and Human Services (public domain)

