Sperm donation
Encyclopedia
Sperm donation is the provision (or ‘donation’) by a man, (known as a ‘sperm donor’), of his sperm
, with the intention that it be used to impregnate a woman who is not usually the man's sexual partner, in order to produce a child.
A sperm donor is the natural or biological father
of every child produced as a result of his donations.
Sperm donation can be performed either in a medical setting, such as a fertility clinic
, or at home. Home donations are done using sperm from a known donor, or from a contact through a classified advert or sperm donation forum
or website.
Pregnancies are usually achieved using donated sperm by artificial insemination
(either by ICI or IUI in a clinic, or Intravaginal Insemination at home) and less commonly by in vitro fertilization (IVF), usually known in this context as ART
but insemination may also be achieved by a donor having sexual intercourse
with a woman for the sole purpose of initiating conception. This method is known as natural insemination, or NI
.
The general process of sperm donation is described as third party reproduction
.
A donor may donate sperm as an anonymous or non-anonymous donor through a clinic known as a sperm bank
or through a third party or broker who makes arrangements between sperm donors and recipient women, known as a sperm agency. A sperm donor may also donate directly to the recipient and may be known to her as a friend or non-blood relative. This may be done privately, or through a sperm bank or fertility clinic
. In some cases, informal sperm donation is not recognised in law, and in many cases informal sperm donors are also the legal father, although the rights and responsibilities this status confers may be ignored by both the donor and recipient.
Sperm donation is used to assist heterosexual couples unable to produce children because of male infertility
, such as where the male partner produces no sperm (azoospermia
). However, techniques (e.g. Intracytoplasmic sperm injection
) have been developed which enable many 'male factor' problems to be overcome and which enable the couple to produce their own biological child (such techniques are not without risks). Sperm donation is now popularly used as a means to enable women who are single (sometimes known as choice mothers) or partnered lesbians to conceive children.
When a donor's sperm is successfully used repeatedly to fertilize the same or different women, potentially several or many siblings and half-siblings will be born. Private donors are not subject to legal limits on the number of offspring, unlike clinic donors. Limits on number of offspring vary widely between different jurisdictions, and there is a lack of academic rigor to the selection of these limits.
Laws vary between countries and states as regards the anonymity or otherwise of clinic donors. Although many donors choose to remain anonymous, new technologies such as the Internet and DNA testing have opened up new avenues for those wishing to know more about the biological father, siblings and half-siblings.
Sperm donors may be selected on the grounds of looks, personality, academic ability, race, and many other factors. Similarity in appearance to the recipient's partner is often a criterion. Clinics and jurisdictions vary widely in the amount of information provided on donors. A desire to obtain more information on donors is one reason why women may choose informal/private donations over clinic donations.
, private sperm donation is not properly recognised in law. Websites and advertising services for private sperm donation may also carry adverts for co-parenting arrangements. Donors may or may not be paid for the donation, according to local laws and agreed arrangements. Even in unpaid arrangements, expenses are often offered. In some countries sperm agencies exist that mediate sperm delivery directly from a donor to the recipient, although their legality varies according to jurisdiction, and may be unclear. Private donors (see types of donors) donate independently of banks or agencies, using classified ads, social networks and forums
to find recipients. Donors may operate either as anonymous or non-anonymous donors or "directed" donors, who direct their sperm to be used by a specific person. Non-anonymous donors are also called "known donors", "open donors" or "identity disclosure donors".
, the donor will usually donate sperm for a specified contractual period of time generally ranging from six to twenty-four months depending on the number of pregnancies which the sperm bank intends to produce from the donor. However, not all donors complete the intended programme of donations. If a sperm bank has access to world markets e.g. by direct sales, or sales to clinics outside their own jurisdiction, a man may donate for a longer period than two years, as the risk of consanguinity
is reduced (although local laws vary widely). The agreement or contract between the donor and the sperm bank will usually contain provisions about the place and hours for donation, a requirement to notify the sperm bank in the case of acquiring a sexual infection, and the requirement not to have intercourse or to masturbate for a period of usually 2-3 days before making a donation.
To donate sperm a man must generally meet specific requirements regarding age and medical history. In the United States, sperm banks are regulated as Human Cell and Tissue or Cell and Tissue Bank Product (HCT/Ps) establishments by the Food and Drug Administration
. Many states also have regulations in addition to those imposed by the FDA. In the European Union
a sperm bank must have a license according to the EU Tissue Directive
. In the UK sperm banks are regulated by the Human Fertilisation and Embryology Authority
.
in a private room or cabin, known as a 'men's production room' (UK), 'donor cabin' (DK) or a masturbatorium (USA). Many of these facilities contain pornography such as videos/DVD, magazines, and/or photographs which may assist the donor in becoming stimulated in order to facilitate production of the ejaculate, also known as the 'semen sample'. In some circumstances, it may also be possible for donors to ejaculate during sexual intercourse, and use a condom
to collect the sperm.
semen extender
is added if the sperm is to be placed in frozen storage in liquid nitrogen
, and the sample is then frozen in a number of vials or straws . One sample will be divided into 1-20 vials or straws depending on the quantity of the ejaculate and whether the sample is 'washed' or 'unwashed'. Following the necessary quarantine period, the samples will be thawed and used to impregnate women through artificial insemination
or other ART
treatments. 'Unwashed' samples are used for ICI
treatments, and 'washed' samples are used in IUI and IVF procedures.
In the US, the screening procedures are regulated by the FDA, the ASRM
, the American Association of Tissue Banks, and the CDC
. The screening regulations are more stringent today than they have been in the past.
In Europe, the screening procedure are regulated by the EU Tissue Directive
.
Screening includes:
Cystic fibrosis carrier screening, chromosome analyses, and hemoglobin evaluations are performed on the majority of sperm donor applicants in the United States. Donors of Jewish, Québécois, or Cajun descent may also get genetic testing for the carrier trait of Tay Sachs disease, but there is significant variation in screening for other disorders that occur with increased frequency in this population.
The samples are generally frozen and stored for at least 6 months after which the donor will be re-tested for the STI
s. This is to ensure no new infections have been acquired or have developed during the period of donation. Providing the result is negative, the sperm samples can be released from quarantine and used in treatments.
Washing techniques are developing that purify sperm from viral load of HIV and hepatitis C., but nevertheless clinics do not offer sperm from carriers of significant STIs.
Screening for cytomegalovirus
is not mandatory in all jurisdictions, and positive donors may still donate at sperm banks.
Donor screening for cytomegalovirus
(CMV) is carried out by testing for IgG antibodies against CMV that are produced if the donor ever has contracted CMV, which is the case in between 50% and 80% of adults. Such antibody-positive individuals may potentially shed virus that remain latent in the body in the semen, infecting the mother and, in turn, the embryo/fetus. Most babies will not be harmed by the virus, but a small percentage may develop neurological abnormalities. However, the risk of acquiring CMV infection from an antibody-positive sperm donor is believed to be extremely low, at least where sperm banks perform follow-up tests on antibody-positive donors for type IgM antibodies that indicate current or recent CMV infection, and where sperm preparations are performed that decrease the amount of white blood cells in the samples, e.g. in samples prepared for IUI. In uncertainty, recipient women may do a blood sample test on themselves for IgG antibodies at their health care provider, determining immunity against the virus.
in intrauterine insemination (IUI) or intra-cervical insemination (ICI), or, less commonly, it may be prepared for use in other assisted reproductive techniques such as IVF and ICSI
. Donated sperm may also be used in surrogacy
arrangements either by artificially inseminating the surrogate with donor sperm (known as traditional surrogacy) or by implanting in a surrogate embryos which have been created by using donor sperm together with eggs from a donor or from the 'commissioning woman' ( known as gestational surrogacy). Spare embryos from this process may be donated to other women or surrogates. Donor sperm may also be used for producing embryos with donated eggs which are then donated to a woman who is not genetically related to the child she produces.
In medical terms, using donor sperm to achieve a pregnancy in IVF or ICSI
is no different from using sperm from a woman's partner.
In the UK, most donors are anonymous at the point of donation and recipients can only see non-identifying information about their donor (height, weight, ethnicity etc.). Donors need to provide identifying information to the clinic and clinics will usually ask the donor's GP to confirm any medical details they have been given. Donors are asked to provide a pen portrait of themselves which is held by the HFEA and can be obtained by the adult conceived from the donation at the age of 18, along with identifying information such as the donor's name and last known address. Known donation is permitted and it is not uncommon for family or friends to donate to a recipient couple.
, and because of the rigorous screening procedures which they adopt, including a typical age limitation on sperm donors, often limiting sperm donors to the ages of 21-39 (see paternal age effect
), and genetic and health screening of donors. In addition, sperm banks may try to ensure that the sperm used in a particular recipient woman comes from a donor whose blood group and genetic profile is compatible with those of the woman.
which is rhesus negative, and where her partner is rhesus positive. The woman's body may reject a fetus if it has rhesus positive blood. Anti D
injections have been developed and may be used to attempt to avoid this, and these are usually automatically given to rhesus negative women immediately after they give birth to their first child. However, in the past this was either not possible or was not always routinely undertaken where a woman gave birth or had an abortion and she may have trouble carrying a child later in life. Furthermore, for some women, the anti D injection does not provide the entire solution, particularly where there is a medical history of complications during pregnancy which risk the woman's blood and that of the fetus becoming mixed. In such cases, sperm from a rhesus negative donor can provide the solution and a woman may be able to conceive and carry a pregnancy to full term when otherwise this would not be possible. For this reason, sperm from rhesus negative sperm donors is often in great demand, particularly those with the O negative blood group who are universal donors.
and a container for shipping the sperm. This is collected and delivered by courier and the woman uses the donor's sperm to perform her own artificial insemination
, typically without medical supervision. The whole process preserves the anonymity of the parties and it enables a donor to produce sperm in the privacy of his own home. A donor will generally produce samples once or twice during a recipient's fertile period, but a second sample each time may not have the same fecundity of the first sample because it is produced too soon after the first one. Pregnancy rates by this method of sperm donation may vary more than those achieved by sperm banks or fertility clinics. Transit times may vary and these have a significant effect on sperm viability so that if a donor is not located near to a recipient woman the sperm may deteriorate. However, the use of fresh, as opposed to frozen semen will mean that a sample has a greater fecundity and this can produce higher pregnancy rates.
Sperm agencies may impose limits on the number of pregnancies achieved from each donor but in practice this is more difficult to achieve than for sperm banks where the whole process may be more regulated. Most sperm donors only donate for a limited period however, and since sperm supplied by a sperm agency is not processed into a number of different vials, there is a practical limit on the number of pregnancies which are usually produced in this way. A sperm agency will, for the same reason, be less likely than a sperm bank to enable a woman to have subsequent children by the same donor.
Sperm agencies are largely unregulated and, because the sperm is not quarantined, it may carry sexually transmitted diseases. This lack of regulation has led to the competent authorities in some jurisdictions bringing legal action against sperm agencies in certain cases. Agencies typically insist on STI testing for donors, but such tests cannot detect recently-acquired infections. Donors providing sperm in this way may not be protected by laws which apply to donations through a sperm bank or fertility clinic and will, if traced, be regarded as the legal father of each child produced by their sperm, (but see below, Private donors).
and sperm donation below'). Where a private or directed donor is used, sperm need not be frozen. Such donors may already know the recipients, or if arranged through a broker, may meet the recipients and may therefore become known to the recipient. Some brokerage services facilitate contact that maintains semi-anonymous identities for legal reasons.
Private donations may be free of charge - avoiding the significant costs of a more medicalised insemination - and fresh rather than frozen semen is generally deemed to increase the chances of pregnancy. However, they also carry the higher risks associated with any unscreened sexual or body fluid contact. Legal treatment of donors varies across jurisdictions, and in most jurisdictions, e.g., Sweden, personal and directed donors lack legal safeguards that may be available to anonymous donors. However, the laws of some nations (e.g., New Zealand), recognize written agreements between donors and recipients in a similar way to institutional donations.
donors in EU may only receive compensation, which is strictly limited to making good the expenses and inconveniences related to the donation. A survey among sperm donors in Cryos International Sperm bank showed that altruistic as well as financial motives were the main factors for becoming a donor. However, when the compensation was increased 100% in 2004 (to DKK 500) it had no significant impact on neither the numbers of new donor candidates coming in nor the frequency of donations from the existing donors. When the compensation was reduced to the previous level (DKK 250) again one year later in 2005 there was no effect either. This led to the assumption that altruism is the main motive and that financial compensation is secondary.
Equipment to collect, freeze and store sperm is available to the public notably through certain US outlets, and some donors process and store their own sperm which they then sell via the Internet.
The selling price of processed and stored sperm is considerably more than the sums which are received by donors. Treatments with donor sperm are generally expensive and are seldom available free of charge through national health services. Sperm banks often package treatments into e.g. three cycles, and in cases of IVF or other ART treatments, they may reduce the charge if a patient donates any spare embryos which are produced through the treatment. There is often more demand for fertility treatment with donor sperm than there is donor sperm available, and this has the effect of keeping the cost of such treatments reasonably high.
However, the following equations generalize the main factors involved:
For intracervical insemination:
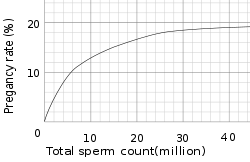
The pregnancy rate increases with increasing number of motile sperm used, but only up to a certain degree, when other factors become limiting instead.
With these numbers, one sample would on average help giving rise to 0.1-0.6 children, that is, it actually takes on average 2-5 samples to make a child.
For intrauterine insemination, a centrifugation fraction (fc) may be added to the equation:
On the other hand, only 5 million motile sperm may be needed per cycle with IUI (nr=5 million)
Thus, only 1-3 samples may be needed for a child if used for IUI.
Using ART
treatments such as IVF can result in one donor sample (or ejaculate) producing on average considerably more than one birth. However, the actual number of births per sample will depend on the actual ART
method used, the age and medical condition of the woman bearing the child, and the quality of the embryos produced by fertilization. Donor sperm is less commonly used for IVF treatments than for artificial insemination
. This is because IVF treatments are usually required only when there is a problem with the female conceiving, or where there is a 'male factor problem' involving the woman's partner. Donor sperm is also used for IVF in surrogacy arrangements where an embryo may be created in an IVF procedure using donor sperm and this is then implanted in a surrogate. In a case where IVF treatments are employed using donor sperm, surplus embryos may be donated to other women or couples and used in embryo transfer
procedures. When donor sperm is used for IVF treatments, there is a risk that large numbers of children will be born from a single donor, and many sperm banks therefore limit the amount of semen from each donor which is prepared for IVF use, or they may restrict the period of time for which such a donor donates his sperm to perhaps as little as three months (about nine or ten ejaculates).
A donor who makes a non-anonymous sperm donation is termed a known donor, open identity or identity release donor.
Non-anonymous sperm donors are, to a substantially higher degree, driven by altruistic motives for their donations.
In any case, some information about the donor may be released to the woman/couple at the time of treatment. A limited donor information at most includes height, weight, eye, skin and hair colour. In Sweden, this is all the information a receiver gets. In the US, on the other hand, additional information may be given, such as a comprehensive biography and sound/video samples.
For most sperm recipients, anonymity of the donor is not of major importance at the obtainment or tryer-stage,. The main reason for anonymity is that recipients think it would be easiest if the donor was completely out of the picture. However, some recipients regret not having chosen non-anonymous donor years later, for instance when the child desperately wants to know more about the donor anyway.
One in three donor conceived children want information about their biological father.
There is a risk of bias in the information given by clinics or sperm banks regarding anonymity, making anonymous sperm donation seem more favorable than it may actually be, resulting from that anonymous sperm donations are easier for them to handle in the long term, because anonymity does not put the clinic or sperm bank responsible for safely storing donor information for a long period of time. In addition, a majority of donors are anonymous, causing a relative deficit in non-anonymous sperm supply.
In the United States, the trend of wanting to know the identity of donors has resulted in some sperm banks offering exclusively non-anonymous donors.
(2009), granted visitation rights to a sperm donor and suggested that it would do so in future cases. Recent court cases have been eroding this protection, finding several private sperm-donors financially responsible for their offspring. The widely publicised case of Andy Bathie
highlights the developing area of fertility law. A major factor in the determination of the sperm donor's support obligation is whether the donor has participate in the child's life in a paternal capacity.
Several countries, e.g. Sweden, Norway, the Netherlands, Britain, Switzerland, Australia and New Zealand only allow non-anonymous sperm donation. The child may, when grown up (15–18 years old), get contact information from the sperm bank about his/her biological father. In Denmark, however, a sperm donor may choose to be either anonymous or non-anonymous. Nevertheless, the initial information which the receiving woman/couple will receive is the same.
Approximately 60% of requesters are female. Approximately 40% of requests are from people raised by single women, 30% from those raised by lesbian couples, and 20% from those raised by heterosexual couples. Approximately 60% of them are of the opinion that all sperm donations should include identity release.
The number of children permitted to be born from a single donor varies according to law and practice. These laws are designed to protect the children produced by sperm donation from consanguinity
in later life: they are not intended to protect the sperm donor himself and those donating sperm will be aware that their donations may give rise to numerous pregnancies in different jurisdictions. Such laws, where they exist, vary from state to state, and a sperm bank may also impose its own limits. The latter will be based on the reports of pregnancies which the sperm bank receives, although this relies upon the accuracy of the returns and the actual number of pregnancies may therefore be somewhat higher. Nevertheless, sperm banks frequently impose a lower limit on geographical numbers than some US states and may also limit the overall number of pregnancies which are permitted from a single donor. When calculating the numbers of children born from each donor, the number of siblings produced in any 'family' as a result of sperm donation from the same donor are almost always excluded. There is, of course, no limit to the number of offspring which may be produced from a single donor where he supplies his sperm privately.
Despite the laws limiting the number of offspring, some donors may produce substantial numbers of children, particularly where they donate through different clinics, where sperm is onsold or is exported to different jurisdictions, and where countries or states do not have a central register of donors.
Sperm agencies, in contrast to sperm banks, rarely impose or enforce limits on the numbers of children which may be produced by a particular donor partly because they are not empowered to demand a report of a pregnancy from recipients and they are rarely, if ever, able to guarantee that a woman may have a subsequent sibling by the donor who was the biological father of her first or earlier children.
to other countries to get the treatment.
For instance, when Sweden banned anonymous sperm donation in 1980, the number of active sperm donors dropped from approximately 200 to 30. Sweden now has an 18 month long waiting list for donor sperm. At least 250 Swedish sperm recipients travel to Denmark annually for insemination. Some of this is also due to the fact that Denmark also allows single women to be inseminated.
After the United Kingdom ended anonymous sperm donation in 2005, the numbers of sperm donors went up, reversing a three-year decline. However, there is still a shortage, and some doctors have suggested raising the limit of children per donor. Sperm exports from Britain are legal (subject to the EU Directive on Tissue Exports) and donors may remain anonymous in this context. Some UK clinics export sperm which may in turn be used in treatments for fertility tourists in other countries. UK clinics also import sperm from Scandinavia. In 2009 one Danish clinic secure the approval of the HFEA to import sperm via registered clinics for use in the UK. The sperm must have been processed, stored and quarantined in compliance with UK regulations. The donors have agreed to be identified when the children produced with their sperm reach the age of eighteen. The number of children produced from such donors in the UK will, of course, be subject to HFEA rules (i.e. currently a limit of ten families,) but the donors' sperm may be used worldwide in accordance with the clinic's own limit of one child per 200.000 of population, subject to national or local limits which apply.
Korea has a sperm shortage because their Bioethics Law prohibits selling and buying of sperm between clinics, and a donor may only help giving rise to a child to one single couple.
Canada also has a shortage because it has been made unlawful to pay people for donating it, requiring recipients who wish to purchase it to import it from the United States.
The United States, on the other hand, has had an increase in sperm donors during the late 2000s recession
, with donors finding the monetary compensation more favorable.
Sperm banks rarely impose limits on the numbers of second or subsequent siblings. Even where there are limits on the use of sperm by a particular donor to a defined number of families (as in the UK) the actual number of children produced from each donor will often be far greater.
A UK sperm bank however, may only onsell sperm before the national limit of ten families has been achieved from one donor within the UK. This means, for example, that a sperm bank may recruit a donor and prepare samples for ICI, IUI and ART use from his donations. After 9 months it is able to release the 10 or so samples donated within the first 3 months, from 6 month quarantine ( approximately 100 vials) and it uses these to achieve 6 pregnancies (although more pregnancies could, of course, be achieved from the number of vials prepared as illustrated). The sperm bank is then able to onsell sperm from that donor to sperm banks and clinics outside the UK and it can illustrate the fecundity of the various types of samples it sells from the pregnancy rates it has achieved. However, from April 2010, the HFEA has imposed limitations on exports of an individual's sperm. The donor must now agree to the export and to the use of his donations to a particular country, and he must be told that regulations for use in that country will vary. He must not have put a limit on the number of births which may be achieved from his donations. The HFEA must be notified of exports of sperm from the UK which will only be granted in accordance with 'special directions'. Individual clinics exporting sperm or onselling to other UK clinics are now responsible for ensuring that the maximum number of births produced from each donor is not exceeded. Prior to 2010 UK clinics could export any quantity of an individual's sperm samples without the consent of the HFEA provided that the donor had consented generally to export and had not imposed a limit on the number of children born from his sperm.
The regulations introduced in April 2010 are intended to ensure that no more than ten families are produced from each donor, regardless of where this occurs. Before this time, some men donated for periods in excess of two years (some for even four or five years) and vials of their sperm were exported without limitation provided that not more than ten families had been produced from their samples in the UK at the time of the export. Donors with particular blood groups or with sperm which produced higher than average pregnancy rates were sometimes offered the opportunity to donate for such prolonged periods. Although this gave rise to considerable numbers of offspring from such donors, local rules applied where the treatments were carried out and there was probably only a low risk of consanguinity. Donors who donated over such periods of time were also aware that their sperm would be used to create numerous offspring.
Embryos may also be onsold. These are usually spare embryos which are created through IVF treatment where a woman achieves the number of pregnancies she requires and the resulting embryos may therefore be disposed of. Donor sperm (and donor eggs) may be used in IVF treatments, and as many as eighteen eggs may be fertilized using one vial of donor sperm, although only the most viable of these will be subsequently implanted in a woman in an attempt to achieve a pregnancy. In the case of the UK, the consent of the donors of both the egg and the sperm which were used to create the embryo must be obtained, and the limit of ten families produced from each donor must not be exceeded.
Onselling is normally only appropriate where the donor remains anonymous. Sperm banks purchasing sperm samples may in turn onsell these to other sperm banks and often engage in the process of exchanging samples with other sperm banks. This is a common practice which enables sperm banks to offer a wider variety of donors, as well as to onsell samples from donors who have reached the maximum permitted number of offspring imposed by, or on, that clinic. Onselling may therefore give rise to numerous pregnancies being produced from individual donors which can sometimes total 100 or more (see above 'Limitation' and the associated link) particularly where a sperm donor donates his sperm for a period of two years or more and where his samples are prepared for IVF use. Sperm from certain donors, such as those with particular blood groups, physical features or intellect, may also be more in demand than sperm from other donors. However, in every case rules as to use and the limitation on the number of pregnancies which apply locally will reduce the risk of consanguinity. The lack of overall records as to use and success will mean that the numbers of pregnancies achieved from the samples of an individual donor will not exist and the donor will not be at risk of knowing the large number of births that were produced from the samples he donated.
Sperm may also be sold on for research or educational purposes, usually after the number of births from the donor concerned has reached its maximum. Sperm is used for genetic and fertility testing, and also for research into birth control.
in adulthood.
. Through the advent of DNA testing and Internet
access to extensive database
s of information, one sperm donor has recently been traced. In 2005 it was revealed in New Scientist magazine that an enterprising 15-year-old used information from a DNA test and the Internet to identify and contact his father, who was a sperm donor. This has brought into question the ability of sperm donors to stay anonymous.
, Canada
, Kenya
, and Hong Kong
. Several UK clinics also export donor sperm but they must take steps to ensure that the maximum number of ten families produced from each donor is not exceeded. The use of the sperm outside the UK will also be subject to local rules. Within the EU there are now regulations governing the transfer of human tissue including sperm between member states to ensure that these take place between registered sperm banks. However, the Food and Drug Administration
(FDA) of the US has banned import of any sperm, motivated by a risk of mad cow disease
, although such a risk is insignificant, since artificial insemination is very different from the route of transmission of mad cow disease. The prevalence of mad cow disease is one in a million, probably less for donors. If prevalence was the case, the infectious proteins would then have to cross the blood-testis barrier
to make transmission possible. Transmission of the disease by an insemination is approximately equal to the risk of getting killed by lightning.
is a charity which provides information, advice and support for people wishing to become egg, sperm or embryo donors. The Trust runs a national helpline and online discussion list for donors to talk to each other.
However, there are certain circumstances where the child very likely should be told:
and helps give the child a sense of identity by answering questions about the donor. It is more common among open identity-families headed by single women. Less than 1% of those seeking donor-siblings find it a negative experience, and in such cases it is mostly where the parents have disagreed with each other about how the relationship should proceed.
method as a solution to childlessness may view it as preserving the sexual integrity of their relationship. However, sperm donation does not maintain the reproductive integrity of a relationship in that the woman's sexual partner is not the biological father of her child, and it is the sperm donor, not the partner, who is the biological father.
However, others point out that the process is essentially a sexual one: a woman's innate sexuality may be the reason why a child is wanted, the donor has to be screened for sexually transmitted diseases which could be passed on through the use of his sperm, and the donor has to sexually stimulate himself in order to produce the sperm samples which are used for achieving pregnancies in women to whom he is not related. Some would argue that it is impossible to distinguish sexuality from reproduction, and that the very reason for preserving sexual integrity is to preserve reproductive integrity.
.
For many donors and recipient women, the lack of physical sexual contact between the parties is one of the essential advantages of sperm donation. Whether the donor is anonymous or not, and whether or not the parties meet, the fact that the reproductive process takes place without genital contact serves to place the procedure on a level which is not readily identified as 'sexual' within the generally understood meaning (see 'Sperm donation and sexuality' above).
However, the very fact that sperm donation involves the placing of a man's gamete in the reproductive tract of a woman for the sole reason of enabling the woman to have that man's child does mean that the process is an intensely personal one which involves the highest degree of intimate contact. In this context, personal, physical intimacy may be seen as secondary to the reproductive process which is taking place. A 'natural' conception also avoids the need to be subjected to mechanical procedures which may or may not involve the intervention of third parties.
NI almost invariably produces higher pregnancy rates than ICI, which is the usual method of artificial insemination deployed in private donor arrangements. This is because NI
involves the fresh and immediate deposit of the donor's sperm high up in a woman's vagina near to the entrance to the womb. By comparison, semen used for artificial insemination
must normally be allowed to liquefy to enable it be used in a syringe (unless a conception cap or conception device
using fresh semen is used for the artificial insemination), and fertility clinics and sperm banks always use sperm which has been liquefied, frozen and thawed, all of which reduces its fecundity. Ensuring that the sperm is deposited correctly in the vagina requires a certain knowledge or skill and the failure correctly to perform artificial insemination is thought to lead to many failures to conceive. Furthermore, medical evidence shows that semen quality
is likely to be substantially higher and its fertility therefore greater where semen is produced during sexual intercourse rather than by masturbation.
The availability of screening and home testing for sexually transmitted diseases, ovulation timings and male and female fertility also make the procedure safer and more reliable than was previously possible.
Consequently, an increasing number of private sperm donors now offer NI
as an alternative to the use of artificial means, or they will do so after attempts to achieve a conception by artificial insemination have failed, and similarly, an increasing number of women are seeking a natural conception from a donor. Some fertility clinics, notably in India and China also offer donors and surrogate women who will attempt to achieve pregnancies by NI as a more effective and cheaper alternative to ART methods. Where NI
is used to achieve a pregnancy by a donor, the ethical considerations are significantly different from considerations where a pregnancy is achieved by artificial means. Whatever method is used, sperm donation is, of course, essentially the attempt to impregnate a woman with the sperm of a man who is not her partner, and neither AI nor NI preserves the reproductive integrity of the relationship a woman has with her partner.
The growth of sperm banks and fertility clinics, the use of sperm agencies and the availability of anonymous donor sperm have assisted in making the use of sperm donation a more respectable, and therefore a more socially acceptable, procedure. The intervention of doctors and others may be seen as making the whole process merely another medical one, where inseminations may be referred to as 'treatments' and donor children as 'resulting from the use of' a donor's sperm, rather than as the biological children of a donor. Still, a study has indicated that both men and women view the use of donor sperm with more skepticism compared with the use of donor eggs, suggesting a unique underlying perception regarding the use of male donor gametes.
As acceptance of sperm donation has generally increased, so has the level of questioning as to whether 'artificial' means of conception are necessary, and some donor children too, have been critical of the procedures which were taken to bring them into the world. Against this background has been the increase in the use of NI
as a method of sperm donation. However, while some donors may be willing to offer this as a method of impregnation, it has many critics and it also raises further legal and social challenges.
Some donor children grow up wishing to find out who their fathers were, but others may be wary of embarking on such a search since they fear they may find scores of half-siblings who have been produced from the same sperm donor. Even though local laws or rules may restrict the numbers of offspring from a single donor, there are no worldwide limitations or controls and most sperm banks will onsell and export all their remaining stocks of vials of sperm when local maxima have been attained (see 'onselling' above).
One item of research has suggested that donor children have a greater likelihood of substance abuse
, mental illness
and criminal behavior when grown.http://www.slate.com/id/2256212 However, its motivation and credibility have been questioned.http://www.bionews.org.uk/page_65970.asp
In 1884 Professor William Pancoast at Philadelphia's Jefferson Medical College performed an insemination on the wife of a sterile Quaker merchant. Instead of taking the sperm from the husband, the professor chloroformed the woman, then let his medical students vote which one of among them was "best looking", with that elected one providing the sperm for the insemination. After talking to the husband, they decided it was best not to let the woman know. At the husband's request, his wife was never told how she became pregnant. As a result of this medical school experiment, the merchant's wife gave birth to a son, who became the first known child by donor insemination (DI).
For over a decade nothing more was heard on the subject. Then, in 1909, a letter by Addison Davis Hard appeared in the American journal Medical World, highlighting the procedure which had taken place at the Jefferson Medical College in Philadelphia in 1884—twenty-five years earlier.
From that time, a very few doctors performed donor insemination privately and such procedures were regarded as private by the parties. Records were usually not maintained so that donors could not be identified for paternity proceedings. Only fresh sperm could be used and it is thought that this largely came from the doctors and their own male staff, although a few private donors were sometimes used who were able to donate on a regular basis at short notice as required.
The first successful human pregnancy using frozen sperm was in 1953.
DI remained virtually unknown to the public until 1954. In that year the first comprehensive account of the process was published in The British Medical Journal.
Donor insemination provoked heated public debate. The Archbishop of Canterbury established the first in a long procession of commissions that, over the years, inquired into the development of the practice. It was at first condemned by the Lambeth Conference and recommended that it be made a criminal offence. A Parliamentary Commission agreed. In Italy, the Pope declared DI a sin, and proposed that anyone using the procedure be sent to prison.
In the same year, 1954, the Supreme Court of Cook County in the USA ruled that regardless of a husband's consent, DI was "contrary to public policy and good morals, and considered adultery on the mother's part." The sperm donor was not married to the child's mother, and therefore, regardless of her husband's consent, the woman's insemination constituted adultery. The ruling went on to say that, "A child so conceived, was born out of wedlock and therefore illegitimate. As such, it is the child of the mother, and the father has no rights or interest in said child." adultery.
However, the following year, Georgia became the first state to pass a statute legitimizing children conceived by DI, on the condition that both the husband and wife consented in advance in writing to the procedure.
In 1973 the Commissioners on Uniform State Laws, and a year later, the American Bar Association, approved the Uniform Parentage Act. This act provides that if a wife is artificially inseminated with donor semen under a physician's supervision, and with her husband's consent, the husband is treated for legal purposes as if he were the natural father of the DI child. This law has been followed by similar legislation in most states of the US.
In 1975, the first commercial sperm bank, Xytex Corporation, was opened in Augusta, GA by Dr. Armand Karow Jr. and Dr. John Black.
In the UK, the Warnock Committee looked at the whole issue of the donation of gametes and assisted reproduction techniques. Donor insemination was already available in the UK through unregulated clinics such as BPAS. The Committee's Report led to the passing of the Human Fertilisation and Embryology Act in 1990. This provided for a system of licensing for fertility clinics and procedures. It also provided that, where a man donates sperm at a licensed clinic in the UK and his sperm is used at a UK clinic to impregnate a woman, the man is not legally responsible for the resulting child.
The 1990 Act also established a central UK central register of donors and donor births to be maintained by the Human Fertilisation and Embryology Authority (the 'HFEA'), a supervisory body established by the Act. Following the Act, where any woman has a child by a man who donates his sperm through a licensed clinic as the result of the use of that man's sperm through artificial insemination or IVF at a licensed UK clinic, details of the child and of the donor, who is its biological father, are required to recorded on the register. This measure was intended to reduce the risk of consanguinity as well as to enforce the limit on the number of births permitted by each donor. The natural child of any donor has access to non-identifying information about him from the child's eighteenth birthday.
The emphasis in the 1990 Act in the UK was on protecting the unborn child. However, a general shortage of donor sperm at the end of the 20th century, exacerbated by the announcement of the removal of anonymity in the UK, led to concerns about the excessive use of the sperm of some donors. These concerns centered on the export and exchange of donor sperm with overseas clinics, and also the interpretation of the term 'sibling use' to include donated embryos produced from one sperm donor, and successive births by surrogates using eggs from different women but sperm from the same sperm donor. Donors were informed that up to ten births could be produced from their sperm, but few probably appreciated that the words 'other than in exceptional circumstances' in the consent could lead to so many pregnancies. These concerns led to the SEED Report commissioned by the HFEA which was in turn followed by new legislation and rules which finally recognised the interests of donors. Where a man donates his sperm through a UK clinic, that sperm is not now permitted to give rise to more than ten families wherever it is used.
In many western countries, sperm donation is now a largely accepted procedure. In the US and elsewhere, the growth in the number of sperm banks has been considerable and there has been a general commercialisation of the procedure. Recent years have also seen the trend away from sperm donation as a method of allowing heterosexual couples to produce children, as other fertility treatments have become more sophisticated, and towards the use of donated sperm by single women and single and coupled lesbians of the procedure. A sperm bank
in the US pioneered the use of on-line search catalogues for donor sperm, and these facilities are now widely available on the websites of sperm banks and fertility clinics.
Controls have been applied in a number of countries such as the UK to prohibit anonymous sperm donation. The Internet has provided a way for people to find donors through sperm donation websites and fertility forums. Recent years have also seen a growth in the number of donors willing to impregnate by NI
as social attitudes to sperm donation generally have changed and more and more women are questioning the need for artificial procedures. Controls over the number of families which are allowed to be created from each donor in many countries have led to the growth of fertility tourism
and to the increase in onselling and export by some sperm banks.
, Road Trip, The Back-Up Plan
, The Kids Are Alright (film)
, The Switch (film), and Baby Mama
, the latter also involving surrogacy
.
Films and other fiction depicting emotional struggles of assisted reproductive technology
have had an upswing first in the latter part of the 2000s decade, although the techniques have been available for decades. Yet, the amount of people that can relate to it by personal experience in one way or another is ever growing, and the variety of trials and struggles is huge.
Not valid.
Sperm
The term sperm is derived from the Greek word sperma and refers to the male reproductive cells. In the types of sexual reproduction known as anisogamy and oogamy, there is a marked difference in the size of the gametes with the smaller one being termed the "male" or sperm cell...
, with the intention that it be used to impregnate a woman who is not usually the man's sexual partner, in order to produce a child.
A sperm donor is the natural or biological father
Father
A father, Pop, Dad, or Papa, is defined as a male parent of any type of offspring. The adjective "paternal" refers to father, parallel to "maternal" for mother...
of every child produced as a result of his donations.
Sperm donation can be performed either in a medical setting, such as a fertility clinic
Fertility clinic
Fertility clinics are staffed medical clinics that assist couples, and sometimes individuals, who want to become parents but for medical reasons have been unable to achieve this goal via the natural course...
, or at home. Home donations are done using sperm from a known donor, or from a contact through a classified advert or sperm donation forum
Internet forum
An Internet forum, or message board, is an online discussion site where people can hold conversations in the form of posted messages. They differ from chat rooms in that messages are at least temporarily archived...
or website.
Pregnancies are usually achieved using donated sperm by artificial insemination
Artificial insemination
Artificial insemination, or AI, is the process by which sperm is placed into the reproductive tract of a female for the purpose of impregnating the female by using means other than sexual intercourse or natural insemination...
(either by ICI or IUI in a clinic, or Intravaginal Insemination at home) and less commonly by in vitro fertilization (IVF), usually known in this context as ART
ART
ART is a three-letter acronym that can mean:Medicine* The use of Antiretroviral drugs, in anti-retroviral therapy, for the treatment of HIV* Assisted reproductive technology* Androgen Replacement Therapy...
but insemination may also be achieved by a donor having sexual intercourse
Sexual intercourse
Sexual intercourse, also known as copulation or coitus, commonly refers to the act in which a male's penis enters a female's vagina for the purposes of sexual pleasure or reproduction. The entities may be of opposite sexes, or they may be hermaphroditic, as is the case with snails...
with a woman for the sole purpose of initiating conception. This method is known as natural insemination, or NI
NI
NI is a two-letter abbreviation and may refer to:-Business:* National Instruments, a U.S. producer of automated test equipment and virtual instrumentation software...
.
The general process of sperm donation is described as third party reproduction
Third party reproduction
Third party reproduction refers to a process where another person provides sperm or eggs or where another woman provides her uterus so that a woman can have a child. Thus the reproductive process goes beyond the traditional father-mother model. However, the third party's involvement is limited to...
.
A donor may donate sperm as an anonymous or non-anonymous donor through a clinic known as a sperm bank
Sperm bank
A sperm bank, semen bank or cryobank is a facility that collects and stores human sperm mainly from sperm donors, primarily for the purpose of achieving pregnancies through third party reproduction, notably by artificial insemination...
or through a third party or broker who makes arrangements between sperm donors and recipient women, known as a sperm agency. A sperm donor may also donate directly to the recipient and may be known to her as a friend or non-blood relative. This may be done privately, or through a sperm bank or fertility clinic
Fertility clinic
Fertility clinics are staffed medical clinics that assist couples, and sometimes individuals, who want to become parents but for medical reasons have been unable to achieve this goal via the natural course...
. In some cases, informal sperm donation is not recognised in law, and in many cases informal sperm donors are also the legal father, although the rights and responsibilities this status confers may be ignored by both the donor and recipient.
Sperm donation is used to assist heterosexual couples unable to produce children because of male infertility
Male infertility
Male infertility refers to the inability of a male to achieve a pregnancy in a fertile female. In humans it accounts for 40-50% of infertility. Male infertility is commonly due to deficiencies in the semen, and semen quality is used as a surrogate measure of male fecundity.-Pre-testicular...
, such as where the male partner produces no sperm (azoospermia
Azoospermia
Azoospermia is the medical condition of a male not having any measurable level of sperm in his semen. It is associated with very low levels of fertility or even sterility, but many forms are amenable to medical treatment...
). However, techniques (e.g. Intracytoplasmic sperm injection
Intracytoplasmic sperm injection
Intracytoplasmic sperm injection is an in vitro fertilization procedure in which a single sperm is injected directly into an egg.-Indications:...
) have been developed which enable many 'male factor' problems to be overcome and which enable the couple to produce their own biological child (such techniques are not without risks). Sperm donation is now popularly used as a means to enable women who are single (sometimes known as choice mothers) or partnered lesbians to conceive children.
When a donor's sperm is successfully used repeatedly to fertilize the same or different women, potentially several or many siblings and half-siblings will be born. Private donors are not subject to legal limits on the number of offspring, unlike clinic donors. Limits on number of offspring vary widely between different jurisdictions, and there is a lack of academic rigor to the selection of these limits.
Laws vary between countries and states as regards the anonymity or otherwise of clinic donors. Although many donors choose to remain anonymous, new technologies such as the Internet and DNA testing have opened up new avenues for those wishing to know more about the biological father, siblings and half-siblings.
Sperm donors may be selected on the grounds of looks, personality, academic ability, race, and many other factors. Similarity in appearance to the recipient's partner is often a criterion. Clinics and jurisdictions vary widely in the amount of information provided on donors. A desire to obtain more information on donors is one reason why women may choose informal/private donations over clinic donations.
Provision
A man who provides sperm as a sperm donor generally gives up all legal and other rights over the biological children produced from his sperm. However, in private arrangements, some degree of co-parenting may be agreed, and there may also be limits on the extent to which private donors can vary their rights and obligations, as in some jurisdictions such as the United KingdomUnited Kingdom
The United Kingdom of Great Britain and Northern IrelandIn the United Kingdom and Dependencies, other languages have been officially recognised as legitimate autochthonous languages under the European Charter for Regional or Minority Languages...
, private sperm donation is not properly recognised in law. Websites and advertising services for private sperm donation may also carry adverts for co-parenting arrangements. Donors may or may not be paid for the donation, according to local laws and agreed arrangements. Even in unpaid arrangements, expenses are often offered. In some countries sperm agencies exist that mediate sperm delivery directly from a donor to the recipient, although their legality varies according to jurisdiction, and may be unclear. Private donors (see types of donors) donate independently of banks or agencies, using classified ads, social networks and forums
Internet forum
An Internet forum, or message board, is an online discussion site where people can hold conversations in the form of posted messages. They differ from chat rooms in that messages are at least temporarily archived...
to find recipients. Donors may operate either as anonymous or non-anonymous donors or "directed" donors, who direct their sperm to be used by a specific person. Non-anonymous donors are also called "known donors", "open donors" or "identity disclosure donors".
Sperm banks
In a sperm bankSperm bank
A sperm bank, semen bank or cryobank is a facility that collects and stores human sperm mainly from sperm donors, primarily for the purpose of achieving pregnancies through third party reproduction, notably by artificial insemination...
, the donor will usually donate sperm for a specified contractual period of time generally ranging from six to twenty-four months depending on the number of pregnancies which the sperm bank intends to produce from the donor. However, not all donors complete the intended programme of donations. If a sperm bank has access to world markets e.g. by direct sales, or sales to clinics outside their own jurisdiction, a man may donate for a longer period than two years, as the risk of consanguinity
Consanguinity
Consanguinity refers to the property of being from the same kinship as another person. In that respect, consanguinity is the quality of being descended from the same ancestor as another person...
is reduced (although local laws vary widely). The agreement or contract between the donor and the sperm bank will usually contain provisions about the place and hours for donation, a requirement to notify the sperm bank in the case of acquiring a sexual infection, and the requirement not to have intercourse or to masturbate for a period of usually 2-3 days before making a donation.
To donate sperm a man must generally meet specific requirements regarding age and medical history. In the United States, sperm banks are regulated as Human Cell and Tissue or Cell and Tissue Bank Product (HCT/Ps) establishments by the Food and Drug Administration
Food and Drug Administration
The Food and Drug Administration is an agency of the United States Department of Health and Human Services, one of the United States federal executive departments...
. Many states also have regulations in addition to those imposed by the FDA. In the European Union
European Union
The European Union is an economic and political union of 27 independent member states which are located primarily in Europe. The EU traces its origins from the European Coal and Steel Community and the European Economic Community , formed by six countries in 1958...
a sperm bank must have a license according to the EU Tissue Directive
EU Tissue Directive
The EU Tissue Directive sets standards of quality and safety for the donation, procurement, testing, processing, preservation, storage and distribution of human tissues and cells intended for human application. It was adopted by the European Parliament on 7 April 2004 and came into effect between...
. In the UK sperm banks are regulated by the Human Fertilisation and Embryology Authority
Human Fertilisation and Embryology Authority
The Human Fertilisation and Embryology Authority is a statutory body in the United Kingdom that regulates and inspects all UK clinics providing in vitro fertilisation, artificial insemination and the storage of human eggs, sperm or embryos. It also regulates Human Embryo research...
.
Production
A man donates sperm at a clinic or sperm bank by way of masturbationMasturbation
Masturbation refers to sexual stimulation of a person's own genitals, usually to the point of orgasm. The stimulation can be performed manually, by use of objects or tools, or by some combination of these methods. Masturbation is a common form of autoeroticism...
in a private room or cabin, known as a 'men's production room' (UK), 'donor cabin' (DK) or a masturbatorium (USA). Many of these facilities contain pornography such as videos/DVD, magazines, and/or photographs which may assist the donor in becoming stimulated in order to facilitate production of the ejaculate, also known as the 'semen sample'. In some circumstances, it may also be possible for donors to ejaculate during sexual intercourse, and use a condom
Condom
A condom is a barrier device most commonly used during sexual intercourse to reduce the probability of pregnancy and spreading sexually transmitted diseases . It is put on a man's erect penis and physically blocks ejaculated semen from entering the body of a sexual partner...
to collect the sperm.
Preparation
The sample is then processed which may include 'washing' the sample so that sperm may be extracted from the rest of the material in the semen. A cryoprotectantCryoprotectant
A cryoprotectant is a substance that is used to protect biological tissue from freezing damage . Arctic and Antarctic insects, fish, amphibians and reptiles create cryoprotectants in their bodies to minimize freezing damage during cold winter periods. Insects most often use sugars or polyols as...
semen extender
Semen extender
Semen extender is a liquid diluent which is added to semen to preserve its fertilizing ability. The extender allows the semen to be freighted to the female, rather than requiring the male and female to be near to each other...
is added if the sperm is to be placed in frozen storage in liquid nitrogen
Liquid nitrogen
Liquid nitrogen is nitrogen in a liquid state at a very low temperature. It is produced industrially by fractional distillation of liquid air. Liquid nitrogen is a colourless clear liquid with density of 0.807 g/mL at its boiling point and a dielectric constant of 1.4...
, and the sample is then frozen in a number of vials or straws . One sample will be divided into 1-20 vials or straws depending on the quantity of the ejaculate and whether the sample is 'washed' or 'unwashed'. Following the necessary quarantine period, the samples will be thawed and used to impregnate women through artificial insemination
Artificial insemination
Artificial insemination, or AI, is the process by which sperm is placed into the reproductive tract of a female for the purpose of impregnating the female by using means other than sexual intercourse or natural insemination...
or other ART
Assisted reproductive technology
Assisted reproductive technology is a general term referring to methods used to achieve pregnancy by artificial or partially artificial means. It is reproductive technology used primarily in infertility treatments. Some forms of ART are also used in fertile couples for genetic reasons...
treatments. 'Unwashed' samples are used for ICI
ICI
ICI or Ici may mean:* ICI programming language, a computer programming language developed in 1992* Ici , an alternative weekly newspaper in Montreal, CanadaICI is also an abbreviation which may mean:...
treatments, and 'washed' samples are used in IUI and IVF procedures.
Medical screening
Sperm banks typically screen every potential donor for genetic diseases, chromosomal abnormalities and sexually transmitted infections that may be transmitted through sperm.In the US, the screening procedures are regulated by the FDA, the ASRM
American Society of Reproductive Medicine
The American Society for Reproductive Medicine is an organization that wants to advance the "art, science, and practice of reproductive medicine". It provides a forum for lay public, researchers, physicians and affiliated health workers through education, publications, and meetings...
, the American Association of Tissue Banks, and the CDC
Centers for Disease Control and Prevention
The Centers for Disease Control and Prevention are a United States federal agency under the Department of Health and Human Services headquartered in Druid Hills, unincorporated DeKalb County, Georgia, in Greater Atlanta...
. The screening regulations are more stringent today than they have been in the past.
In Europe, the screening procedure are regulated by the EU Tissue Directive
EU Tissue Directive
The EU Tissue Directive sets standards of quality and safety for the donation, procurement, testing, processing, preservation, storage and distribution of human tissues and cells intended for human application. It was adopted by the European Parliament on 7 April 2004 and came into effect between...
.
Screening includes:
- Taking a medical history of the donor, his children, siblings, parents, and grandparents etc. for three to four generations back. This is often done in conjunction with the patient's family doctor.
- HIV risk assessment interview, asking about sexual activity and any past drug use.
- Blood tests and urine tests for infectious diseases, such as:
- HIV-1/2 see sections below
- HTLV-1/2
- Hepatitis B
- Hepatitis CHepatitis CHepatitis C is an infectious disease primarily affecting the liver, caused by the hepatitis C virus . The infection is often asymptomatic, but chronic infection can lead to scarring of the liver and ultimately to cirrhosis, which is generally apparent after many years...
- SyphilisSyphilisSyphilis is a sexually transmitted infection caused by the spirochete bacterium Treponema pallidum subspecies pallidum. The primary route of transmission is through sexual contact; however, it may also be transmitted from mother to fetus during pregnancy or at birth, resulting in congenital syphilis...
- GonorrheaGonorrheaGonorrhea is a common sexually transmitted infection caused by the bacterium Neisseria gonorrhoeae. The usual symptoms in men are burning with urination and penile discharge. Women, on the other hand, are asymptomatic half the time or have vaginal discharge and pelvic pain...
- Chlamydia
- CytomegalovirusCytomegalovirusCytomegalovirus is a viral genus of the viral group known as Herpesviridae or herpesviruses. It is typically abbreviated as CMV: The species that infects humans is commonly known as human CMV or human herpesvirus-5 , and is the most studied of all cytomegaloviruses...
(CMV) see sections below, although not all clinics test for this.
- Blood and urine tests for blood typing and general health indicators: ABO/Rh typing, CBCComplete blood countA complete blood count , also known as full blood count or full blood exam or blood panel, is a test panel requested by a doctor or other medical professional that gives information about the cells in a patient's blood...
, liver panel and urinalysisUrinalysisA urinalysis , also known as Routine and Microscopy , is an array of tests performed on urine, and one of the most common methods of medical diagnosis... - Complete physical examination including careful examination of the penis, scrotum and testicles.
- Genetic testing for carrier traits, for example:
- Cystic FibrosisCystic fibrosisCystic fibrosis is a recessive genetic disease affecting most critically the lungs, and also the pancreas, liver, and intestine...
- Sickle-cell diseaseSickle-cell diseaseSickle-cell disease , or sickle-cell anaemia or drepanocytosis, is an autosomal recessive genetic blood disorder with overdominance, characterized by red blood cells that assume an abnormal, rigid, sickle shape. Sickling decreases the cells' flexibility and results in a risk of various...
- ThalassemiaThalassemiaThalassemia is an inherited autosomal recessive blood disease that originated in the Mediterranean region. In thalassemia the genetic defect, which could be either mutation or deletion, results in reduced rate of synthesis or no synthesis of one of the globin chains that make up hemoglobin...
- Other hemoglobin-related blood disorders.
- Cystic Fibrosis
Cystic fibrosis carrier screening, chromosome analyses, and hemoglobin evaluations are performed on the majority of sperm donor applicants in the United States. Donors of Jewish, Québécois, or Cajun descent may also get genetic testing for the carrier trait of Tay Sachs disease, but there is significant variation in screening for other disorders that occur with increased frequency in this population.
- General health
- Semen analysisSemen analysisA semen analysis evaluates certain characteristics of a male's semen and the sperm contained in the semen. It may be done while investigating a couple's infertility or after a vasectomy to verify that the procedure was successful. It is also used for testing donors for sperm donation, in stud...
for:- Sperm count
- MorphologyMorphology (biology)In biology, morphology is a branch of bioscience dealing with the study of the form and structure of organisms and their specific structural features....
- MotilityMotilityMotility is a biological term which refers to the ability to move spontaneously and actively, consuming energy in the process. Most animals are motile but the term applies to single-celled and simple multicellular organisms, as well as to some mechanisms of fluid flow in multicellular organs, in...
- AcrosomeAcrosomeThe acrosome is an organelle that develops over the anterior half of the head in the spermatozoa of many animals. It is a cap-like structure derived from the Golgi apparatus. Acrosome formation is completed during testicular maturation. In Eutherian mammals the acrosome contains digestive enzymes...
activity may also be tested
Quarantine
The samples are generally frozen and stored for at least 6 months after which the donor will be re-tested for the STI
STI
-Institutes:*Sega Technical Institute*Semantic Technology Institute International, a scientific and research network; also some of its members call themselves STI*Southern Technical Institute—a university in Marietta, Georgia, USA...
s. This is to ensure no new infections have been acquired or have developed during the period of donation. Providing the result is negative, the sperm samples can be released from quarantine and used in treatments.
Washing techniques are developing that purify sperm from viral load of HIV and hepatitis C., but nevertheless clinics do not offer sperm from carriers of significant STIs.
Cytomegalovirus
Screening for cytomegalovirus
Cytomegalovirus
Cytomegalovirus is a viral genus of the viral group known as Herpesviridae or herpesviruses. It is typically abbreviated as CMV: The species that infects humans is commonly known as human CMV or human herpesvirus-5 , and is the most studied of all cytomegaloviruses...
is not mandatory in all jurisdictions, and positive donors may still donate at sperm banks.
Donor screening for cytomegalovirus
Cytomegalovirus
Cytomegalovirus is a viral genus of the viral group known as Herpesviridae or herpesviruses. It is typically abbreviated as CMV: The species that infects humans is commonly known as human CMV or human herpesvirus-5 , and is the most studied of all cytomegaloviruses...
(CMV) is carried out by testing for IgG antibodies against CMV that are produced if the donor ever has contracted CMV, which is the case in between 50% and 80% of adults. Such antibody-positive individuals may potentially shed virus that remain latent in the body in the semen, infecting the mother and, in turn, the embryo/fetus. Most babies will not be harmed by the virus, but a small percentage may develop neurological abnormalities. However, the risk of acquiring CMV infection from an antibody-positive sperm donor is believed to be extremely low, at least where sperm banks perform follow-up tests on antibody-positive donors for type IgM antibodies that indicate current or recent CMV infection, and where sperm preparations are performed that decrease the amount of white blood cells in the samples, e.g. in samples prepared for IUI. In uncertainty, recipient women may do a blood sample test on themselves for IgG antibodies at their health care provider, determining immunity against the virus.
Preparations
Donated sperm may be prepared for use by artificial inseminationArtificial insemination
Artificial insemination, or AI, is the process by which sperm is placed into the reproductive tract of a female for the purpose of impregnating the female by using means other than sexual intercourse or natural insemination...
in intrauterine insemination (IUI) or intra-cervical insemination (ICI), or, less commonly, it may be prepared for use in other assisted reproductive techniques such as IVF and ICSI
ICSI
The abbreviation ICSI may refer to:* Intracytoplasmic sperm injection, a medical technique used in assisted reproduction* International Computer Science Institute, a non-profit research lab in Berkeley, California...
. Donated sperm may also be used in surrogacy
Surrogacy
Surrogacy is an arrangement in which a woman carries and delivers a child for another couple or person. This woman may be the child's genetic mother , or she may carry the pregnancy to delivery after having an embryo, to which she has no genetic relationship whatsoever, transferred to her uterus...
arrangements either by artificially inseminating the surrogate with donor sperm (known as traditional surrogacy) or by implanting in a surrogate embryos which have been created by using donor sperm together with eggs from a donor or from the 'commissioning woman' ( known as gestational surrogacy). Spare embryos from this process may be donated to other women or surrogates. Donor sperm may also be used for producing embryos with donated eggs which are then donated to a woman who is not genetically related to the child she produces.
In medical terms, using donor sperm to achieve a pregnancy in IVF or ICSI
ICSI
The abbreviation ICSI may refer to:* Intracytoplasmic sperm injection, a medical technique used in assisted reproduction* International Computer Science Institute, a non-profit research lab in Berkeley, California...
is no different from using sperm from a woman's partner.
Information about donor
In the US, sperm banks maintain lists or catalogues of donors which provide basic information about the donor such as racial origin, skin color, height, weight, colour of eyes, and blood group. Some of these catalogues are available for browsing via the Internet, while others are only made available to patients when they apply to a sperm bank for treatment. Some sperm banks make additional information about each donor available for an additional fee, and others make additional basic information known to children produced from donors when those children reach the age of eighteen. Some clinics offer "exclusive donors" whose sperm is only used to produce pregnancies for one recipient woman. How accurate this is, or can be, is not known, and neither is it known whether the information produced by sperm banks, or by the donors themselves, is true. Many sperm banks will, however, carry out whatever checks they can to verify the information they request, such as checking the identity of the donor and contacting his own doctor to verify medical details. Simply because such information is not verifiable does not imply that it is in any way inaccurate, and a sperm bank will rely upon its reputation which, in turn, will be based upon its success rate and upon the accuracy of the information about its donors which it makes available.In the UK, most donors are anonymous at the point of donation and recipients can only see non-identifying information about their donor (height, weight, ethnicity etc.). Donors need to provide identifying information to the clinic and clinics will usually ask the donor's GP to confirm any medical details they have been given. Donors are asked to provide a pen portrait of themselves which is held by the HFEA and can be obtained by the adult conceived from the donation at the age of 18, along with identifying information such as the donor's name and last known address. Known donation is permitted and it is not uncommon for family or friends to donate to a recipient couple.
Other screening criteria
Sexually active gay men are prohibited or discouraged from donating in some countries, including the United States. Some sperm banks also screen out some potential donors based on height, baldness, and family medical history.Sperm donation and reduced birth defects
Children conceived through sperm donation have a birth defect rate of almost a fifth compared with the general population. This may be explained by the fact that sperm banks only accept donors who have good semen qualitySemen quality
Semen quality is a measure of the ability of semen to accomplish fertilization. Thus, it is a measure of fertility in a man. It is the sperm in the semen that are of importance, and therefore semen quality involves both sperm quantity and quality...
, and because of the rigorous screening procedures which they adopt, including a typical age limitation on sperm donors, often limiting sperm donors to the ages of 21-39 (see paternal age effect
Paternal age effect
The paternal age effect can refer to the statistical relationships of: a man's age to sperm and semen abnormalities; a man's age to his fertility; a man's age to adverse pregnancy outcomes in his female partner ; a father's age at the birth of his offspring on the probability of an adverse...
), and genetic and health screening of donors. In addition, sperm banks may try to ensure that the sperm used in a particular recipient woman comes from a donor whose blood group and genetic profile is compatible with those of the woman.
Sperm donation and rhesus incompatibility
Sperm donation is also used in cases of rhesus incompatibility. This particularly occurs where a woman has a blood typeBlood type
A blood type is a classification of blood based on the presence or absence of inherited antigenic substances on the surface of red blood cells . These antigens may be proteins, carbohydrates, glycoproteins, or glycolipids, depending on the blood group system...
which is rhesus negative, and where her partner is rhesus positive. The woman's body may reject a fetus if it has rhesus positive blood. Anti D
Rho(D) Immune Globulin
Rho Immune Globulin is a medicine given by intramuscular injection that is used to prevent the immunological condition known as Rhesus disease...
injections have been developed and may be used to attempt to avoid this, and these are usually automatically given to rhesus negative women immediately after they give birth to their first child. However, in the past this was either not possible or was not always routinely undertaken where a woman gave birth or had an abortion and she may have trouble carrying a child later in life. Furthermore, for some women, the anti D injection does not provide the entire solution, particularly where there is a medical history of complications during pregnancy which risk the woman's blood and that of the fetus becoming mixed. In such cases, sperm from a rhesus negative donor can provide the solution and a woman may be able to conceive and carry a pregnancy to full term when otherwise this would not be possible. For this reason, sperm from rhesus negative sperm donors is often in great demand, particularly those with the O negative blood group who are universal donors.
Sperm agencies
Sperm may also be donated through an agency rather than through a sperm bank. The agency recruits sperm donors, usually via the Internet, and it also advertises its services on the Internet. Donors may undergo the same kind of checks and tests required by a sperm bank, although clinics and agencies are not necessarily subject to the same regulatory regimes. In the case of an agency, the sperm will be supplied to the recipient woman fresh rather than frozen. A woman chooses a donor and notifies the agency when she requires donations. The agency notifies the donor who must supply his sperm on the appropriate days nominated by the recipient women. The agency will usually provide the sperm donor with a male collection kit usually including a collection condomCondom
A condom is a barrier device most commonly used during sexual intercourse to reduce the probability of pregnancy and spreading sexually transmitted diseases . It is put on a man's erect penis and physically blocks ejaculated semen from entering the body of a sexual partner...
and a container for shipping the sperm. This is collected and delivered by courier and the woman uses the donor's sperm to perform her own artificial insemination
Artificial insemination
Artificial insemination, or AI, is the process by which sperm is placed into the reproductive tract of a female for the purpose of impregnating the female by using means other than sexual intercourse or natural insemination...
, typically without medical supervision. The whole process preserves the anonymity of the parties and it enables a donor to produce sperm in the privacy of his own home. A donor will generally produce samples once or twice during a recipient's fertile period, but a second sample each time may not have the same fecundity of the first sample because it is produced too soon after the first one. Pregnancy rates by this method of sperm donation may vary more than those achieved by sperm banks or fertility clinics. Transit times may vary and these have a significant effect on sperm viability so that if a donor is not located near to a recipient woman the sperm may deteriorate. However, the use of fresh, as opposed to frozen semen will mean that a sample has a greater fecundity and this can produce higher pregnancy rates.
Sperm agencies may impose limits on the number of pregnancies achieved from each donor but in practice this is more difficult to achieve than for sperm banks where the whole process may be more regulated. Most sperm donors only donate for a limited period however, and since sperm supplied by a sperm agency is not processed into a number of different vials, there is a practical limit on the number of pregnancies which are usually produced in this way. A sperm agency will, for the same reason, be less likely than a sperm bank to enable a woman to have subsequent children by the same donor.
Sperm agencies are largely unregulated and, because the sperm is not quarantined, it may carry sexually transmitted diseases. This lack of regulation has led to the competent authorities in some jurisdictions bringing legal action against sperm agencies in certain cases. Agencies typically insist on STI testing for donors, but such tests cannot detect recently-acquired infections. Donors providing sperm in this way may not be protected by laws which apply to donations through a sperm bank or fertility clinic and will, if traced, be regarded as the legal father of each child produced by their sperm, (but see below, Private donors).
Private or "directed" donors
Some donors and recipients choose to arrange donations privately and directly. Recipients may approach a friend, or may obtain a "private" or "directed" donor by advertising. A number of Web sites seek to link such donors and recipients, while advertisements in gay and lesbian publications are common. Although artificial insemination is usually used, the parties may sometimes agree to inseminate naturally (see 'NINI
NI is a two-letter abbreviation and may refer to:-Business:* National Instruments, a U.S. producer of automated test equipment and virtual instrumentation software...
and sperm donation below'). Where a private or directed donor is used, sperm need not be frozen. Such donors may already know the recipients, or if arranged through a broker, may meet the recipients and may therefore become known to the recipient. Some brokerage services facilitate contact that maintains semi-anonymous identities for legal reasons.
Private donations may be free of charge - avoiding the significant costs of a more medicalised insemination - and fresh rather than frozen semen is generally deemed to increase the chances of pregnancy. However, they also carry the higher risks associated with any unscreened sexual or body fluid contact. Legal treatment of donors varies across jurisdictions, and in most jurisdictions, e.g., Sweden, personal and directed donors lack legal safeguards that may be available to anonymous donors. However, the laws of some nations (e.g., New Zealand), recognize written agreements between donors and recipients in a similar way to institutional donations.
Donor payment
The majority of sperm donors who donate their sperm through a sperm bank receive some kind of payment although this is rarely a significant amount. The payments vary from the situation in the United Kingdom where donors are only entitled to their expenses in connection with the donation, to the situation with some US sperm banks where a donor receives a set fee for each donation plus an additional amount for each vial stored. At one prominent California sperm bank for example, TSBC, donors receive roughly $50 for each donation (ejaculation) which has acceptable motility/survival rates both at donation and at a test-thaw a couple of days later. Because of the requirement for the two-day celibacy period before donation, and geographical factors which usually require the donor to travel, it is not a viable way to earn a significant income—and is far less lucrative than selling human eggs. Some private donors may seek remuneration although others donate for altruistic reasons. According to the EU Tissue DirectiveEU Tissue Directive
The EU Tissue Directive sets standards of quality and safety for the donation, procurement, testing, processing, preservation, storage and distribution of human tissues and cells intended for human application. It was adopted by the European Parliament on 7 April 2004 and came into effect between...
donors in EU may only receive compensation, which is strictly limited to making good the expenses and inconveniences related to the donation. A survey among sperm donors in Cryos International Sperm bank showed that altruistic as well as financial motives were the main factors for becoming a donor. However, when the compensation was increased 100% in 2004 (to DKK 500) it had no significant impact on neither the numbers of new donor candidates coming in nor the frequency of donations from the existing donors. When the compensation was reduced to the previous level (DKK 250) again one year later in 2005 there was no effect either. This led to the assumption that altruism is the main motive and that financial compensation is secondary.
Equipment to collect, freeze and store sperm is available to the public notably through certain US outlets, and some donors process and store their own sperm which they then sell via the Internet.
The selling price of processed and stored sperm is considerably more than the sums which are received by donors. Treatments with donor sperm are generally expensive and are seldom available free of charge through national health services. Sperm banks often package treatments into e.g. three cycles, and in cases of IVF or other ART treatments, they may reduce the charge if a patient donates any spare embryos which are produced through the treatment. There is often more demand for fertility treatment with donor sperm than there is donor sperm available, and this has the effect of keeping the cost of such treatments reasonably high.
Samples per child
The number of donor samples (ejaculates) that are required to help give rise to a child varies substantially from donor to donor, as well as from clinic to clinic.However, the following equations generalize the main factors involved:
For intracervical insemination:

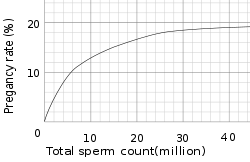
- N is how many children a single sample can help give rise to.
- Vs is the volume of a sample (ejaculate), usually between 1.0 mL and 6.5 mL
- c is the concentration of motile sperm in a sample after freezing and thawing, approximately 5-20 million per ml but varies substantially
- rs is the pregnancy ratePregnancy ratePregnancy rate in infertility treatment is the success rate for pregnancy. It is the percentage of all attempts that leads to pregnancy, with attempts generally referring to menstrual cycles where insemination or any artificial equivalent is used, which may be simple artificial insemination or AI...
per cycle, between 10% to 35% - nr is the total motile sperm count recommended for vaginal insemination (VI) or intra-cervical insemination (ICIICIICI or Ici may mean:* ICI programming language, a computer programming language developed in 1992* Ici , an alternative weekly newspaper in Montreal, CanadaICI is also an abbreviation which may mean:...
), approximately 20 million pr. ml.
The pregnancy rate increases with increasing number of motile sperm used, but only up to a certain degree, when other factors become limiting instead.
With these numbers, one sample would on average help giving rise to 0.1-0.6 children, that is, it actually takes on average 2-5 samples to make a child.
For intrauterine insemination, a centrifugation fraction (fc) may be added to the equation:
- fc is the fraction of the volume that remains after centrifugation of the sample, which may be about half (0.5) to a third (0.33).
On the other hand, only 5 million motile sperm may be needed per cycle with IUI (nr=5 million)
Thus, only 1-3 samples may be needed for a child if used for IUI.
Using ART
Assisted reproductive technology
Assisted reproductive technology is a general term referring to methods used to achieve pregnancy by artificial or partially artificial means. It is reproductive technology used primarily in infertility treatments. Some forms of ART are also used in fertile couples for genetic reasons...
treatments such as IVF can result in one donor sample (or ejaculate) producing on average considerably more than one birth. However, the actual number of births per sample will depend on the actual ART
Assisted reproductive technology
Assisted reproductive technology is a general term referring to methods used to achieve pregnancy by artificial or partially artificial means. It is reproductive technology used primarily in infertility treatments. Some forms of ART are also used in fertile couples for genetic reasons...
method used, the age and medical condition of the woman bearing the child, and the quality of the embryos produced by fertilization. Donor sperm is less commonly used for IVF treatments than for artificial insemination
Artificial insemination
Artificial insemination, or AI, is the process by which sperm is placed into the reproductive tract of a female for the purpose of impregnating the female by using means other than sexual intercourse or natural insemination...
. This is because IVF treatments are usually required only when there is a problem with the female conceiving, or where there is a 'male factor problem' involving the woman's partner. Donor sperm is also used for IVF in surrogacy arrangements where an embryo may be created in an IVF procedure using donor sperm and this is then implanted in a surrogate. In a case where IVF treatments are employed using donor sperm, surplus embryos may be donated to other women or couples and used in embryo transfer
Embryo transfer
Embryo transfer refers to a step in the process of assisted reproduction in which embryos are placed into the uterus of a female with the intent to establish a pregnancy...
procedures. When donor sperm is used for IVF treatments, there is a risk that large numbers of children will be born from a single donor, and many sperm banks therefore limit the amount of semen from each donor which is prepared for IVF use, or they may restrict the period of time for which such a donor donates his sperm to perhaps as little as three months (about nine or ten ejaculates).
Anonymous or non-anonymous
Anonymous sperm donation is where the child and/or receiving couple will never get to know the identity of the donor, and non-anonymous when they will.A donor who makes a non-anonymous sperm donation is termed a known donor, open identity or identity release donor.
Non-anonymous sperm donors are, to a substantially higher degree, driven by altruistic motives for their donations.
In any case, some information about the donor may be released to the woman/couple at the time of treatment. A limited donor information at most includes height, weight, eye, skin and hair colour. In Sweden, this is all the information a receiver gets. In the US, on the other hand, additional information may be given, such as a comprehensive biography and sound/video samples.
For most sperm recipients, anonymity of the donor is not of major importance at the obtainment or tryer-stage,. The main reason for anonymity is that recipients think it would be easiest if the donor was completely out of the picture. However, some recipients regret not having chosen non-anonymous donor years later, for instance when the child desperately wants to know more about the donor anyway.
One in three donor conceived children want information about their biological father.
There is a risk of bias in the information given by clinics or sperm banks regarding anonymity, making anonymous sperm donation seem more favorable than it may actually be, resulting from that anonymous sperm donations are easier for them to handle in the long term, because anonymity does not put the clinic or sperm bank responsible for safely storing donor information for a long period of time. In addition, a majority of donors are anonymous, causing a relative deficit in non-anonymous sperm supply.
In the United States, the trend of wanting to know the identity of donors has resulted in some sperm banks offering exclusively non-anonymous donors.
In law
The law generally protects sperm donors from being responsible for children produced from their donations, and the law also usually provides that sperm donors have no rights over the children which they produce. An exception is Ireland, where the Supreme Court, in the case of McD v. LMcD v. L
McD v. L is a ruling by the Supreme Court of Ireland, handed down on 10 December 2009, that granted a sperm donor visitation rights to a child born via artificial insemination...
(2009), granted visitation rights to a sperm donor and suggested that it would do so in future cases. Recent court cases have been eroding this protection, finding several private sperm-donors financially responsible for their offspring. The widely publicised case of Andy Bathie
Andy Bathie
Andy Bathie is a sperm donor who was sued for child support in the United Kingdom.He is from Enfield in the United Kingdom and worked as a fireman. He became a private sperm donor to a lesbian couple. He was later pursued by the Child Support Agency for maintenance payments, and ordered to pay...
highlights the developing area of fertility law. A major factor in the determination of the sperm donor's support obligation is whether the donor has participate in the child's life in a paternal capacity.
Several countries, e.g. Sweden, Norway, the Netherlands, Britain, Switzerland, Australia and New Zealand only allow non-anonymous sperm donation. The child may, when grown up (15–18 years old), get contact information from the sperm bank about his/her biological father. In Denmark, however, a sperm donor may choose to be either anonymous or non-anonymous. Nevertheless, the initial information which the receiving woman/couple will receive is the same.
Desire to know
For most sperm recipients, anonymity is not of major importance. For the donor conceived children, on the other hand, it may be psychologically burdensome not having the possibility of contacting or knowing almost nothing about the biological father. One in three donor-conceived children want information about their biological father. In case of non-anonymous sperm donation, most of the donor-conceived people contact the clinic as soon as they reach the required age.Approximately 60% of requesters are female. Approximately 40% of requests are from people raised by single women, 30% from those raised by lesbian couples, and 20% from those raised by heterosexual couples. Approximately 60% of them are of the opinion that all sperm donations should include identity release.
Limitation
Where a sperm donor donates sperm through a sperm bank, the sperm bank will generally undertake a number of medical and scientific checks to ensure that the donor produces sperm of sufficient quantity and quality and that the donor is healthy and will not pass diseases through the use of his sperm. The donor's sperm must also withstand the freezing and thawing process necessary to store and quarantine the sperm. The cost to the sperm bank for such tests is considerable. This normally means that clinics may use the same donor to produce a number of pregnancies in a number of different women.The number of children permitted to be born from a single donor varies according to law and practice. These laws are designed to protect the children produced by sperm donation from consanguinity
Consanguinity
Consanguinity refers to the property of being from the same kinship as another person. In that respect, consanguinity is the quality of being descended from the same ancestor as another person...
in later life: they are not intended to protect the sperm donor himself and those donating sperm will be aware that their donations may give rise to numerous pregnancies in different jurisdictions. Such laws, where they exist, vary from state to state, and a sperm bank may also impose its own limits. The latter will be based on the reports of pregnancies which the sperm bank receives, although this relies upon the accuracy of the returns and the actual number of pregnancies may therefore be somewhat higher. Nevertheless, sperm banks frequently impose a lower limit on geographical numbers than some US states and may also limit the overall number of pregnancies which are permitted from a single donor. When calculating the numbers of children born from each donor, the number of siblings produced in any 'family' as a result of sperm donation from the same donor are almost always excluded. There is, of course, no limit to the number of offspring which may be produced from a single donor where he supplies his sperm privately.
Despite the laws limiting the number of offspring, some donors may produce substantial numbers of children, particularly where they donate through different clinics, where sperm is onsold or is exported to different jurisdictions, and where countries or states do not have a central register of donors.
Sperm agencies, in contrast to sperm banks, rarely impose or enforce limits on the numbers of children which may be produced by a particular donor partly because they are not empowered to demand a report of a pregnancy from recipients and they are rarely, if ever, able to guarantee that a woman may have a subsequent sibling by the donor who was the biological father of her first or earlier children.
Sperm shortage
Some countries have a substantial sperm shortage. This has caused fertility tourismFertility tourism
Fertility tourism or reproductive tourism is the practice of traveling to another country for fertility treatments. It may be regarded as a form of medical tourism. The main reasons for fertility tourism are legal regulation of the sought procedure in the home country, or lower price...
to other countries to get the treatment.
For instance, when Sweden banned anonymous sperm donation in 1980, the number of active sperm donors dropped from approximately 200 to 30. Sweden now has an 18 month long waiting list for donor sperm. At least 250 Swedish sperm recipients travel to Denmark annually for insemination. Some of this is also due to the fact that Denmark also allows single women to be inseminated.
After the United Kingdom ended anonymous sperm donation in 2005, the numbers of sperm donors went up, reversing a three-year decline. However, there is still a shortage, and some doctors have suggested raising the limit of children per donor. Sperm exports from Britain are legal (subject to the EU Directive on Tissue Exports) and donors may remain anonymous in this context. Some UK clinics export sperm which may in turn be used in treatments for fertility tourists in other countries. UK clinics also import sperm from Scandinavia. In 2009 one Danish clinic secure the approval of the HFEA to import sperm via registered clinics for use in the UK. The sperm must have been processed, stored and quarantined in compliance with UK regulations. The donors have agreed to be identified when the children produced with their sperm reach the age of eighteen. The number of children produced from such donors in the UK will, of course, be subject to HFEA rules (i.e. currently a limit of ten families,) but the donors' sperm may be used worldwide in accordance with the clinic's own limit of one child per 200.000 of population, subject to national or local limits which apply.
Korea has a sperm shortage because their Bioethics Law prohibits selling and buying of sperm between clinics, and a donor may only help giving rise to a child to one single couple.
Canada also has a shortage because it has been made unlawful to pay people for donating it, requiring recipients who wish to purchase it to import it from the United States.
The United States, on the other hand, has had an increase in sperm donors during the late 2000s recession
Late 2000s recession
The late-2000s recession, sometimes referred to as the Great Recession or Lesser Depression or Long Recession, is a severe ongoing global economic problem that began in December 2007 and took a particularly sharp downward turn in September 2008. The Great Recession has affected the entire world...
, with donors finding the monetary compensation more favorable.
Siblings
Where a woman wishes to have additional children by sperm donation, she will often wish to have these by the same donor. The advantage of having subsequent children by the same donor is that these will be full biological siblings, having the same biological father and mother. Many sperm banks offer a service of storing sperm for future pregnancies, but few will otherwise guarantee that sperm from the original donor will be available in the future.Sperm banks rarely impose limits on the numbers of second or subsequent siblings. Even where there are limits on the use of sperm by a particular donor to a defined number of families (as in the UK) the actual number of children produced from each donor will often be far greater.
Onselling
There is a market for vials of processed sperm and for various reasons a sperm bank may sell-on stocks of vials which it holds (known as 'onselling'). Onselling therefore enables a sperm bank to maximize the sale and disposal of sperm samples which it has processed. The reasons for onselling may be where part of, or even the main business of, a particular sperm bank is to process and store sperm rather than to use it in fertility treatments, or where a sperm bank is able to collect and store more sperm than it can use within nationally set limits. In the latter case a sperm bank may sell on sperm from a particular donor for use in another jurisdiction after the number of pregnancies achieved from that donor has reached its national maximum.A UK sperm bank however, may only onsell sperm before the national limit of ten families has been achieved from one donor within the UK. This means, for example, that a sperm bank may recruit a donor and prepare samples for ICI, IUI and ART use from his donations. After 9 months it is able to release the 10 or so samples donated within the first 3 months, from 6 month quarantine ( approximately 100 vials) and it uses these to achieve 6 pregnancies (although more pregnancies could, of course, be achieved from the number of vials prepared as illustrated). The sperm bank is then able to onsell sperm from that donor to sperm banks and clinics outside the UK and it can illustrate the fecundity of the various types of samples it sells from the pregnancy rates it has achieved. However, from April 2010, the HFEA has imposed limitations on exports of an individual's sperm. The donor must now agree to the export and to the use of his donations to a particular country, and he must be told that regulations for use in that country will vary. He must not have put a limit on the number of births which may be achieved from his donations. The HFEA must be notified of exports of sperm from the UK which will only be granted in accordance with 'special directions'. Individual clinics exporting sperm or onselling to other UK clinics are now responsible for ensuring that the maximum number of births produced from each donor is not exceeded. Prior to 2010 UK clinics could export any quantity of an individual's sperm samples without the consent of the HFEA provided that the donor had consented generally to export and had not imposed a limit on the number of children born from his sperm.
The regulations introduced in April 2010 are intended to ensure that no more than ten families are produced from each donor, regardless of where this occurs. Before this time, some men donated for periods in excess of two years (some for even four or five years) and vials of their sperm were exported without limitation provided that not more than ten families had been produced from their samples in the UK at the time of the export. Donors with particular blood groups or with sperm which produced higher than average pregnancy rates were sometimes offered the opportunity to donate for such prolonged periods. Although this gave rise to considerable numbers of offspring from such donors, local rules applied where the treatments were carried out and there was probably only a low risk of consanguinity. Donors who donated over such periods of time were also aware that their sperm would be used to create numerous offspring.
Embryos may also be onsold. These are usually spare embryos which are created through IVF treatment where a woman achieves the number of pregnancies she requires and the resulting embryos may therefore be disposed of. Donor sperm (and donor eggs) may be used in IVF treatments, and as many as eighteen eggs may be fertilized using one vial of donor sperm, although only the most viable of these will be subsequently implanted in a woman in an attempt to achieve a pregnancy. In the case of the UK, the consent of the donors of both the egg and the sperm which were used to create the embryo must be obtained, and the limit of ten families produced from each donor must not be exceeded.
Onselling is normally only appropriate where the donor remains anonymous. Sperm banks purchasing sperm samples may in turn onsell these to other sperm banks and often engage in the process of exchanging samples with other sperm banks. This is a common practice which enables sperm banks to offer a wider variety of donors, as well as to onsell samples from donors who have reached the maximum permitted number of offspring imposed by, or on, that clinic. Onselling may therefore give rise to numerous pregnancies being produced from individual donors which can sometimes total 100 or more (see above 'Limitation' and the associated link) particularly where a sperm donor donates his sperm for a period of two years or more and where his samples are prepared for IVF use. Sperm from certain donors, such as those with particular blood groups, physical features or intellect, may also be more in demand than sperm from other donors. However, in every case rules as to use and the limitation on the number of pregnancies which apply locally will reduce the risk of consanguinity. The lack of overall records as to use and success will mean that the numbers of pregnancies achieved from the samples of an individual donor will not exist and the donor will not be at risk of knowing the large number of births that were produced from the samples he donated.
Sperm may also be sold on for research or educational purposes, usually after the number of births from the donor concerned has reached its maximum. Sperm is used for genetic and fertility testing, and also for research into birth control.
Donor tracking
Even when the donor had chosen to be anonymous, there are still opportunities for children to find their biological father. Registries and DNA-databases are useful for this purpose. Registries can also help a donor-conceived person identify their siblings, especially half-siblings from other mothers, and avoid accidental incestAccidental incest
Accidental incest is incest that is committed by two partners who do not know they are biologically related. It can occur when two people who are unaware of their biological relationship become sexually intimate, or between siblings who share a room and partake in sexual exploration...
in adulthood.
Tracking by registries
Some donors are non-anonymous, but most are anonymous, i.e. the donor-conceived person does not know the true identity of the donor. Still, he or she may obtain the donor number from the fertility clinic and ascertain whether other children were produced from the same donor. If they were, then those children will be genetic half-siblings. In short, donor registries match people who have the same donor number, and they also provide a method by which a donor may contact the children which he has produced through his donations.Tracking by DNA-databases
However, even sperm donors who have not initiated contact through a registry are now increasingly being traced by their children. In the current era there can be no such thing as guaranteed anonymityAnonymity
Anonymity is derived from the Greek word ἀνωνυμία, anonymia, meaning "without a name" or "namelessness". In colloquial use, anonymity typically refers to the state of an individual's personal identity, or personally identifiable information, being publicly unknown.There are many reasons why a...
. Through the advent of DNA testing and Internet
Internet
The Internet is a global system of interconnected computer networks that use the standard Internet protocol suite to serve billions of users worldwide...
access to extensive database
Database
A database is an organized collection of data for one or more purposes, usually in digital form. The data are typically organized to model relevant aspects of reality , in a way that supports processes requiring this information...
s of information, one sperm donor has recently been traced. In 2005 it was revealed in New Scientist magazine that an enterprising 15-year-old used information from a DNA test and the Internet to identify and contact his father, who was a sperm donor. This has brought into question the ability of sperm donors to stay anonymous.
International comparison
On the global market, Denmark has a well-developed system of sperm export. This success mainly comes from the reputation of Danish sperm donors for being of high quality and, in contrast with the law in the other Nordic countries, gives donors the choice of being either anonymous or non-anonymous to the receiving couple. Furthermore, Nordic sperm donors tend to be tall and highly educated and have altruistic motives for their donations, partly due to the relatively low monetary compensation in Nordic countries. More than 50 countries worldwide are importers of Danish sperm, including ParaguayParaguay
Paraguay , officially the Republic of Paraguay , is a landlocked country in South America. It is bordered by Argentina to the south and southwest, Brazil to the east and northeast, and Bolivia to the northwest. Paraguay lies on both banks of the Paraguay River, which runs through the center of the...
, Canada
Canada
Canada is a North American country consisting of ten provinces and three territories. Located in the northern part of the continent, it extends from the Atlantic Ocean in the east to the Pacific Ocean in the west, and northward into the Arctic Ocean...
, Kenya
Kenya
Kenya , officially known as the Republic of Kenya, is a country in East Africa that lies on the equator, with the Indian Ocean to its south-east...
, and Hong Kong
Hong Kong
Hong Kong is one of two Special Administrative Regions of the People's Republic of China , the other being Macau. A city-state situated on China's south coast and enclosed by the Pearl River Delta and South China Sea, it is renowned for its expansive skyline and deep natural harbour...
. Several UK clinics also export donor sperm but they must take steps to ensure that the maximum number of ten families produced from each donor is not exceeded. The use of the sperm outside the UK will also be subject to local rules. Within the EU there are now regulations governing the transfer of human tissue including sperm between member states to ensure that these take place between registered sperm banks. However, the Food and Drug Administration
Food and Drug Administration
The Food and Drug Administration is an agency of the United States Department of Health and Human Services, one of the United States federal executive departments...
(FDA) of the US has banned import of any sperm, motivated by a risk of mad cow disease
Creutzfeldt-Jakob disease
Creutzfeldt–Jakob disease or CJD is a degenerative neurological disorder that is incurable and invariably fatal. CJD is at times called a human form of mad cow disease, given that bovine spongiform encephalopathy is believed to be the cause of variant Creutzfeldt–Jakob disease in humans.CJD...
, although such a risk is insignificant, since artificial insemination is very different from the route of transmission of mad cow disease. The prevalence of mad cow disease is one in a million, probably less for donors. If prevalence was the case, the infectious proteins would then have to cross the blood-testis barrier
Blood-testis barrier
The blood–testis barrier is a physical barrier between the blood vessels and the seminiferous tubules of the animal testes...
to make transmission possible. Transmission of the disease by an insemination is approximately equal to the risk of getting killed by lightning.
Support for donors
In the UK, the National Gamete Donation TrustNational Gamete Donation Trust
The National Gamete Donation Trust raises awareness of the national shortage of sperm, egg and embryo donors in the UK. Its aim is to recruit donors to alleviate the shortage, and it provides information on egg, sperm and embryo donation and donor recruitment in the UK.It works closely with...
is a charity which provides information, advice and support for people wishing to become egg, sperm or embryo donors. The Trust runs a national helpline and online discussion list for donors to talk to each other.
Psychological and social issues
Common reasons to donate are to help childless couples, and, for some, the monetary compensation. Reluctance to donate may be caused by a sense of ownership and responsibility for the well-being of the offspring.Telling the child
Many donees do not tell the child that they were conceived as a result of sperm donation, or, when non-anonymous donor sperm has been used, they do not tell the child until they are old enough for the clinic to provide the contact information about the donor.However, there are certain circumstances where the child very likely should be told:
- When many relatives know about the insemination, so that the child might find it out from somebody else.
- When the husband carries a significant genetic disease, relieving the child from fear of being a carrier.
Families sharing same donor
Having contact and meeting among families sharing the same donor generally has positive effects. It gives the child an extended familyExtended family
The term extended family has several distinct meanings. In modern Western cultures dominated by nuclear family constructs, it has come to be used generically to refer to grandparents, uncles, aunts, and cousins, whether they live together within the same household or not. However, it may also refer...
and helps give the child a sense of identity by answering questions about the donor. It is more common among open identity-families headed by single women. Less than 1% of those seeking donor-siblings find it a negative experience, and in such cases it is mostly where the parents have disagreed with each other about how the relationship should proceed.
Other family members
Parents of donors, who are the grandparents of donor offspring and may therefore be the oldest surviving progenitors, may regard the donated genetic contribution as a family asset, and may regard the donor conceived people as their grandchildren.Sperm donation and sexuality
Sperm donation can be a morally contentious issue. Couples in heterosexual relationships considering the use of donor sperm through an ARTAssisted reproductive technology
Assisted reproductive technology is a general term referring to methods used to achieve pregnancy by artificial or partially artificial means. It is reproductive technology used primarily in infertility treatments. Some forms of ART are also used in fertile couples for genetic reasons...
method as a solution to childlessness may view it as preserving the sexual integrity of their relationship. However, sperm donation does not maintain the reproductive integrity of a relationship in that the woman's sexual partner is not the biological father of her child, and it is the sperm donor, not the partner, who is the biological father.
However, others point out that the process is essentially a sexual one: a woman's innate sexuality may be the reason why a child is wanted, the donor has to be screened for sexually transmitted diseases which could be passed on through the use of his sperm, and the donor has to sexually stimulate himself in order to produce the sperm samples which are used for achieving pregnancies in women to whom he is not related. Some would argue that it is impossible to distinguish sexuality from reproduction, and that the very reason for preserving sexual integrity is to preserve reproductive integrity.
NI and sperm donation
Where a donor inseminates a woman naturally by having sexual intercourse with her for the sole reason of enabling the woman to achieve a pregnancy, this is known as natural insemination or NINI
NI is a two-letter abbreviation and may refer to:-Business:* National Instruments, a U.S. producer of automated test equipment and virtual instrumentation software...
.
For many donors and recipient women, the lack of physical sexual contact between the parties is one of the essential advantages of sperm donation. Whether the donor is anonymous or not, and whether or not the parties meet, the fact that the reproductive process takes place without genital contact serves to place the procedure on a level which is not readily identified as 'sexual' within the generally understood meaning (see 'Sperm donation and sexuality' above).
However, the very fact that sperm donation involves the placing of a man's gamete in the reproductive tract of a woman for the sole reason of enabling the woman to have that man's child does mean that the process is an intensely personal one which involves the highest degree of intimate contact. In this context, personal, physical intimacy may be seen as secondary to the reproductive process which is taking place. A 'natural' conception also avoids the need to be subjected to mechanical procedures which may or may not involve the intervention of third parties.
NI almost invariably produces higher pregnancy rates than ICI, which is the usual method of artificial insemination deployed in private donor arrangements. This is because NI
NI
NI is a two-letter abbreviation and may refer to:-Business:* National Instruments, a U.S. producer of automated test equipment and virtual instrumentation software...
involves the fresh and immediate deposit of the donor's sperm high up in a woman's vagina near to the entrance to the womb. By comparison, semen used for artificial insemination
Artificial insemination
Artificial insemination, or AI, is the process by which sperm is placed into the reproductive tract of a female for the purpose of impregnating the female by using means other than sexual intercourse or natural insemination...
must normally be allowed to liquefy to enable it be used in a syringe (unless a conception cap or conception device
Conception device
A conception device is a medical device which is used to assist in the achievement of a pregnancy, often, but not always, by means other than sexual intercourse or NI...
using fresh semen is used for the artificial insemination), and fertility clinics and sperm banks always use sperm which has been liquefied, frozen and thawed, all of which reduces its fecundity. Ensuring that the sperm is deposited correctly in the vagina requires a certain knowledge or skill and the failure correctly to perform artificial insemination is thought to lead to many failures to conceive. Furthermore, medical evidence shows that semen quality
Semen quality
Semen quality is a measure of the ability of semen to accomplish fertilization. Thus, it is a measure of fertility in a man. It is the sperm in the semen that are of importance, and therefore semen quality involves both sperm quantity and quality...
is likely to be substantially higher and its fertility therefore greater where semen is produced during sexual intercourse rather than by masturbation.
The availability of screening and home testing for sexually transmitted diseases, ovulation timings and male and female fertility also make the procedure safer and more reliable than was previously possible.
Consequently, an increasing number of private sperm donors now offer NI
NI
NI is a two-letter abbreviation and may refer to:-Business:* National Instruments, a U.S. producer of automated test equipment and virtual instrumentation software...
as an alternative to the use of artificial means, or they will do so after attempts to achieve a conception by artificial insemination have failed, and similarly, an increasing number of women are seeking a natural conception from a donor. Some fertility clinics, notably in India and China also offer donors and surrogate women who will attempt to achieve pregnancies by NI as a more effective and cheaper alternative to ART methods. Where NI
NI
NI is a two-letter abbreviation and may refer to:-Business:* National Instruments, a U.S. producer of automated test equipment and virtual instrumentation software...
is used to achieve a pregnancy by a donor, the ethical considerations are significantly different from considerations where a pregnancy is achieved by artificial means. Whatever method is used, sperm donation is, of course, essentially the attempt to impregnate a woman with the sperm of a man who is not her partner, and neither AI nor NI preserves the reproductive integrity of the relationship a woman has with her partner.
Sperm donation and social issues
The use of sperm donation is increasingly popular among unmarried women and single or coupled lesbians. Indeed, some sperm banks and fertility clinics, particularly in the US, Denmark and the UK have a predominance of women being treated with donor sperm who come within these groups and their publicity is aimed at them. This produces many ethical issues around the ideals of conventional parenting and has wider issues for society as a whole, including the issues of the role of men as parents, the issue of family support for children, and the issue of financial support for women with children.The growth of sperm banks and fertility clinics, the use of sperm agencies and the availability of anonymous donor sperm have assisted in making the use of sperm donation a more respectable, and therefore a more socially acceptable, procedure. The intervention of doctors and others may be seen as making the whole process merely another medical one, where inseminations may be referred to as 'treatments' and donor children as 'resulting from the use of' a donor's sperm, rather than as the biological children of a donor. Still, a study has indicated that both men and women view the use of donor sperm with more skepticism compared with the use of donor eggs, suggesting a unique underlying perception regarding the use of male donor gametes.
As acceptance of sperm donation has generally increased, so has the level of questioning as to whether 'artificial' means of conception are necessary, and some donor children too, have been critical of the procedures which were taken to bring them into the world. Against this background has been the increase in the use of NI
NI
NI is a two-letter abbreviation and may refer to:-Business:* National Instruments, a U.S. producer of automated test equipment and virtual instrumentation software...
as a method of sperm donation. However, while some donors may be willing to offer this as a method of impregnation, it has many critics and it also raises further legal and social challenges.
Some donor children grow up wishing to find out who their fathers were, but others may be wary of embarking on such a search since they fear they may find scores of half-siblings who have been produced from the same sperm donor. Even though local laws or rules may restrict the numbers of offspring from a single donor, there are no worldwide limitations or controls and most sperm banks will onsell and export all their remaining stocks of vials of sperm when local maxima have been attained (see 'onselling' above).
One item of research has suggested that donor children have a greater likelihood of substance abuse
Substance abuse
A substance-related disorder is an umbrella term used to describe several different conditions associated with several different substances .A substance related disorder is a condition in which an individual uses or abuses a...
, mental illness
Mental illness
A mental disorder or mental illness is a psychological or behavioral pattern generally associated with subjective distress or disability that occurs in an individual, and which is not a part of normal development or culture. Such a disorder may consist of a combination of affective, behavioural,...
and criminal behavior when grown.http://www.slate.com/id/2256212 However, its motivation and credibility have been questioned.http://www.bionews.org.uk/page_65970.asp
History
In 1790, Scottish anatomist and surgeon Dr. John Hunter reported that he had successfully inseminated the wife of a linen draper, using her husband's sperm.In 1884 Professor William Pancoast at Philadelphia's Jefferson Medical College performed an insemination on the wife of a sterile Quaker merchant. Instead of taking the sperm from the husband, the professor chloroformed the woman, then let his medical students vote which one of among them was "best looking", with that elected one providing the sperm for the insemination. After talking to the husband, they decided it was best not to let the woman know. At the husband's request, his wife was never told how she became pregnant. As a result of this medical school experiment, the merchant's wife gave birth to a son, who became the first known child by donor insemination (DI).
For over a decade nothing more was heard on the subject. Then, in 1909, a letter by Addison Davis Hard appeared in the American journal Medical World, highlighting the procedure which had taken place at the Jefferson Medical College in Philadelphia in 1884—twenty-five years earlier.
From that time, a very few doctors performed donor insemination privately and such procedures were regarded as private by the parties. Records were usually not maintained so that donors could not be identified for paternity proceedings. Only fresh sperm could be used and it is thought that this largely came from the doctors and their own male staff, although a few private donors were sometimes used who were able to donate on a regular basis at short notice as required.
The first successful human pregnancy using frozen sperm was in 1953.
DI remained virtually unknown to the public until 1954. In that year the first comprehensive account of the process was published in The British Medical Journal.
Donor insemination provoked heated public debate. The Archbishop of Canterbury established the first in a long procession of commissions that, over the years, inquired into the development of the practice. It was at first condemned by the Lambeth Conference and recommended that it be made a criminal offence. A Parliamentary Commission agreed. In Italy, the Pope declared DI a sin, and proposed that anyone using the procedure be sent to prison.
In the same year, 1954, the Supreme Court of Cook County in the USA ruled that regardless of a husband's consent, DI was "contrary to public policy and good morals, and considered adultery on the mother's part." The sperm donor was not married to the child's mother, and therefore, regardless of her husband's consent, the woman's insemination constituted adultery. The ruling went on to say that, "A child so conceived, was born out of wedlock and therefore illegitimate. As such, it is the child of the mother, and the father has no rights or interest in said child." adultery.
However, the following year, Georgia became the first state to pass a statute legitimizing children conceived by DI, on the condition that both the husband and wife consented in advance in writing to the procedure.
In 1973 the Commissioners on Uniform State Laws, and a year later, the American Bar Association, approved the Uniform Parentage Act. This act provides that if a wife is artificially inseminated with donor semen under a physician's supervision, and with her husband's consent, the husband is treated for legal purposes as if he were the natural father of the DI child. This law has been followed by similar legislation in most states of the US.
In 1975, the first commercial sperm bank, Xytex Corporation, was opened in Augusta, GA by Dr. Armand Karow Jr. and Dr. John Black.
In the UK, the Warnock Committee looked at the whole issue of the donation of gametes and assisted reproduction techniques. Donor insemination was already available in the UK through unregulated clinics such as BPAS. The Committee's Report led to the passing of the Human Fertilisation and Embryology Act in 1990. This provided for a system of licensing for fertility clinics and procedures. It also provided that, where a man donates sperm at a licensed clinic in the UK and his sperm is used at a UK clinic to impregnate a woman, the man is not legally responsible for the resulting child.
The 1990 Act also established a central UK central register of donors and donor births to be maintained by the Human Fertilisation and Embryology Authority (the 'HFEA'), a supervisory body established by the Act. Following the Act, where any woman has a child by a man who donates his sperm through a licensed clinic as the result of the use of that man's sperm through artificial insemination or IVF at a licensed UK clinic, details of the child and of the donor, who is its biological father, are required to recorded on the register. This measure was intended to reduce the risk of consanguinity as well as to enforce the limit on the number of births permitted by each donor. The natural child of any donor has access to non-identifying information about him from the child's eighteenth birthday.
The emphasis in the 1990 Act in the UK was on protecting the unborn child. However, a general shortage of donor sperm at the end of the 20th century, exacerbated by the announcement of the removal of anonymity in the UK, led to concerns about the excessive use of the sperm of some donors. These concerns centered on the export and exchange of donor sperm with overseas clinics, and also the interpretation of the term 'sibling use' to include donated embryos produced from one sperm donor, and successive births by surrogates using eggs from different women but sperm from the same sperm donor. Donors were informed that up to ten births could be produced from their sperm, but few probably appreciated that the words 'other than in exceptional circumstances' in the consent could lead to so many pregnancies. These concerns led to the SEED Report commissioned by the HFEA which was in turn followed by new legislation and rules which finally recognised the interests of donors. Where a man donates his sperm through a UK clinic, that sperm is not now permitted to give rise to more than ten families wherever it is used.
In many western countries, sperm donation is now a largely accepted procedure. In the US and elsewhere, the growth in the number of sperm banks has been considerable and there has been a general commercialisation of the procedure. Recent years have also seen the trend away from sperm donation as a method of allowing heterosexual couples to produce children, as other fertility treatments have become more sophisticated, and towards the use of donated sperm by single women and single and coupled lesbians of the procedure. A sperm bank
Sperm bank
A sperm bank, semen bank or cryobank is a facility that collects and stores human sperm mainly from sperm donors, primarily for the purpose of achieving pregnancies through third party reproduction, notably by artificial insemination...
in the US pioneered the use of on-line search catalogues for donor sperm, and these facilities are now widely available on the websites of sperm banks and fertility clinics.
Controls have been applied in a number of countries such as the UK to prohibit anonymous sperm donation. The Internet has provided a way for people to find donors through sperm donation websites and fertility forums. Recent years have also seen a growth in the number of donors willing to impregnate by NI
NI
NI is a two-letter abbreviation and may refer to:-Business:* National Instruments, a U.S. producer of automated test equipment and virtual instrumentation software...
as social attitudes to sperm donation generally have changed and more and more women are questioning the need for artificial procedures. Controls over the number of families which are allowed to be created from each donor in many countries have led to the growth of fertility tourism
Fertility tourism
Fertility tourism or reproductive tourism is the practice of traveling to another country for fertility treatments. It may be regarded as a form of medical tourism. The main reasons for fertility tourism are legal regulation of the sought procedure in the home country, or lower price...
and to the increase in onselling and export by some sperm banks.
Fictional representation
Movie plots involving artificial insemination by donor are seen in Made in AmericaMade in America (film)
Made in America is a 1993 comedy film released on May 28, 1993 by Warner Bros. starring Whoopi Goldberg and Ted Danson, and featuring Nia Long, Jennifer Tilly and Will Smith.-Plot:...
, Road Trip, The Back-Up Plan
The Back-Up Plan
The Back-up Plan is a 2010 romantic comedy film, starring Jennifer Lopez and Alex O'Loughlin. It was released theatrically in the U.S. on April 23, 2010, and later in other regions...
, The Kids Are Alright (film)
The Kids Are Alright (film)
The Kids Are Alright is a 1979 rockumentary film about the English rock band The Who, including live performances, promotional films and interviews from 1964 to 1978.-Production:...
, The Switch (film), and Baby Mama
Baby Mama (film)
Baby Mama is a 2008 comedy film from Universal Pictures written and directed by Michael McCullers and starring Tina Fey, Amy Poehler, Sigourney Weaver, Greg Kinnear, and Dax Shepard.-Plot:...
, the latter also involving surrogacy
Surrogacy
Surrogacy is an arrangement in which a woman carries and delivers a child for another couple or person. This woman may be the child's genetic mother , or she may carry the pregnancy to delivery after having an embryo, to which she has no genetic relationship whatsoever, transferred to her uterus...
.
Films and other fiction depicting emotional struggles of assisted reproductive technology
Assisted reproductive technology
Assisted reproductive technology is a general term referring to methods used to achieve pregnancy by artificial or partially artificial means. It is reproductive technology used primarily in infertility treatments. Some forms of ART are also used in fertile couples for genetic reasons...
have had an upswing first in the latter part of the 2000s decade, although the techniques have been available for decades. Yet, the amount of people that can relate to it by personal experience in one way or another is ever growing, and the variety of trials and struggles is huge.
See also
- Accidental incestAccidental incestAccidental incest is incest that is committed by two partners who do not know they are biologically related. It can occur when two people who are unaware of their biological relationship become sexually intimate, or between siblings who share a room and partake in sexual exploration...
- Artificial inseminationArtificial inseminationArtificial insemination, or AI, is the process by which sperm is placed into the reproductive tract of a female for the purpose of impregnating the female by using means other than sexual intercourse or natural insemination...
- Conception deviceConception deviceA conception device is a medical device which is used to assist in the achievement of a pregnancy, often, but not always, by means other than sexual intercourse or NI...
- Donor conceived peopleDonor conceived peopleA donor offspring, or donor conceived person, is conceived via the donation of sperm or ova , or both, either from two separate donors or from a couple...
- Egg donorEgg donorEgg donation is the process by which a woman provides one or several eggs for purposes of assisted reproduction or biomedical research. For assisted reproduction purposes, egg donation involves the process of in vitro fertilization as the eggs are fertilized in the laboratory. After the eggs...
- InfertilityInfertilityInfertility primarily refers to the biological inability of a person to contribute to conception. Infertility may also refer to the state of a woman who is unable to carry a pregnancy to full term...
- IVF
- McD v. LMcD v. LMcD v. L is a ruling by the Supreme Court of Ireland, handed down on 10 December 2009, that granted a sperm donor visitation rights to a child born via artificial insemination...
- Posthumous sperm retrievalPosthumous sperm retrievalPosthumous sperm retrieval is a procedure in which spermatozoa are extracted from a man after he has been pronounced legally brain dead. There has been significant debate over the ethicality and legality of the procedure, and on the legal rights of the child and surviving parent if the gametes are...
- Rh DiseaseRh diseaseRh disease is one of the causes of hemolytic disease of the newborn...
- Semen qualitySemen qualitySemen quality is a measure of the ability of semen to accomplish fertilization. Thus, it is a measure of fertility in a man. It is the sperm in the semen that are of importance, and therefore semen quality involves both sperm quantity and quality...
- Sperm bankSperm bankA sperm bank, semen bank or cryobank is a facility that collects and stores human sperm mainly from sperm donors, primarily for the purpose of achieving pregnancies through third party reproduction, notably by artificial insemination...
- SurrogacySurrogacySurrogacy is an arrangement in which a woman carries and delivers a child for another couple or person. This woman may be the child's genetic mother , or she may carry the pregnancy to delivery after having an embryo, to which she has no genetic relationship whatsoever, transferred to her uterus...
- Third party reproductionThird party reproductionThird party reproduction refers to a process where another person provides sperm or eggs or where another woman provides her uterus so that a woman can have a child. Thus the reproductive process goes beyond the traditional father-mother model. However, the third party's involvement is limited to...
External links
- Sperm donation in the UK (the UK's regulatory body - lists all UK clinics offering sperm donation)
- Affiliate Resurrection Review
Not valid.

