Antibiotic resistance
Encyclopedia
Antibiotic resistance is a type of drug resistance
where a microorganism
is able to survive exposure to an antibiotic
. While a spontaneous or induced genetic mutation in bacteria may confer resistance to antimicrobial drugs, gene
s that confer resistance can be transferred between bacteria in a horizontal
fashion by conjugation
, transduction
, or transformation
. Thus a gene for antibiotic resistance which had evolved via natural selection
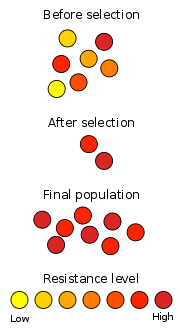
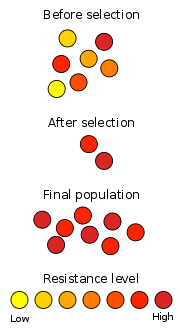
may be shared. Evolutionary stress such as exposure to antibiotics then selects for the antibiotic resistant trait. Many antibiotic resistance genes reside on plasmids, facilitating their transfer. If a bacterium carries several resistance genes, it is called multidrug resistant (MDR) or, informally, a superbug or super bacterium.
Genes for resistance to antibiotics, like the antibiotics themselves, are ancient. However, the increasing prevalence of antibiotic-resistant bacterial infections seen in clinical practice stems from antibiotic use both within human medicine and veterinary medicine. Any use of antibiotics can increase selective pressure in a population of bacteria to allow the resistant bacteria to thrive and the susceptible bacteria to die off. As resistance towards antibiotics becomes more common, a greater need for alternative treatments arises. However, despite a push for new antibiotic therapies there has been a continued decline in the number of newly approved drugs. Antibiotic resistance therefore poses a significant problem.
Certain antibiotic classes are highly associated with colonisation with superbugs compared to other antibiotic classes. The risk for colonisation increases if there is a lack of sensitivity (resistance) of the superbugs to the antibiotic used and high tissue penetration, as well as broad-spectrum activity against "good bacteria". In the case of MRSA
, increased rates of MRSA infections are seen with glycopeptides, cephalosporin
s and especially quinolones. In the case of colonisation with Clostridium difficile
the high risk antibiotics include cephalosporins and in particular quinolones and clindamycin
.
In a paper published in the recent edition of the journal Nature, researchers at McMaster University say they have discovered that antibiotic-resistant genes existed in soil bacteria at the same time that now-extinct mammoths, early horses and bison roamed Canada's North.
Inappropriate prescribing of antibiotics has been attributed to a number of causes, including: people who insist on antibiotics, physicians simply prescribe them as they feel they do not have time to explain why they are not necessary, physicians who do not know when to prescribe antibiotics or else are overly cautious for medical legal reasons. For example, a third of people believe that antibiotics are effective for the common cold
and 22% of people do not finish a course of antibiotics primarily because they feel better (varying from 10% to 44%, depending on the country). Compliance with once-daily antibiotics is better than with twice-daily antibiotics. Suboptimum antibiotic concentrations in critically ill people increase the frequency of antibiotic resistance organisms. While taking antibiotics doses less than those recommended may increase rates of resistance, shortening the course of antibiotics may actually decrease rates of resistance.
Poor hand hygiene by hospital staff has been associated with the spread of resistant organisms and an increase in hand washing compliance results in decreased rates of these organisms.
The World Health Organization concluded antibiotics as growth promoters in animal feeds should be prohibited in the absence of risk assessments. In 1998, European Union health ministers voted to ban four antibiotics widely used to promote animal growth (despite their scientific panel's recommendations). Regulation banning the use of antibiotics in European feed, with the exception of two antibiotics in poultry feeds, became effective in 2006. In Scandinavia, there is evidence that the ban has led to a lower prevalence of antimicrobial resistance in (nonhazardous) animal bacterial populations. In the USA, federal agencies do not collect data on antibiotic use in animals, but animal-to-human spread of drug-resistant organisms has been demonstrated in research studies. Antibiotics are still used in U.S. animal feed, along with other ingredients which have safety concerns.
Growing U.S. consumer concern about using antibiotics in animal feed has led to a niche market of "antibiotic-free" animal products, but this small market is unlikely to change entrenched, industry-wide practices.
In 2001, the Union of Concerned Scientists estimated that greater than 70% of the antibiotics used in the US are given to food animals (for example, chickens, pigs and cattle) in the absence of disease. In 2000, the US Food and Drug Administration (FDA) announced their intention to revoke approval of fluoroquinolone use in poultry production because of substantial evidence linking it to the emergence of fluoroquinolone-resistant Campylobacter
infections in humans. The final decision to ban fluoroquinolones from use in poultry production was not made until five years later because of challenges from the food animal and pharmaceutical industries. During 2007, two federal bills (S. 549 and H.R. 962) aim at phasing out "nontherapeutic" antibiotics in US food animal production.
 Antibiotic resistance can be a result of horizontal gene transfer
Antibiotic resistance can be a result of horizontal gene transfer
, and also of unlinked point mutations in the pathogen
genome
at a rate of about 1 in 108 per chromosomal replication. The antibiotic action against the pathogen can be seen as an environmental pressure; those bacteria which have a mutation allowing them to survive will live on to reproduce. They will then pass this trait to their offspring, which will result in the evolution of a fully resistant colony.
The four main mechanisms by which microorganisms exhibit resistance to antimicrobials are:
There are three known mechanisms of fluoroquinolone resistance. Some types of efflux
pumps can act to decrease intracellular quinolone
concentration. In Gram-negative bacteria, plasmid-mediated resistance genes produce proteins that can bind to DNA gyrase
, protecting it from the action of quinolones. Finally, mutations at key sites in DNA gyrase or topoisomerase IV
can decrease their binding affinity to quinolones, decreasing the drug's effectiveness. Research has shown the bacterial protein LexA
may play a key role in the acquisition of bacterial mutations giving resistance to quinolones and rifampicin.
Antibiotic resistance can also be introduced artificially into a microorganism through laboratory protocols, sometimes used as a selectable marker
to examine the mechanisms of gene transfer or to identify individuals that absorbed a piece of DNA that included the resistance gene and another gene of interest. A recent study demonstrated the extent of horizontal gene transfer
among Staphylococcus to be much greater than one previously expected, and encompasses genes with functions beyond antibiotic resistance and virulence, and beyond genes residing within the mobile genetic elements
.
(colloquially known as "Staph aureus" or a "Staph infection") is one of the major resistant pathogens. Found on the mucous membranes and the human skin
of around a third of the population, it is extremely adaptable to antibiotic pressure. It was one of the earlier bacteria in which penicillin
resistance was found—in 1947, just four years after the drug started being mass-produced. Methicillin
was then the antibiotic of choice, but has since been replaced by oxacillin
due to significant kidney toxicity. Methicillin-resistant Staphylococcus aureus
(MRSA) was first detected in Britain in 1961, and is now "quite common" in hospitals. MRSA was responsible for 37% of fatal cases of sepsis
in the UK
in 1999, up from 4% in 1991. Half of all S. aureus infections in the US
are resistant to penicillin, methicillin, tetracycline and erythromycin
.
This left vancomycin
as the only effective agent available at the time. However, strains with intermediate (4-8 μg/ml) levels of resistance, termed glycopeptide-intermediate Staphylococcus aureus (GISA) or vancomycin-intermediate Staphylococcus aureus (VISA), began appearing in the late 1990s. The first identified case was in Japan in 1996, and strains have since been found in hospitals in England, France and the US. The first documented strain with complete (>16 μg/ml) resistance to vancomycin, termed vancomycin-resistant Staphylococcus aureus
(VRSA) appeared in the United States in 2002.
A new class of antibiotics, oxazolidinones
, became available in the 1990s, and the first commercially available oxazolidinone, linezolid
, is comparable to vancomycin in effectiveness against MRSA. Linezolid-resistance in S. aureus was reported in 2003.
Community-acquired MRSA (CA-MRSA)has now emerged as an epidemic that is responsible for rapidly progressive, fatal diseases, including necrotizing pneumonia, severe sepsis
and necrotizing fasciitis
. MRSA is the most frequently identified antimicrobial drug-resistant pathogen in US hospitals. The epidemiology
of infections caused by MRSA is rapidly changing. In the past 10 years, infections caused by this organism have emerged in the community. The two MRSA clones in the United States most closely associated with community outbreaks, USA400 (MW2 strain, ST1 lineage) and USA300, often contain Panton-Valentine leukocidin
(PVL) genes and, more frequently, have been associated with skin and soft tissue infections. Outbreaks of CA-MRSA infections have been reported in correctional facilities, among athletic teams, among military recruits, in newborn nurseries, and among men who have sex with men. CA-MRSA infections now appear to be endemic in many urban regions and cause most CA-S. aureus infections.
(Group A Streptococcus: GAS) infections can usually be treated with many different antibiotics. Early treatment may reduce the risk of death from invasive group A streptococcal disease. However, even the best medical care does not prevent death in every case. For those with very severe illness, supportive care in an intensive care unit may be needed. For persons with necrotizing fasciitis, surgery often is needed to remove damaged tissue. Strains of S. pyogenes resistant to macrolide
antibiotics have emerged; however, all strains remain uniformly sensitive to penicillin
.
Resistance of Streptococcus pneumoniae
to penicillin and other beta-lactams is increasing worldwide. The major mechanism of resistance involves the introduction of mutations in genes encoding penicillin-binding proteins. Selective pressure is thought to play an important role, and use of beta-lactam antibiotics has been implicated as a risk factor for infection and colonization. S. pneumoniae is responsible for pneumonia
, bacteremia
, otitis media
, meningitis
, sinusitis
, peritonitis
and arthritis
.
Multidrug-resistant Enterococcus faecalis
and Enterococcus faecium
are associated with nosocomial infections
. Among these strains, penicillin
-resistant Enterococcus
was seen in 1983, vancomycin-resistant Enterococcus
in 1987, and linezolid
-resistant Enterococcus
in the late 1990s.
is a highly prevalent opportunistic pathogen. One of the most worrisome characteristics of P. aeruginosa is its low antibiotic susceptibility, which is is attributable to a concerted action of multidrug efflux pumps
with chromosomally encoded antibiotic resistance genes (for example, mexAB-oprM, mexXY, etc.) and the low permeability of the bacterial cellular envelopes. Besides intrinsic resistance, P. aeruginosa easily evolves specific resistance either by mutation
in chromosomally-encoded genes, or by the horizontal gene transfer of antibiotic resistance determinants. Evolution of multidrug resistance
by P. aeruginosa isolates requires several genetic events that include acquisition of different mutations and/or horizontal transfer of antibiotic resistance genes. Hypermutation favours the selection of mutation-driven antibiotic resistance in P. aeruginosa strains, producing chronic infections, whereas the clustering of several different antibiotic resistance genes in integron
s favours the concerted acquisition of antibiotic resistance determinants. Some recent studies have shown phenotypic resistance associated with biofilm
formation or the emergence of small-colony-variants may be important in the response of P. aeruginosa populations to antibiotic
s treatment.
is a nosocomial pathogen that causes diarrheal disease in hospitals world wide. Clindamycin
-resistant C. difficile was reported as the causative agent of large outbreaks of diarrheal disease in hospitals in New York, Arizona, Florida and Massachusetts between 1989 and 1992. Geographically dispersed outbreaks of C. difficile strains resistant to fluoroquinolone antibiotics, such as ciprofloxacin and levofloxacin, were also reported in North America in 2005.
and Salmonella
come directly from contaminated food. When both bacteria are spread, serious health conditions arise. Many people are hospitalized each year after becoming infected, with some dying as a result. By 1993, E. coli resistant to multiple fluoroquinolone variants was documented.
(CDC) reported an increasing number of Acinetobacter baumannii
bloodstream infections in patients at military medical facilities in which service members injured in the Iraq
/Kuwait
region during Operation Iraqi Freedom and in Afghanistan
during Operation Enduring Freedom were treated. Most of these showed multidrug resistance
(MRAB), with a few isolates resistant to all drugs tested.
to isoniazid
, rifampin, and other common treatments has become an increasingly relevant clinical challenge.
infection, which is a leading cause of nosocomial diarrhea
in the United States, and a major cause of death, worldwide.
There is clinical evidence that topical dermatological preparations, such as those containing tea tree oil
and thyme
oil, may be effective in preventing transmittal of CA-MRSA. In addition, other phytotherapeutic
medicines, too, can reduce the use of antibiotics or eliminate their use entirely.
Vaccine
s do not suffer the problem of resistance because a vaccine enhances the body's natural defenses, while an antibiotic operates separately from the body's normal defenses. Nevertheless, new strains may evolve
that escape immunity induced by vaccines; for example an update influenza vaccine is needed each year.
While theoretically promising, antistaphylococcal vaccines have shown limited efficacy, because of immunological variation between Staphylococcus species, and the limited duration of effectiveness of the antibodies produced. Development and testing of more effective vaccines is under way.
The Australian Commonwealth Scientific and Industrial Research Organization (CSIRO), realizing the need for the reduction of antibiotic use, has been working on two alternatives. One alternative is to prevent diseases by adding cytokine
s instead of antibiotics to animal feed. These proteins are made in the animal body "naturally" after a disease and are not antibiotics, so they do not contribute to the antibiotic resistance problem. Furthermore, studies on using cytokines have shown they also enhance the growth of animals like the antibiotics now used, but without the drawbacks of nontherapeutic antibiotic use. Cytokines have the potential to achieve the animal growth rates traditionally sought by the use of antibiotics without the contribution of antibiotic resistance associated with the widespread nontherapeutic uses of antibiotics currently used in the food animal production industries. Additionally, CSIRO is working on vaccines for diseases.
, an approach that has been extensively researched and used as a therapeutic agent for over 60 years, especially in the Soviet Union
, is an alternative that might help with the problem of resistance. Phage therapy was widely used in the United States until the discovery of antibiotics, in the early 1940s. Bacteriophages or "phages" are viruses that invade bacterial cells and, in the case of lytic phages, disrupt bacterial metabolism and cause the bacterium to lyse
. Phage therapy is the therapeutic use of lytic bacteriophages to treat pathogenic bacterial infections.
Bacteriophage therapy is an important alternative to antibiotics in the current era of multidrug resistant pathogens. A review of studies that dealt with the therapeutic use of phages from 1966–1996 and few latest ongoing phage therapy projects via internet showed: phages were used topically, orally or systemically in Polish and Soviet studies. The success rate found in these studies was 80–95% with few gastrointestinal or allergic side effects. British studies also demonstrated significant efficacy of phages against Escherichia coli
, Acinetobacter
spp., Pseudomonas
spp. and Staphylococcus aureus
. US studies dealt with improving the bioavailability of phage. Phage therapy may prove as an important alternative to antibiotics for treating multidrug resistant pathogens.
(R&D) efforts have provided new drugs in time to treat bacteria that became resistant to older antibiotics. That is no longer the case. The potential crisis at hand is the result of a marked decrease in industry R&D, and the increasing prevalence of resistant bacteria. Infectious disease physicians are alarmed by the prospect that effective antibiotics may not be available to treat seriously ill patients in the near future.
As bacterial antibiotic resistance continues to exhaust the supply of effective antibiotics, a global public health disaster appears likely. Poor financial investment in antibiotic research has exacerbated the situation. A call to arms raised by several prestigious scientific organisations a few years ago rallied the scientific community, and now the scope of antibacterial research has broadened considerably.
The pipeline of new antibiotics is drying up. Major pharmaceutical companies are losing interest in the antibiotics market because these drugs may not be as profitable as drugs that treat chronic (long-term) conditions and lifestyle issues.
Archaeocin
s is the name given to a new class of potentially useful antibiotics that are derived from the Archaea
group of organisms. Eight archaeocins have been partially or fully characterized, but hundreds are believed to exist, especially within the haloarchaea
. The prevalence of archaeocins is unknown simply because no one has looked for them. The discovery of new archaeocins hinges on recovery and cultivation of archaeal organisms from the environment. For example, samples from a novel hypersaline field site, Wilson Hot Springs, recovered 350 halophilic organisms; preliminary analysis of 75 isolates showed that 48 were archaeal and 27 were bacterial.
In research published on October 17, 2008 in Cell
, a team of scientists pinpointed the place on bacteria where the antibiotic myxopyronin
launches its attack, and why that attack is successful. The myxopyronin binds to and inhibits the crucial bacterial enzyme, RNA polymerase
. The myxopyronin changes the structure of the switch-2 segment of the enzyme, inhibiting its function of reading and transmitting DNA code. This prevents RNA polymerase from delivering genetic information to the ribosomes, causing the bacteria to die.
One of the major causes of antibiotic resistance is the decrease of effective drug concentrations at their target place, due to the increased action of ABC transporters. Since ABC transporter blockers can be used in combination with current drugs to increase their effective intracellular concentration, the possible impact of ABC transporter inhibitors is of great clinical interest. ABC transporter blockers that may be useful to increase the efficacy of current drugs have entered clinical trials and are available to be used in therapeutic regimens.
. By constructing a plasmid
which contains an antibiotic resistance gene as well as the gene being engineered or expressed, a researcher can ensure that when bacteria replicate, only the copies which carry along the plasmid survive. This ensures that the gene being manipulated passes along when the bacteria replicates.
The most commonly used antibiotics in genetic engineering are generally "older" antibiotics which have largely fallen out of use in clinical practice. These include:
Industrially the use of antibiotic resistance is disfavored since maintaining bacterial cultures would require feeding them large quantities of antibiotics. Instead, the use of auxotrophic bacterial strains (and function-replacement plasmids) is preferred.
Drug resistance
Drug resistance is the reduction in effectiveness of a drug such as an antimicrobial or an antineoplastic in curing a disease or condition. When the drug is not intended to kill or inhibit a pathogen, then the term is equivalent to dosage failure or drug tolerance. More commonly, the term is used...
where a microorganism
Microorganism
A microorganism or microbe is a microscopic organism that comprises either a single cell , cell clusters, or no cell at all...
is able to survive exposure to an antibiotic
Antibiotic
An antibacterial is a compound or substance that kills or slows down the growth of bacteria.The term is often used synonymously with the term antibiotic; today, however, with increased knowledge of the causative agents of various infectious diseases, antibiotic has come to denote a broader range of...
. While a spontaneous or induced genetic mutation in bacteria may confer resistance to antimicrobial drugs, gene
Gene
A gene is a molecular unit of heredity of a living organism. It is a name given to some stretches of DNA and RNA that code for a type of protein or for an RNA chain that has a function in the organism. Living beings depend on genes, as they specify all proteins and functional RNA chains...
s that confer resistance can be transferred between bacteria in a horizontal
Horizontal gene transfer
Horizontal gene transfer , also lateral gene transfer , is any process in which an organism incorporates genetic material from another organism without being the offspring of that organism...
fashion by conjugation
Bacterial conjugation
Bacterial conjugation is the transfer of genetic material between bacterial cells by direct cell-to-cell contact or by a bridge-like connection between two cells...
, transduction
Transduction (genetics)
Transduction is the process by which DNA is transferred from one bacterium to another by a virus. It also refers to the process whereby foreign DNA is introduced into another cell via a viral vector. Transduction does not require cell-to-cell contact , and it is DNAase resistant...
, or transformation
Transformation (genetics)
In molecular biology transformation is the genetic alteration of a cell resulting from the direct uptake, incorporation and expression of exogenous genetic material from its surroundings and taken up through the cell membrane. Transformation occurs naturally in some species of bacteria, but it can...
. Thus a gene for antibiotic resistance which had evolved via natural selection
Natural selection
Natural selection is the nonrandom process by which biologic traits become either more or less common in a population as a function of differential reproduction of their bearers. It is a key mechanism of evolution....
may be shared. Evolutionary stress such as exposure to antibiotics then selects for the antibiotic resistant trait. Many antibiotic resistance genes reside on plasmids, facilitating their transfer. If a bacterium carries several resistance genes, it is called multidrug resistant (MDR) or, informally, a superbug or super bacterium.
Genes for resistance to antibiotics, like the antibiotics themselves, are ancient. However, the increasing prevalence of antibiotic-resistant bacterial infections seen in clinical practice stems from antibiotic use both within human medicine and veterinary medicine. Any use of antibiotics can increase selective pressure in a population of bacteria to allow the resistant bacteria to thrive and the susceptible bacteria to die off. As resistance towards antibiotics becomes more common, a greater need for alternative treatments arises. However, despite a push for new antibiotic therapies there has been a continued decline in the number of newly approved drugs. Antibiotic resistance therefore poses a significant problem.
Causes
The widespread use of antibiotics both inside and outside of medicine is playing a significant role in the emergence of resistant bacteria. Although there were low levels of preexisting antibiotic-resistant bacteria before the widespread use of antibiotics, evolutionary pressure from their use has played a role in the development of muiltidrug resistance varieties and the spread of resistance between bacterial species. Antibiotics are often used in rearing animals for food, and this use, among others, leads to the creation of resistant strains of bacteria. In some countries, antibiotics are sold over the counter without a prescription, which also leads to the creation of resistant strains. In human medicine, the major problem of the emergence of resistant bacteria is due to misuse and overuse of antibiotics by doctors as well as patients. Other practices contributing towards resistance include the addition of antibiotics to livestock feed. Household use of antibacterials in soaps and other products, although not clearly contributing to resistance, is also discouraged (as not being effective at infection control). Also unsound practices in the pharmaceutical manufacturing industry can contribute towards the likelihood of creating antibiotic-resistant strains.Certain antibiotic classes are highly associated with colonisation with superbugs compared to other antibiotic classes. The risk for colonisation increases if there is a lack of sensitivity (resistance) of the superbugs to the antibiotic used and high tissue penetration, as well as broad-spectrum activity against "good bacteria". In the case of MRSA
Methicillin-resistant Staphylococcus aureus
Methicillin-resistant Staphylococcus aureus is a bacterium responsible for several difficult-to-treat infections in humans. It is also called multidrug-resistant Staphylococcus aureus and oxacillin-resistant Staphylococcus aureus...
, increased rates of MRSA infections are seen with glycopeptides, cephalosporin
Cephalosporin
The cephalosporins are a class of β-lactam antibiotics originally derived from Acremonium, which was previously known as "Cephalosporium".Together with cephamycins they constitute a subgroup of β-lactam antibiotics called cephems.-Medical use:...
s and especially quinolones. In the case of colonisation with Clostridium difficile
Clostridium difficile
Clostridium difficile , also known as "CDF/cdf", or "C...
the high risk antibiotics include cephalosporins and in particular quinolones and clindamycin
Clindamycin
Clindamycin rINN is a lincosamide antibiotic. It is usually used to treat infections with anaerobic bacteria but can also be used to treat some protozoal diseases, such as malaria...
.
In a paper published in the recent edition of the journal Nature, researchers at McMaster University say they have discovered that antibiotic-resistant genes existed in soil bacteria at the same time that now-extinct mammoths, early horses and bison roamed Canada's North.
In medicine
The volume of antibiotic prescribed is the major factor in increasing rates of bacterial resistance rather than compliance with antibiotics. A single dose of antibiotics leads to a greater risk of resistant organisms to that antibiotic in the person for up to a year.Inappropriate prescribing of antibiotics has been attributed to a number of causes, including: people who insist on antibiotics, physicians simply prescribe them as they feel they do not have time to explain why they are not necessary, physicians who do not know when to prescribe antibiotics or else are overly cautious for medical legal reasons. For example, a third of people believe that antibiotics are effective for the common cold
Common cold
The common cold is a viral infectious disease of the upper respiratory system, caused primarily by rhinoviruses and coronaviruses. Common symptoms include a cough, sore throat, runny nose, and fever...
and 22% of people do not finish a course of antibiotics primarily because they feel better (varying from 10% to 44%, depending on the country). Compliance with once-daily antibiotics is better than with twice-daily antibiotics. Suboptimum antibiotic concentrations in critically ill people increase the frequency of antibiotic resistance organisms. While taking antibiotics doses less than those recommended may increase rates of resistance, shortening the course of antibiotics may actually decrease rates of resistance.
Poor hand hygiene by hospital staff has been associated with the spread of resistant organisms and an increase in hand washing compliance results in decreased rates of these organisms.
Role of other animals
Drugs are used in animals that are used as human food, such as cattle, pigs, chickens, fish, etc., and these drugs can affect the safety of the meat, milk, and eggs produced from those animals and can be the source of superbugs. For example, farm animals, particularly pigs, are believed to be able to infect people with MRSA. The resistant bacteria in animals due to antibiotic exposure can be transmitted to humans via three pathways, those being through the consumption of meat, from close or direct contact with animals, or through the environment.The World Health Organization concluded antibiotics as growth promoters in animal feeds should be prohibited in the absence of risk assessments. In 1998, European Union health ministers voted to ban four antibiotics widely used to promote animal growth (despite their scientific panel's recommendations). Regulation banning the use of antibiotics in European feed, with the exception of two antibiotics in poultry feeds, became effective in 2006. In Scandinavia, there is evidence that the ban has led to a lower prevalence of antimicrobial resistance in (nonhazardous) animal bacterial populations. In the USA, federal agencies do not collect data on antibiotic use in animals, but animal-to-human spread of drug-resistant organisms has been demonstrated in research studies. Antibiotics are still used in U.S. animal feed, along with other ingredients which have safety concerns.
Growing U.S. consumer concern about using antibiotics in animal feed has led to a niche market of "antibiotic-free" animal products, but this small market is unlikely to change entrenched, industry-wide practices.
In 2001, the Union of Concerned Scientists estimated that greater than 70% of the antibiotics used in the US are given to food animals (for example, chickens, pigs and cattle) in the absence of disease. In 2000, the US Food and Drug Administration (FDA) announced their intention to revoke approval of fluoroquinolone use in poultry production because of substantial evidence linking it to the emergence of fluoroquinolone-resistant Campylobacter
Campylobacter
Campylobacter is a genus of bacteria that are Gram-negative, spiral, and microaerophilic. Motile, with either unipolar or bipolar flagella, the organisms have a characteristic spiral/corkscrew appearance and are oxidase-positive. Campylobacter jejuni is now recognized as one of the main causes...
infections in humans. The final decision to ban fluoroquinolones from use in poultry production was not made until five years later because of challenges from the food animal and pharmaceutical industries. During 2007, two federal bills (S. 549 and H.R. 962) aim at phasing out "nontherapeutic" antibiotics in US food animal production.
Mechanisms
Horizontal gene transfer
Horizontal gene transfer , also lateral gene transfer , is any process in which an organism incorporates genetic material from another organism without being the offspring of that organism...
, and also of unlinked point mutations in the pathogen
Pathogen
A pathogen gignomai "I give birth to") or infectious agent — colloquially, a germ — is a microbe or microorganism such as a virus, bacterium, prion, or fungus that causes disease in its animal or plant host...
genome
Genome
In modern molecular biology and genetics, the genome is the entirety of an organism's hereditary information. It is encoded either in DNA or, for many types of virus, in RNA. The genome includes both the genes and the non-coding sequences of the DNA/RNA....
at a rate of about 1 in 108 per chromosomal replication. The antibiotic action against the pathogen can be seen as an environmental pressure; those bacteria which have a mutation allowing them to survive will live on to reproduce. They will then pass this trait to their offspring, which will result in the evolution of a fully resistant colony.
The four main mechanisms by which microorganisms exhibit resistance to antimicrobials are:
- Drug inactivation or modification: for example, enzymatic deactivation of penicillin GPenicillinPenicillin is a group of antibiotics derived from Penicillium fungi. They include penicillin G, procaine penicillin, benzathine penicillin, and penicillin V....
in some penicillin-resistant bacteria through the production of β-lactamases - Alteration of target site: for example, alteration of PBP—the binding target site of penicillins—in MRSA and other penicillin-resistant bacteria
- Alteration of metabolic pathway: for example, some sulfonamide-resistant bacteria do not require para-aminobenzoic acid (PABA), an important precursor for the synthesis of folic acidFolic acidFolic acid and folate , as well as pteroyl-L-glutamic acid, pteroyl-L-glutamate, and pteroylmonoglutamic acid are forms of the water-soluble vitamin B9...
and nucleic acids in bacteria inhibited by sulfonamides, instead, like mammalian cells, they turn to using preformed folic acid. - Reduced drug accumulation: by decreasing drug permeabilitySemipermeable membraneA semipermeable membrane, also termed a selectively permeable membrane, a partially permeable membrane or a differentially permeable membrane, is a membrane that will allow certain molecules or ions to pass through it by diffusion and occasionally specialized "facilitated diffusion".The rate of...
and/or increasing active efflux (pumping out) of the drugs across the cell surface
There are three known mechanisms of fluoroquinolone resistance. Some types of efflux
Efflux (microbiology)
Active efflux is a mechanism responsible for extrusion of toxic substances and antibiotics outside the cell; this is considered to be a vital part of xenobiotic metabolism...
pumps can act to decrease intracellular quinolone
Quinolone
The quinolones are a family of synthetic broad-spectrum antibiotics. The term quinolone refers to potent synthetic chemotherapeutic antibacterials....
concentration. In Gram-negative bacteria, plasmid-mediated resistance genes produce proteins that can bind to DNA gyrase
DNA gyrase
DNA gyrase, often referred to simply as gyrase, is an enzyme that relieves strain while double-stranded DNA is being unwound by helicase. This causes negative supercoiling of the DNA...
, protecting it from the action of quinolones. Finally, mutations at key sites in DNA gyrase or topoisomerase IV
Topoisomerase IV
Topoisomerase IV is one of two type-II topoisomerases in bacteria, the other being DNA gyrase. Like gyrase, topoisomerase IV is able to pass one double-strand of DNA through another double-strand of DNA, thereby changing the linking number of DNA by two in each enzymatic...
can decrease their binding affinity to quinolones, decreasing the drug's effectiveness. Research has shown the bacterial protein LexA
Lexa
Lexa:* Lexa Pierce* Repressor lexA - Place name :* Lexa, Arkansas, a city in Phillips County, United StatesLexa means aborigional or native according to the dictionary.- Family name :* the House of Lexa , Lexa von Aehrenthal:...
may play a key role in the acquisition of bacterial mutations giving resistance to quinolones and rifampicin.
Antibiotic resistance can also be introduced artificially into a microorganism through laboratory protocols, sometimes used as a selectable marker
Selectable marker
A selectable marker is a gene introduced into a cell, especially a bacterium or to cells in culture, that confers a trait suitable for artificial selection. They are a type of reporter gene used in laboratory microbiology, molecular biology, and genetic engineering to indicate the success of a...
to examine the mechanisms of gene transfer or to identify individuals that absorbed a piece of DNA that included the resistance gene and another gene of interest. A recent study demonstrated the extent of horizontal gene transfer
Horizontal gene transfer
Horizontal gene transfer , also lateral gene transfer , is any process in which an organism incorporates genetic material from another organism without being the offspring of that organism...
among Staphylococcus to be much greater than one previously expected, and encompasses genes with functions beyond antibiotic resistance and virulence, and beyond genes residing within the mobile genetic elements
Mobile genetic elements
Mobile genetic elements are a type of DNA that can move around within the genome. They include:*Transposons **Retrotransposons**DNA transposons**Insertion sequences*Plasmids...
.
Staphylococcus aureus
Staphylococcus aureusStaphylococcus aureus
Staphylococcus aureus is a facultative anaerobic Gram-positive coccal bacterium. It is frequently found as part of the normal skin flora on the skin and nasal passages. It is estimated that 20% of the human population are long-term carriers of S. aureus. S. aureus is the most common species of...
(colloquially known as "Staph aureus" or a "Staph infection") is one of the major resistant pathogens. Found on the mucous membranes and the human skin
Human skin
The human skin is the outer covering of the body. In humans, it is the largest organ of the integumentary system. The skin has multiple layers of ectodermal tissue and guards the underlying muscles, bones, ligaments and internal organs. Human skin is similar to that of most other mammals,...
of around a third of the population, it is extremely adaptable to antibiotic pressure. It was one of the earlier bacteria in which penicillin
Penicillin
Penicillin is a group of antibiotics derived from Penicillium fungi. They include penicillin G, procaine penicillin, benzathine penicillin, and penicillin V....
resistance was found—in 1947, just four years after the drug started being mass-produced. Methicillin
Methicillin
Meticillin or methicillin is a narrow-spectrum beta-lactam antibiotic of the penicillin class. It should not be confused with the antibiotic metacycline.-History:Methicillin was developed by Beecham in 1959...
was then the antibiotic of choice, but has since been replaced by oxacillin
Oxacillin
Oxacillin sodium is a narrow spectrum beta-lactam antibiotic of the penicillin class.It was developed by Beecham.-Uses:...
due to significant kidney toxicity. Methicillin-resistant Staphylococcus aureus
Methicillin-resistant Staphylococcus aureus
Methicillin-resistant Staphylococcus aureus is a bacterium responsible for several difficult-to-treat infections in humans. It is also called multidrug-resistant Staphylococcus aureus and oxacillin-resistant Staphylococcus aureus...
(MRSA) was first detected in Britain in 1961, and is now "quite common" in hospitals. MRSA was responsible for 37% of fatal cases of sepsis
Sepsis
Sepsis is a potentially deadly medical condition that is characterized by a whole-body inflammatory state and the presence of a known or suspected infection. The body may develop this inflammatory response by the immune system to microbes in the blood, urine, lungs, skin, or other tissues...
in the UK
United Kingdom
The United Kingdom of Great Britain and Northern IrelandIn the United Kingdom and Dependencies, other languages have been officially recognised as legitimate autochthonous languages under the European Charter for Regional or Minority Languages...
in 1999, up from 4% in 1991. Half of all S. aureus infections in the US
United States
The United States of America is a federal constitutional republic comprising fifty states and a federal district...
are resistant to penicillin, methicillin, tetracycline and erythromycin
Erythromycin
Erythromycin is a macrolide antibiotic that has an antimicrobial spectrum similar to or slightly wider than that of penicillin, and is often used for people who have an allergy to penicillins. For respiratory tract infections, it has better coverage of atypical organisms, including mycoplasma and...
.
This left vancomycin
Vancomycin
Vancomycin INN is a glycopeptide antibiotic used in the prophylaxis and treatment of infections caused by Gram-positive bacteria. It has traditionally been reserved as a drug of "last resort", used only after treatment with other antibiotics had failed, although the emergence of...
as the only effective agent available at the time. However, strains with intermediate (4-8 μg/ml) levels of resistance, termed glycopeptide-intermediate Staphylococcus aureus (GISA) or vancomycin-intermediate Staphylococcus aureus (VISA), began appearing in the late 1990s. The first identified case was in Japan in 1996, and strains have since been found in hospitals in England, France and the US. The first documented strain with complete (>16 μg/ml) resistance to vancomycin, termed vancomycin-resistant Staphylococcus aureus
Vancomycin-resistant Staphylococcus aureus
Vancomycin-resistant Staphylococcus aureus refers to strains of Staphylococcus aureus that have become resistant to the glycopeptide antibiotic vancomycin. With the increase of staphylococcal resistance to methicillin, vancomycin is often a treatment of choice in infections with...
(VRSA) appeared in the United States in 2002.
A new class of antibiotics, oxazolidinones
Linezolid
Linezolid is a synthetic antibiotic used for the treatment of serious infections caused by Gram-positive bacteria that are resistant to several other antibiotics...
, became available in the 1990s, and the first commercially available oxazolidinone, linezolid
Linezolid
Linezolid is a synthetic antibiotic used for the treatment of serious infections caused by Gram-positive bacteria that are resistant to several other antibiotics...
, is comparable to vancomycin in effectiveness against MRSA. Linezolid-resistance in S. aureus was reported in 2003.
Community-acquired MRSA (CA-MRSA)has now emerged as an epidemic that is responsible for rapidly progressive, fatal diseases, including necrotizing pneumonia, severe sepsis
Sepsis
Sepsis is a potentially deadly medical condition that is characterized by a whole-body inflammatory state and the presence of a known or suspected infection. The body may develop this inflammatory response by the immune system to microbes in the blood, urine, lungs, skin, or other tissues...
and necrotizing fasciitis
Necrotizing fasciitis
Necrotizing fasciitis , commonly known as flesh-eating disease or Flesh-eating bacteria syndrome, is a rare infection of the deeper layers of skin and subcutaneous tissues, easily spreading across the fascial plane within the subcutaneous tissue.Necrotizing fasciitis is a quickly progressing and...
. MRSA is the most frequently identified antimicrobial drug-resistant pathogen in US hospitals. The epidemiology
Epidemiology
Epidemiology is the study of health-event, health-characteristic, or health-determinant patterns in a population. It is the cornerstone method of public health research, and helps inform policy decisions and evidence-based medicine by identifying risk factors for disease and targets for preventive...
of infections caused by MRSA is rapidly changing. In the past 10 years, infections caused by this organism have emerged in the community. The two MRSA clones in the United States most closely associated with community outbreaks, USA400 (MW2 strain, ST1 lineage) and USA300, often contain Panton-Valentine leukocidin
Panton-Valentine leukocidin
Panton-Valentine leukocidin is a cytotoxin—one of the β-pore-forming toxins. The presence of PVL is associated with increased virulence of certain strains of Staphylococcus aureus...
(PVL) genes and, more frequently, have been associated with skin and soft tissue infections. Outbreaks of CA-MRSA infections have been reported in correctional facilities, among athletic teams, among military recruits, in newborn nurseries, and among men who have sex with men. CA-MRSA infections now appear to be endemic in many urban regions and cause most CA-S. aureus infections.
Streptococcus and Enterococcus
Streptococcus pyogenesStreptococcus pyogenes
Streptococcus pyogenes is a spherical, Gram-positive bacterium that is the cause of group A streptococcal infections. S. pyogenes displays streptococcal group A antigen on its cell wall. S...
(Group A Streptococcus: GAS) infections can usually be treated with many different antibiotics. Early treatment may reduce the risk of death from invasive group A streptococcal disease. However, even the best medical care does not prevent death in every case. For those with very severe illness, supportive care in an intensive care unit may be needed. For persons with necrotizing fasciitis, surgery often is needed to remove damaged tissue. Strains of S. pyogenes resistant to macrolide
Macrolide
The macrolides are a group of drugs whose activity stems from the presence of a macrolide ring, a large macrocyclic lactone ring to which one or more deoxy sugars, usually cladinose and desosamine, may be attached. The lactone rings are usually 14-, 15-, or 16-membered...
antibiotics have emerged; however, all strains remain uniformly sensitive to penicillin
Penicillin
Penicillin is a group of antibiotics derived from Penicillium fungi. They include penicillin G, procaine penicillin, benzathine penicillin, and penicillin V....
.
Resistance of Streptococcus pneumoniae
Streptococcus pneumoniae
Streptococcus pneumoniae, or pneumococcus, is Gram-positive, alpha-hemolytic, aerotolerant anaerobic member of the genus Streptococcus. A significant human pathogenic bacterium, S...
to penicillin and other beta-lactams is increasing worldwide. The major mechanism of resistance involves the introduction of mutations in genes encoding penicillin-binding proteins. Selective pressure is thought to play an important role, and use of beta-lactam antibiotics has been implicated as a risk factor for infection and colonization. S. pneumoniae is responsible for pneumonia
Pneumonia
Pneumonia is an inflammatory condition of the lung—especially affecting the microscopic air sacs —associated with fever, chest symptoms, and a lack of air space on a chest X-ray. Pneumonia is typically caused by an infection but there are a number of other causes...
, bacteremia
Bacteremia
Bacteremia is the presence of bacteria in the blood. The blood is normally a sterile environment, so the detection of bacteria in the blood is always abnormal....
, otitis media
Otitis media
Otitis media is inflammation of the middle ear, or a middle ear infection.It occurs in the area between the tympanic membrane and the inner ear, including a duct known as the eustachian tube. It is one of the two categories of ear inflammation that can underlie what is commonly called an earache,...
, meningitis
Meningitis
Meningitis is inflammation of the protective membranes covering the brain and spinal cord, known collectively as the meninges. The inflammation may be caused by infection with viruses, bacteria, or other microorganisms, and less commonly by certain drugs...
, sinusitis
Sinusitis
Sinusitis is inflammation of the paranasal sinuses, which may be due to infection, allergy, or autoimmune issues. Most cases are due to a viral infection and resolve over the course of 10 days...
, peritonitis
Peritonitis
Peritonitis is an inflammation of the peritoneum, the serous membrane that lines part of the abdominal cavity and viscera. Peritonitis may be localised or generalised, and may result from infection or from a non-infectious process.-Abdominal pain and tenderness:The main manifestations of...
and arthritis
Arthritis
Arthritis is a form of joint disorder that involves inflammation of one or more joints....
.
Multidrug-resistant Enterococcus faecalis
Enterococcus faecalis
Enterococcus faecalis – formerly classified as part of the Group D Streptococcus system – is a Gram-positive, commensal bacterium inhabiting the gastrointestinal tracts of humans and other mammals. It is among the main constituents of some probiotic food supplements. Like other species in the genus...
and Enterococcus faecium
Enterococcus faecium
Enterococcus faecium is a Gram-positive, alpha hemolytic or nonhemolytic bacterium in the genus Enterococcus. It can be commensal in the human intestine, but it may also be pathogenic, causing diseases such as neonatal meningitis.Vancomycin-resistant E. faecium is often referred to as VRE.Some...
are associated with nosocomial infections
Nosocomial infection
A nosocomial infection , also known as a hospital-acquired infection or HAI, is an infection whose development is favoured by a hospital environment, such as one acquired by a patient during a hospital visit or one developing among hospital staff...
. Among these strains, penicillin
Penicillin
Penicillin is a group of antibiotics derived from Penicillium fungi. They include penicillin G, procaine penicillin, benzathine penicillin, and penicillin V....
-resistant Enterococcus
Enterococcus
Enterococcus is a genus of lactic acid bacteria of the phylum Firmicutes. Enterococci are Gram-positive cocci that often occur in pairs or short chains, and are difficult to distinguish from streptococci on physical characteristics alone. Two species are common commensal organisms in the...
was seen in 1983, vancomycin-resistant Enterococcus
Vancomycin-Resistant Enterococcus
Vancomycin-resistant Enterococcus, or vancomycin-resistant enterococci , are bacterial strains of the genus Enterococcus that are resistant to the antibiotic vancomycin. To become VRE, vancomycin-sensitive enterococci typically obtain new DNA in the form of plasmids or transposons which encode...
in 1987, and linezolid
Linezolid
Linezolid is a synthetic antibiotic used for the treatment of serious infections caused by Gram-positive bacteria that are resistant to several other antibiotics...
-resistant Enterococcus
Enterococcus
Enterococcus is a genus of lactic acid bacteria of the phylum Firmicutes. Enterococci are Gram-positive cocci that often occur in pairs or short chains, and are difficult to distinguish from streptococci on physical characteristics alone. Two species are common commensal organisms in the...
in the late 1990s.
Pseudomonas aeruginosa
Pseudomonas aeruginosaPseudomonas aeruginosa
Pseudomonas aeruginosa is a common bacterium that can cause disease in animals, including humans. It is found in soil, water, skin flora, and most man-made environments throughout the world. It thrives not only in normal atmospheres, but also in hypoxic atmospheres, and has, thus, colonized many...
is a highly prevalent opportunistic pathogen. One of the most worrisome characteristics of P. aeruginosa is its low antibiotic susceptibility, which is is attributable to a concerted action of multidrug efflux pumps
Efflux (microbiology)
Active efflux is a mechanism responsible for extrusion of toxic substances and antibiotics outside the cell; this is considered to be a vital part of xenobiotic metabolism...
with chromosomally encoded antibiotic resistance genes (for example, mexAB-oprM, mexXY, etc.) and the low permeability of the bacterial cellular envelopes. Besides intrinsic resistance, P. aeruginosa easily evolves specific resistance either by mutation
Mutation
In molecular biology and genetics, mutations are changes in a genomic sequence: the DNA sequence of a cell's genome or the DNA or RNA sequence of a virus. They can be defined as sudden and spontaneous changes in the cell. Mutations are caused by radiation, viruses, transposons and mutagenic...
in chromosomally-encoded genes, or by the horizontal gene transfer of antibiotic resistance determinants. Evolution of multidrug resistance
Multidrug resistance
Multiple drug resistance or Multidrug resistance is a condition enabling a disease-causing organism to resist distinct drugs or chemicals of a wide variety of structure and function targeted at eradicating the organism...
by P. aeruginosa isolates requires several genetic events that include acquisition of different mutations and/or horizontal transfer of antibiotic resistance genes. Hypermutation favours the selection of mutation-driven antibiotic resistance in P. aeruginosa strains, producing chronic infections, whereas the clustering of several different antibiotic resistance genes in integron
Integron
An integron is a two component gene capture and dissemination system, initially discovered in relation to antibiotic resistance, and which is found in plasmids, chromosomes and transposons...
s favours the concerted acquisition of antibiotic resistance determinants. Some recent studies have shown phenotypic resistance associated with biofilm
Biofilm
A biofilm is an aggregate of microorganisms in which cells adhere to each other on a surface. These adherent cells are frequently embedded within a self-produced matrix of extracellular polymeric substance...
formation or the emergence of small-colony-variants may be important in the response of P. aeruginosa populations to antibiotic
Antibiotic
An antibacterial is a compound or substance that kills or slows down the growth of bacteria.The term is often used synonymously with the term antibiotic; today, however, with increased knowledge of the causative agents of various infectious diseases, antibiotic has come to denote a broader range of...
s treatment.
Clostridium difficile
Clostridium difficileClostridium difficile
Clostridium difficile , also known as "CDF/cdf", or "C...
is a nosocomial pathogen that causes diarrheal disease in hospitals world wide. Clindamycin
Clindamycin
Clindamycin rINN is a lincosamide antibiotic. It is usually used to treat infections with anaerobic bacteria but can also be used to treat some protozoal diseases, such as malaria...
-resistant C. difficile was reported as the causative agent of large outbreaks of diarrheal disease in hospitals in New York, Arizona, Florida and Massachusetts between 1989 and 1992. Geographically dispersed outbreaks of C. difficile strains resistant to fluoroquinolone antibiotics, such as ciprofloxacin and levofloxacin, were also reported in North America in 2005.
Salmonella and E. coli
Escherichia coliEscherichia coli
Escherichia coli is a Gram-negative, rod-shaped bacterium that is commonly found in the lower intestine of warm-blooded organisms . Most E. coli strains are harmless, but some serotypes can cause serious food poisoning in humans, and are occasionally responsible for product recalls...
and Salmonella
Salmonella
Salmonella is a genus of rod-shaped, Gram-negative, non-spore-forming, predominantly motile enterobacteria with diameters around 0.7 to 1.5 µm, lengths from 2 to 5 µm, and flagella which grade in all directions . They are chemoorganotrophs, obtaining their energy from oxidation and reduction...
come directly from contaminated food. When both bacteria are spread, serious health conditions arise. Many people are hospitalized each year after becoming infected, with some dying as a result. By 1993, E. coli resistant to multiple fluoroquinolone variants was documented.
Acinetobacter baumannii
On November 5, 2004, the Centers for Disease Control and PreventionCenters for Disease Control and Prevention
The Centers for Disease Control and Prevention are a United States federal agency under the Department of Health and Human Services headquartered in Druid Hills, unincorporated DeKalb County, Georgia, in Greater Atlanta...
(CDC) reported an increasing number of Acinetobacter baumannii
Acinetobacter baumannii
Acinetobacter baumannii is a species of pathogenic bacteria, referred to as an aerobic gram-negative bacterium, that is resistant to most antibiotics. As a result of its resistance to drug treatment, some estimates state the disease is killing tens of thousands of U.S...
bloodstream infections in patients at military medical facilities in which service members injured in the Iraq
Iraq
Iraq ; officially the Republic of Iraq is a country in Western Asia spanning most of the northwestern end of the Zagros mountain range, the eastern part of the Syrian Desert and the northern part of the Arabian Desert....
/Kuwait
Kuwait
The State of Kuwait is a sovereign Arab state situated in the north-east of the Arabian Peninsula in Western Asia. It is bordered by Saudi Arabia to the south at Khafji, and Iraq to the north at Basra. It lies on the north-western shore of the Persian Gulf. The name Kuwait is derived from the...
region during Operation Iraqi Freedom and in Afghanistan
Afghanistan
Afghanistan , officially the Islamic Republic of Afghanistan, is a landlocked country located in the centre of Asia, forming South Asia, Central Asia and the Middle East. With a population of about 29 million, it has an area of , making it the 42nd most populous and 41st largest nation in the world...
during Operation Enduring Freedom were treated. Most of these showed multidrug resistance
Multidrug resistance
Multiple drug resistance or Multidrug resistance is a condition enabling a disease-causing organism to resist distinct drugs or chemicals of a wide variety of structure and function targeted at eradicating the organism...
(MRAB), with a few isolates resistant to all drugs tested.
Mycobacterium tuberculosis
Resistance of Mycobacterium tuberculosisMycobacterium tuberculosis
Mycobacterium tuberculosis is a pathogenic bacterial species in the genus Mycobacterium and the causative agent of most cases of tuberculosis . First discovered in 1882 by Robert Koch, M...
to isoniazid
Isoniazid
Isoniazid , also known as isonicotinylhydrazine , is an organic compound that is the first-line antituberculosis medication in prevention and treatment. It was first discovered in 1912, and later in 1951 it was found to be effective against tuberculosis by inhibiting its mycolic acid...
, rifampin, and other common treatments has become an increasingly relevant clinical challenge.
Prevention
Rational use of antibiotics may reduce the chances of development of opportunistic infection by antibiotic-resistant bacteria due to dysbacteriosis. In one study, the use of fluoroquinolones is clearly associated with Clostridium difficileClostridium difficile
Clostridium difficile , also known as "CDF/cdf", or "C...
infection, which is a leading cause of nosocomial diarrhea
Diarrhea
Diarrhea , also spelled diarrhoea, is the condition of having three or more loose or liquid bowel movements per day. It is a common cause of death in developing countries and the second most common cause of infant deaths worldwide. The loss of fluids through diarrhea can cause dehydration and...
in the United States, and a major cause of death, worldwide.
There is clinical evidence that topical dermatological preparations, such as those containing tea tree oil
Tea tree oil
Tea tree oil, or melaleuca oil, is a pale yellow colour to nearly clear essential oil with a fresh camphoraceous odor. It is taken from the leaves of the Melaleuca alternifolia, which is native to the northeast coast of New South Wales, Australia...
and thyme
Thyme
Thyme is a culinary and medicinal herb of the genus Thymus.-History:Ancient Egyptians used thyme for embalming. The ancient Greeks used it in their baths and burnt it as incense in their temples, believing it was a source of courage...
oil, may be effective in preventing transmittal of CA-MRSA. In addition, other phytotherapeutic
Phytotherapy
Phytotherapy is the study of the use of extracts from natural origin as medicines or health-promoting agents.Traditional phytotherapy is often used as synonym for herbalism and regarded as "alternative medicine" by much of Western medicine, although effects of many substances found in plants have...
medicines, too, can reduce the use of antibiotics or eliminate their use entirely.
Vaccine
Vaccine
A vaccine is a biological preparation that improves immunity to a particular disease. A vaccine typically contains an agent that resembles a disease-causing microorganism, and is often made from weakened or killed forms of the microbe or its toxins...
s do not suffer the problem of resistance because a vaccine enhances the body's natural defenses, while an antibiotic operates separately from the body's normal defenses. Nevertheless, new strains may evolve
Evolution
Evolution is any change across successive generations in the heritable characteristics of biological populations. Evolutionary processes give rise to diversity at every level of biological organisation, including species, individual organisms and molecules such as DNA and proteins.Life on Earth...
that escape immunity induced by vaccines; for example an update influenza vaccine is needed each year.
While theoretically promising, antistaphylococcal vaccines have shown limited efficacy, because of immunological variation between Staphylococcus species, and the limited duration of effectiveness of the antibodies produced. Development and testing of more effective vaccines is under way.
The Australian Commonwealth Scientific and Industrial Research Organization (CSIRO), realizing the need for the reduction of antibiotic use, has been working on two alternatives. One alternative is to prevent diseases by adding cytokine
Cytokine
Cytokines are small cell-signaling protein molecules that are secreted by the glial cells of the nervous system and by numerous cells of the immune system and are a category of signaling molecules used extensively in intercellular communication...
s instead of antibiotics to animal feed. These proteins are made in the animal body "naturally" after a disease and are not antibiotics, so they do not contribute to the antibiotic resistance problem. Furthermore, studies on using cytokines have shown they also enhance the growth of animals like the antibiotics now used, but without the drawbacks of nontherapeutic antibiotic use. Cytokines have the potential to achieve the animal growth rates traditionally sought by the use of antibiotics without the contribution of antibiotic resistance associated with the widespread nontherapeutic uses of antibiotics currently used in the food animal production industries. Additionally, CSIRO is working on vaccines for diseases.
Phage therapy
Phage therapyPhage therapy
Phage therapy is the therapeutic use of bacteriophages to treat pathogenic bacterial infections. Although extensively used and developed mainly in former Soviet Union countries circa 1920, this method of therapy is still being tested for treatment of a variety of bacterial and poly-microbial...
, an approach that has been extensively researched and used as a therapeutic agent for over 60 years, especially in the Soviet Union
Soviet Union
The Soviet Union , officially the Union of Soviet Socialist Republics , was a constitutionally socialist state that existed in Eurasia between 1922 and 1991....
, is an alternative that might help with the problem of resistance. Phage therapy was widely used in the United States until the discovery of antibiotics, in the early 1940s. Bacteriophages or "phages" are viruses that invade bacterial cells and, in the case of lytic phages, disrupt bacterial metabolism and cause the bacterium to lyse
Lysis
Lysis refers to the breaking down of a cell, often by viral, enzymic, or osmotic mechanisms that compromise its integrity. A fluid containing the contents of lysed cells is called a "lysate"....
. Phage therapy is the therapeutic use of lytic bacteriophages to treat pathogenic bacterial infections.
Bacteriophage therapy is an important alternative to antibiotics in the current era of multidrug resistant pathogens. A review of studies that dealt with the therapeutic use of phages from 1966–1996 and few latest ongoing phage therapy projects via internet showed: phages were used topically, orally or systemically in Polish and Soviet studies. The success rate found in these studies was 80–95% with few gastrointestinal or allergic side effects. British studies also demonstrated significant efficacy of phages against Escherichia coli
Escherichia coli
Escherichia coli is a Gram-negative, rod-shaped bacterium that is commonly found in the lower intestine of warm-blooded organisms . Most E. coli strains are harmless, but some serotypes can cause serious food poisoning in humans, and are occasionally responsible for product recalls...
, Acinetobacter
Acinetobacter
Acinetobacter [asz−in−ée−toe–back−ter] is a genus of Gram-negative bacteria belonging to the Gammaproteobacteria. Acinetobacter species are non-motile and oxidase-negative, and occur in pairs under magnification....
spp., Pseudomonas
Pseudomonas
Pseudomonas is a genus of gammaproteobacteria, belonging to the family Pseudomonadaceae containing 191 validly described species.Recently, 16S rRNA sequence analysis has redefined the taxonomy of many bacterial species. As a result, the genus Pseudomonas includes strains formerly classified in the...
spp. and Staphylococcus aureus
Staphylococcus aureus
Staphylococcus aureus is a facultative anaerobic Gram-positive coccal bacterium. It is frequently found as part of the normal skin flora on the skin and nasal passages. It is estimated that 20% of the human population are long-term carriers of S. aureus. S. aureus is the most common species of...
. US studies dealt with improving the bioavailability of phage. Phage therapy may prove as an important alternative to antibiotics for treating multidrug resistant pathogens.
New medications
Until recently, research and developmentResearch and development
The phrase research and development , according to the Organization for Economic Co-operation and Development, refers to "creative work undertaken on a systematic basis in order to increase the stock of knowledge, including knowledge of man, culture and society, and the use of this stock of...
(R&D) efforts have provided new drugs in time to treat bacteria that became resistant to older antibiotics. That is no longer the case. The potential crisis at hand is the result of a marked decrease in industry R&D, and the increasing prevalence of resistant bacteria. Infectious disease physicians are alarmed by the prospect that effective antibiotics may not be available to treat seriously ill patients in the near future.
As bacterial antibiotic resistance continues to exhaust the supply of effective antibiotics, a global public health disaster appears likely. Poor financial investment in antibiotic research has exacerbated the situation. A call to arms raised by several prestigious scientific organisations a few years ago rallied the scientific community, and now the scope of antibacterial research has broadened considerably.
The pipeline of new antibiotics is drying up. Major pharmaceutical companies are losing interest in the antibiotics market because these drugs may not be as profitable as drugs that treat chronic (long-term) conditions and lifestyle issues.
Archaeocin
Archaeocin
Archaeocin is the name given to a new type of potentially useful antibiotic that is derived from the Archaea group of organisms. Eight archaeocins have been partially or fully characterized, but hundreds of archaeocins are believed to exist, especially within the haloarchaea...
s is the name given to a new class of potentially useful antibiotics that are derived from the Archaea
Archaea
The Archaea are a group of single-celled microorganisms. A single individual or species from this domain is called an archaeon...
group of organisms. Eight archaeocins have been partially or fully characterized, but hundreds are believed to exist, especially within the haloarchaea
Archaea
The Archaea are a group of single-celled microorganisms. A single individual or species from this domain is called an archaeon...
. The prevalence of archaeocins is unknown simply because no one has looked for them. The discovery of new archaeocins hinges on recovery and cultivation of archaeal organisms from the environment. For example, samples from a novel hypersaline field site, Wilson Hot Springs, recovered 350 halophilic organisms; preliminary analysis of 75 isolates showed that 48 were archaeal and 27 were bacterial.
In research published on October 17, 2008 in Cell
Cell (journal)
Cell is a peer-reviewed scientific journal publishing research papers across a broad range of disciplines within the life sciences. Areas covered include molecular biology, cell biology, systems biology, stem cells, developmental biology, genetics and genomics, proteomics, cancer research,...
, a team of scientists pinpointed the place on bacteria where the antibiotic myxopyronin
Myxopyronin
Myxopyronin is an alpha-pyrone antibiotic, the first in a new class of inhibitors of bacterial RNA polymerase that target switch 1 and switch 2 of the RNAP "switch region." Rifamycin antibacterial agents, which are first-line treatments for tuberculosis, and lipiarmycin also target RNAP, but...
launches its attack, and why that attack is successful. The myxopyronin binds to and inhibits the crucial bacterial enzyme, RNA polymerase
RNA polymerase
RNA polymerase is an enzyme that produces RNA. In cells, RNAP is needed for constructing RNA chains from DNA genes as templates, a process called transcription. RNA polymerase enzymes are essential to life and are found in all organisms and many viruses...
. The myxopyronin changes the structure of the switch-2 segment of the enzyme, inhibiting its function of reading and transmitting DNA code. This prevents RNA polymerase from delivering genetic information to the ribosomes, causing the bacteria to die.
One of the major causes of antibiotic resistance is the decrease of effective drug concentrations at their target place, due to the increased action of ABC transporters. Since ABC transporter blockers can be used in combination with current drugs to increase their effective intracellular concentration, the possible impact of ABC transporter inhibitors is of great clinical interest. ABC transporter blockers that may be useful to increase the efficacy of current drugs have entered clinical trials and are available to be used in therapeutic regimens.
Applications
Antibiotic resistance is an important tool for genetic engineeringGenetic engineering
Genetic engineering, also called genetic modification, is the direct human manipulation of an organism's genome using modern DNA technology. It involves the introduction of foreign DNA or synthetic genes into the organism of interest...
. By constructing a plasmid
Plasmid
In microbiology and genetics, a plasmid is a DNA molecule that is separate from, and can replicate independently of, the chromosomal DNA. They are double-stranded and, in many cases, circular...
which contains an antibiotic resistance gene as well as the gene being engineered or expressed, a researcher can ensure that when bacteria replicate, only the copies which carry along the plasmid survive. This ensures that the gene being manipulated passes along when the bacteria replicates.
The most commonly used antibiotics in genetic engineering are generally "older" antibiotics which have largely fallen out of use in clinical practice. These include:
- ampicillinAmpicillinAmpicillin is a beta-lactam antibiotic that has been used extensively to treat bacterial infections since 1961. Until the introduction of ampicillin by the British company Beecham, penicillin therapies had only been effective against Gram-positive organisms such as staphylococci and streptococci...
- kanamycinKanamycinKanamycin sulfate is an aminoglycoside antibiotic, available in oral, intravenous, and intramuscular forms, and used to treat a wide variety of infections. Kanamycin is isolated from Streptomyces kanamyceticus.-Mechanism:...
- tetracycline
- chloramphenicolChloramphenicolChloramphenicol is a bacteriostatic antimicrobial that became available in 1949. It is considered a prototypical broad-spectrum antibiotic, alongside the tetracyclines, and as it is both cheap and easy to manufacture it is frequently found as a drug of choice in the third world.Chloramphenicol is...
Industrially the use of antibiotic resistance is disfavored since maintaining bacterial cultures would require feeding them large quantities of antibiotics. Instead, the use of auxotrophic bacterial strains (and function-replacement plasmids) is preferred.
See also
- Antibiotic misuseAntibiotic misuseAntibiotic misuse, sometimes called antibiotic abuse or antibiotic overuse, refers to the misuse and overuse of antibiotics, which has potentially serious effects on public health. This overuse is a contributing factor to the creation of Antibiotic resistant bacteria, or "super bugs", sometimes out...
- Antibiotic tolerance
- Drug resistanceDrug resistanceDrug resistance is the reduction in effectiveness of a drug such as an antimicrobial or an antineoplastic in curing a disease or condition. When the drug is not intended to kill or inhibit a pathogen, then the term is equivalent to dosage failure or drug tolerance. More commonly, the term is used...
- Multidrug resistanceMultidrug resistanceMultiple drug resistance or Multidrug resistance is a condition enabling a disease-causing organism to resist distinct drugs or chemicals of a wide variety of structure and function targeted at eradicating the organism...
- Multidrug toleranceMultidrug toleranceMultidrug tolerance or antibiotic tolerance is the ability of a disease-causing microorganism to resist killing by antibiotics or other antimicrobials. It is mechanistically distinct from multidrug resistance: It is not caused by mutant microbes, but rather by microbial cells that exist in a...
- New Delhi metallo-beta-lactamaseNew Delhi metallo-beta-lactamaseNew Delhi metallo-beta-lactamase-1 is an enzyme that makes bacteria resistant to a broad range of beta-lactam antibiotics. These include the antibiotics of the carbapenem family, which are a mainstay for the treatment of antibiotic-resistant bacterial infections...
(NDM-1) antibacterial resistance gene. - Beta-lactamase#KPC (K. pneumoniae carbapenemase) (Class A) (KPC) antibacterial resistance gene
- Antibacterial soapAntibacterial soapAntibacterial soap is any cleaning product to which active antibacterial ingredients have been added. These chemicals kill bacteria and microbes, but are no more effective at deactivating viruses than any other kind of soap or detergent, and they also kill nonpathogenic bacteria.-Ingredients:Most...
- Bacterial conjugationBacterial conjugationBacterial conjugation is the transfer of genetic material between bacterial cells by direct cell-to-cell contact or by a bridge-like connection between two cells...
- Drug of last resortDrug of last resortDrugs of last resort are drugs only used when all other options are exhausted. Many of the best known are antibiotics, antivirals, or chemotherapy agents. In those cases, they have the most potent antibiotic, antiviral, or anticancer effects, and/or are drugs for which no resistant strains are...
- Efflux
- Nosocomial infectionNosocomial infectionA nosocomial infection , also known as a hospital-acquired infection or HAI, is an infection whose development is favoured by a hospital environment, such as one acquired by a patient during a hospital visit or one developing among hospital staff...
- Pesticide resistancePesticide resistancePesticide resistance is the adaptation of pest population targeted by a pesticide resulting in decreased susceptibility to that chemical. In other words, pests develop a resistance to a chemical through natural selection: the most resistant organisms are the ones to survive and pass on their...
- LexARepressor lexARepressor LexA or LexA is a repressor enzyme that represses SOS response genes coding for DNA polymerases required for repairing DNA damage. LexA is intimately linked to RecA in the biochemical cycle of DNA damage and repair. RecA binds to DNA-bound LexA causing LexA to cleave itself in a...
- TuberculosisTuberculosisTuberculosis, MTB, or TB is a common, and in many cases lethal, infectious disease caused by various strains of mycobacteria, usually Mycobacterium tuberculosis. Tuberculosis usually attacks the lungs but can also affect other parts of the body...
- List of environment topics
- Broad-spectrum antibioticBroad-spectrum antibioticThe term broad-spectrum antibiotic refers to an antibiotic that acts against a wide range of disease-causing bacteria. A broad-spectrum antibiotic acts against both Gram-positive and Gram-negative bacteria, in contrast to a narrow-spectrum antibiotic, which is effective against specific families of...
- Center for Disease Dynamics, Economics & PolicyCenter for Disease Dynamics, Economics & PolicyThe Center for Disease Dynamics, Economics & Policy is a public health research organization with headquarters in Washington, D.C. and New Delhi...
External links
- WHO fact sheet
- CDC Article on Hospital Acquired MRSA
- CDC Article on Community Acquired MRSA
- CDC Guideline "Management of Multidrug-Resistant Organisms in Healthcare Settings, 2006"
- ReAct Action on Antibiotic Resistance
- Alliance for the Prudent Use of Antibiotics
- Prudent Use of Antibiotics
- Information about phage therapy – a possible alternative to antibiotics in case of resistant infections
- Antibiotic-resistance genes as markers Once necessary, now undesirable
- CBS Article on Phage Therapy and Antibiotic Resistance
- Hospitals: Breeding the Superbug? Article on MRSA infections in hospitals, Allianz Knowledge, May 2008
- BURDEN of Resistance and Disease in European Nations - An EU-Project to estimate the financial burden of antibiotic resistance in European Hospitals
- Extending the Cure: Policy Research to Extend Antibiotic Effectiveness
- 2003 New Guidance for Industry on Antimicrobial Drugs for Food Animals Questions and Answers, U.S. FDA
- SciDev.net Antibiotic Resistance spotlight The Science and Development Network is an online science and development network focused on news and information important to the developing world
- Do Bugs Need Drugs?
- Uppsala university, Resistance to antibiotics – global threat
- Combating Drug Resistance - Tackling drug resistance in bacteria and other pathogens.

