Breast cancer screening
Encyclopedia
Breast cancer screening refers to the medical screening of asymptomatic
, apparently healthy women for breast cancer
in an attempt to achieve an earlier diagnosis. The assumption is that early detection will improve outcomes. A number of screening test have been employed including: clinical and self breast exams, mammography, genetic screening, ultrasound, and magnetic resonance imaging.
A clinical or self breast exam involves feeling the breast for lumps
or other abnormalities. Evidence however does not support its use in women with a typical risk for breast cancer. The use of mammography
in universal screening for breast cancer is also controversial. The Cochrane collaboration
in 2009 concluded that it is unclear whether screening does more good than harm. Many national organizations still recommend it for most older women. If screening mammography (as opposed to diagnostic mammography) is chosen for women at normal risk for breast cancer, it should only be done every two years in women between the ages of 50 and 74. Several tools are available to help target breast cancer screening to older women with longer life expectancies. Similar imaging studies can be performed with magnetic resonance imaging
.
Earlier, more aggressive, and more frequent screening is recommended for women at particularly high risk of developing breast cancer, such as those with a confirmed BRCA mutation
, those who have previously had breast cancer, and those with a strong family history of breast and ovarian cancer.
Abnormal findings on screening are further investigated by surgically removing a piece of the suspicious lumps (biopsy
) to examine them under the microscope. Ultrasound
may be used to guide the biopsy needle during the procedure. Magnetic resonance imaging
is used to guide treatment, but is not an established screening method for healthy women.
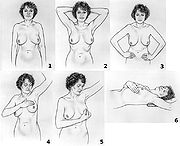 Breast examination (either clinical breast exams (CBE) by a health care provider or by self exams) were once widely recommended. They however are not supported by evidence and may, like mammography and other screening methods that produce false positive results, contribute to harm. The use of screening in women without symptoms and at low risk is thus controversial.
Breast examination (either clinical breast exams (CBE) by a health care provider or by self exams) were once widely recommended. They however are not supported by evidence and may, like mammography and other screening methods that produce false positive results, contribute to harm. The use of screening in women without symptoms and at low risk is thus controversial.
A 2003 Cochrane review found screening by breast self-examination or by clinical exam is not associated with death rates among women who report performing breast self-examination and does, like other breast cancer screening methods, increase harms, in terms of increased numbers of benign lesions identified and an increased number of biopsies performed. They conclude "screening by breast self-examination or physical examination cannot be recommended."
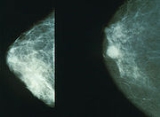
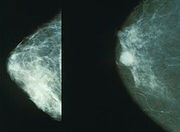
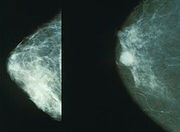
is a common screening method, since it is relatively fast and widely available in developed countries. Mammography is a type of radiography
used on the breasts. Mammography is not useful in finding breast tumors in dense breast tissue characteristic of women under 40 years. It is typically used for two purposes: to aid in the diagnosis of a woman who is experiencing symptoms (called diagnostic mammography), and for medical screening of apparently healthy women (called screening mammography). In women over 50 without dense breasts, breast cancers detected by screening mammography are usually smaller and less aggressive than those detected by patients or doctors as a breast lump. This is because the most aggressive breast cancers are found in dense breast tissue which mammograms can not image.
The presumption is that by detecting the cancer in an earlier stage, women will be more likely to be cured by treatment. This assertion however has been challenged by recent reviews which have found the significance of these benefits to be questionable.
 Screening mammography is usually recommended to women who are most likely to develop breast cancer. In general, this means women with a personal or family history of breast cancer, and most older women, but not frail elderly
Screening mammography is usually recommended to women who are most likely to develop breast cancer. In general, this means women with a personal or family history of breast cancer, and most older women, but not frail elderly
women, who are unlikely to benefit from treatment.
Women who agree to be screened have their breasts X-rayed on a specialized X-ray machine. This exposes the woman's breasts to a small amount of ionizing radiation
, which has a very small, but non-zero, chance of causing cancer.
The X-ray image, called a radiograph, is sent to a physician who specializes in interpreting these images, called a radiologist. The image may be on plain photographic film
or digital mammography
on a computer screen; despite the much higher cost of the digital systems, the two methods are generally considered equally effective. The equipment may use a computer-aided diagnosis
(CAD) system.
There is considerable variation in interpreting the images; the same image may be declared normal by one radiologist and suspicious by another. It can be helpful to compare the images to any previously taken images, as changes over time may be significant.
If a suspicious signs are identified in the image, then the woman is usually recalled for a second mammogram, sometimes after waiting six months to see whether the spot is growing, or a biopsy
of the breast. Most of these will prove to be false positives, resulting in sometimes debilitating anxiety
over nothing. Most women recalled will undergo additional imaging only, without any further intervention. Recall rates are higher in the U.S. than in the UK.
A 2009 Cochrane review estimated that mammography in women between 50 and 75 years old results in a relative risk reduction
of death from breast cancer of 15% or an absolute risk reduction
of 0.05%. Those who have mammograms however end up with increased surgeries, chemotherapy, radiotherapy and other potentially procedures resulting from the over-detection of harmless lumps. Many women will experience important psychological distress for many months because of false positive findings. Consequently, the value of routine mammography in women at low or average risk is controversial. With unnecessary treatment of ten women for every one woman whose life was prolonged, the authors concluded that routine mammography may do more harm than good.
If 1,000 women in their 50s are screened every year for ten years, the following outcomes are considered typical in the developed world:
The outcomes are worse for women in their 20s, 30s, and 40s, as they are far less likely to have a life-threatening breast cancer, and more likely to have dense breasts that make interpreting the mammogram more difficult. Among women in their 60s, who have a somewhat higher rate of breast cancer, the proportion of positive outcomes to harms are better:
Mammography is not generally considered as an effective screening technique for women at average or low risk of developing cancer who are less than 50 years old. For normal-risk women 40 to 49 years of age, the risks of mammography outweigh the benefits, and the US Preventive Services Task Force says that the evidence in favor of routine screening of women under the age of 50 is "weak". Part of the difficulty in interpreting mammograms in younger women stems from breast density. Radiographically, a dense breast has a preponderance of glandular tissue, and younger age or estrogen
hormone replacement therapy
contribute to mammographic breast density. After menopause, the breast glandular tissue gradually is replaced by fatty tissue, making mammographic interpretation much more accurate.
In the UK, all women are invited for screening once every three years beginning at age 50. As of 2009 the United States Preventive Services Task Force recommends that women over the age of 50 receive mammography once every two years. Some other organizations recommend mammograms begin as early as age 40 in normal-risk women, and take place more frequently, up to once each year.
Women at higher risk may benefit from earlier or more frequent screening. Women with one or more first-degree relatives (mother, sister, daughter) with premenopausal breast cancer often begin screening at an earlier age, perhaps at an age 10 years younger than the age when the relative was diagnosed with breast cancer.
insurance, 38% of currently uninsured women, and 33% of women uninsured for more than 12 months).
All U.S. states except Utah
require private health insurance plans and Medicaid to pay for breast cancer screening.
As of 1998, Medicare
(available to those aged 65 or older or who have been on Social Security Disability Insurance
for over 2 years) pays for annual screening mammography in women aged 40 or older.
All organized breast cancer screening programs in Canada offer clinical breast examinations for women aged 40 and over and screening mammography every two years for women aged 50–69. In 2003, about 61% of women aged 50–69 in Canada reported having had a mammogram within the past two years.
The UK's NHS
Breast Screening Programme, the first of its kind in the world, began in 1988 and achieved national coverage in the mid-1990s. It provides free breast cancer screening mammography every three years for all women in the UK aged 50 and over.
As 2006, about 76% of women aged 53–64 resident in England
had been screened at least once in the previous three years.
The Australian national breast screening program, BreastScreen Australia, was commenced in the early 1990s and invites women aged 50–69 to screening every 2 years. No routine clinical examination is performed, and the cost of screening is free to the point of diagnosis.
The Singapore national breast screening program, BreastScreen Singapore, is the only publicly funded national breast screening program in Asia, and enrolls women aged 50–64 for screening every two years. Like the Australian system, no clinical examination is performed routinely. Unlike most national screening systems, however, clients have to pay half of the cost of the screening mammogram; this is in line with the Singapore health system's core principle of co-payment for all health services.
The contribution of mammography to the early diagnosis of cancer is controversial, and for those found with benign lesions, mammography can create a high psychological and financial cost. Most women participating in mammography screening programs accept the risk of false positive recall, and the majority do not find it very distressing. Many patients find the recall very frightening, and are intensely relieved to discover that it was a false positive, as about 90% of women do.
A major effect of routine breast screening is to greatly increase the rate of early breast cancer detection, in particular for non-invasive ductal carcinoma in situ (DCIS), sometimes called "pre-breast cancer", which is almost never forms a lump and which generally cannot be detected except through mammography. While this ability to detect such very early breast malignancies is at the heart of claims that screening mammography can improve survival from breast cancer, it is also controversial. This is because a very large proportion of such cases will not progress to kill the patient, and thus mammography cannot be genuinely claimed to have saved any lives in such cases; in fact, it would lead to increased sickness and unnecessary surgery for such patients.
Consequently, finding and treating many cases of DCIS represents overdiagnosis
and overtreatment. Treatment is given to all women with DCIS because it is currently impossible to predict which patients with DCIS will have an indolent, non-fatal course, and which few will inevitably progress to invasive cancer and premature death if left untreated. Consequently, all patients with DCIS are treated in much the same way, with at least wide local excision, and sometimes mastectomy if the DCIS is very extensive. The cure rate for DCIS if treated appropriately is extremely high, partly because the majority of DCIS cases were harmless in the first place.
The phenomenon of finding pre-invasive malignancy or nonmalignant benign disease is commonplace in all forms of cancer screening, including pap smear
s for cervical cancer, fecal occult blood
testing for colon cancer, and prostate-specific antigen testing for prostate cancer. All of these tests have the potential to detect asymptomatic cancers, and all of them have a high rate of false positives and lead to invasive procedures that are unlikely to benefit the patient.
(MRI) has been shown to detect cancers not visible on mammograms. The chief strength of breast MRI is its very high negative predictive value
. A negative MRI can rule out the presence of cancer to a high degree of certainty, making it an excellent tool for screening in patients at high genetic risk or radiographically dense breasts, and for pre-treatment staging where the extent of disease is difficult to determine on mammography and ultrasound. MRI can diagnose benign proliferative change, fibroadenomas, and other common benign findings at a glance, often eliminating the need for costly and unnecessary biopsies or surgical procedures. The spatial and temporal resolution of breast MRI has increased markedly in recent years, making it possible to detect or rule out the presence of small in situ cancers, including ductal carcinoma in situ.
However, breast MRI has long been regarded to have disadvantages. For example, although it is 27–36% more sensitive, it has been claimed to be less specific than mammography. As a result, MRI studies may have more false positives
(up to 30%), which may have undesirable financial and psychological costs. It is also a relatively expensive procedure, and one which requires the intravenous injection of gadolinium
, which has been implicated in a rare reaction called nephrogenic systemic fibrosis
. Although NSF is extremely uncommon, patients with a history of renal disease may not be able to undergo breast MRI. Further, an MRI may not be used for screening patients with a pacemaker or breast reconstruction patients with a tissue expander due to the presence of metal.
Proposed indications for using MRI for screening include:
In addition, breast MRI may be helpful for screening in women who have had breast augmentation procedures involving intramammary injections of various foreign substances that may mask the appearances of breast cancer on mammography and/or ultrasound. These substances include silicone oil
and polyacrylamide gel.
Two studies published in 2007 demonstrated the strengths of MRI-based screening:
Based on this evidence, and the lack of effective alternative methods for screening in young women of very high genetic risk (either an extremely strong first degree family history or proven BRCA1 or BRCA2 oncogene mutation carrier status) for breast cancer, the Australian federal government decided to routinely reimburse annual breast MRI scans for such women under the age of 50 from January 2009 onwards.
does not detect cancers, but may reveal a propensity to develop cancer. Women who are known to have a higher risk of developing breast cancer usually undertake more aggressive screening programs.
A clinical practice guideline by the US Preventive Services Task Force recommends against routine referral for genetic counseling
or routine testing for BRCA mutation
s, on fair evidence that the harms outweigh the benefits. It also encourages a referral for counseling and testing in women whose a family history that indicates they have an increased risk of a BRCA mutation, on fair evidence of benefit. About 2% of American women have family histories that indicate an increased risk of having a medically significant BRCA mutation.
Asymptomatic
In medicine, a disease is considered asymptomatic if a patient is a carrier for a disease or infection but experiences no symptoms. A condition might be asymptomatic if it fails to show the noticeable symptoms with which it is usually associated. Asymptomatic infections are also called subclinical...
, apparently healthy women for breast cancer
Breast cancer
Breast cancer is cancer originating from breast tissue, most commonly from the inner lining of milk ducts or the lobules that supply the ducts with milk. Cancers originating from ducts are known as ductal carcinomas; those originating from lobules are known as lobular carcinomas...
in an attempt to achieve an earlier diagnosis. The assumption is that early detection will improve outcomes. A number of screening test have been employed including: clinical and self breast exams, mammography, genetic screening, ultrasound, and magnetic resonance imaging.
A clinical or self breast exam involves feeling the breast for lumps
Breast lump
Breast lump is a localized swelling that feels different from the surrounding breast tissue. It is a symptom/sign for a variety of conditions. As approximately 10% of breast lumps ultimately lead to a diagnosis of breast cancer, it is important for women with a breast lump to receive appropriate...
or other abnormalities. Evidence however does not support its use in women with a typical risk for breast cancer. The use of mammography
Mammography
Mammography is the process of using low-energy-X-rays to examine the human breast and is used as a diagnostic and a screening tool....
in universal screening for breast cancer is also controversial. The Cochrane collaboration
Cochrane Collaboration
The Cochrane Collaboration is a group of over 28,000 volunteers in more than 100 countries who review the effects of health care interventions tested in biomedical randomized controlled trials. A few more recent reviews have also studied the results of non-randomized, observational studies...
in 2009 concluded that it is unclear whether screening does more good than harm. Many national organizations still recommend it for most older women. If screening mammography (as opposed to diagnostic mammography) is chosen for women at normal risk for breast cancer, it should only be done every two years in women between the ages of 50 and 74. Several tools are available to help target breast cancer screening to older women with longer life expectancies. Similar imaging studies can be performed with magnetic resonance imaging
Magnetic resonance imaging
Magnetic resonance imaging , nuclear magnetic resonance imaging , or magnetic resonance tomography is a medical imaging technique used in radiology to visualize detailed internal structures...
.
Earlier, more aggressive, and more frequent screening is recommended for women at particularly high risk of developing breast cancer, such as those with a confirmed BRCA mutation
BRCA mutation
A BRCA mutation is a mutation in either of the genes BRCA1 and BRCA2. Harmful mutations in these genes produce a hereditary breast-ovarian cancer syndrome in affected families...
, those who have previously had breast cancer, and those with a strong family history of breast and ovarian cancer.
Abnormal findings on screening are further investigated by surgically removing a piece of the suspicious lumps (biopsy
Biopsy
A biopsy is a medical test involving sampling of cells or tissues for examination. It is the medical removal of tissue from a living subject to determine the presence or extent of a disease. The tissue is generally examined under a microscope by a pathologist, and can also be analyzed chemically...
) to examine them under the microscope. Ultrasound
Ultrasound
Ultrasound is cyclic sound pressure with a frequency greater than the upper limit of human hearing. Ultrasound is thus not separated from "normal" sound based on differences in physical properties, only the fact that humans cannot hear it. Although this limit varies from person to person, it is...
may be used to guide the biopsy needle during the procedure. Magnetic resonance imaging
Magnetic resonance imaging
Magnetic resonance imaging , nuclear magnetic resonance imaging , or magnetic resonance tomography is a medical imaging technique used in radiology to visualize detailed internal structures...
is used to guide treatment, but is not an established screening method for healthy women.
Breast exam
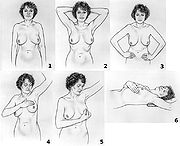
A 2003 Cochrane review found screening by breast self-examination or by clinical exam is not associated with death rates among women who report performing breast self-examination and does, like other breast cancer screening methods, increase harms, in terms of increased numbers of benign lesions identified and an increased number of biopsies performed. They conclude "screening by breast self-examination or physical examination cannot be recommended."
Mammography
MammographyMammography
Mammography is the process of using low-energy-X-rays to examine the human breast and is used as a diagnostic and a screening tool....
is a common screening method, since it is relatively fast and widely available in developed countries. Mammography is a type of radiography
Radiography
Radiography is the use of X-rays to view a non-uniformly composed material such as the human body. By using the physical properties of the ray an image can be developed which displays areas of different density and composition....
used on the breasts. Mammography is not useful in finding breast tumors in dense breast tissue characteristic of women under 40 years. It is typically used for two purposes: to aid in the diagnosis of a woman who is experiencing symptoms (called diagnostic mammography), and for medical screening of apparently healthy women (called screening mammography). In women over 50 without dense breasts, breast cancers detected by screening mammography are usually smaller and less aggressive than those detected by patients or doctors as a breast lump. This is because the most aggressive breast cancers are found in dense breast tissue which mammograms can not image.
The presumption is that by detecting the cancer in an earlier stage, women will be more likely to be cured by treatment. This assertion however has been challenged by recent reviews which have found the significance of these benefits to be questionable.
How it works
Frailty syndrome
The frailty syndrome is a collection of symptoms or markers, primarily due to the aging-related loss and dysfunction of skeletal muscle and bone, that place older adults at increased risk of adverse events such as death, disability, and institutionalization.-Sarcopenia:Sarcopenia, refers to loss...
women, who are unlikely to benefit from treatment.
Women who agree to be screened have their breasts X-rayed on a specialized X-ray machine. This exposes the woman's breasts to a small amount of ionizing radiation
Ionizing radiation
Ionizing radiation is radiation composed of particles that individually have sufficient energy to remove an electron from an atom or molecule. This ionization produces free radicals, which are atoms or molecules containing unpaired electrons...
, which has a very small, but non-zero, chance of causing cancer.
The X-ray image, called a radiograph, is sent to a physician who specializes in interpreting these images, called a radiologist. The image may be on plain photographic film
Photographic film
Photographic film is a sheet of plastic coated with an emulsion containing light-sensitive silver halide salts with variable crystal sizes that determine the sensitivity, contrast and resolution of the film...
or digital mammography
Digital mammography
Digital mammography is a specialized form of mammography that uses digital receptors and computers instead of x-ray film to help examine breast tissue for breast cancer. The electrical signals can be read on computer screens, permitting more manipulation of images to theoretically allow...
on a computer screen; despite the much higher cost of the digital systems, the two methods are generally considered equally effective. The equipment may use a computer-aided diagnosis
Computer-aided diagnosis
Computer-aided detection and computer-aided diagnosis are procedures in medicine that assist doctors in the interpretation of medical images. Imaging techniques in X-ray, MRI, and Ultrasound diagnostics yield a great deal of information, which the radiologist has to analyze and evaluate...
(CAD) system.
There is considerable variation in interpreting the images; the same image may be declared normal by one radiologist and suspicious by another. It can be helpful to compare the images to any previously taken images, as changes over time may be significant.
If a suspicious signs are identified in the image, then the woman is usually recalled for a second mammogram, sometimes after waiting six months to see whether the spot is growing, or a biopsy
Biopsy
A biopsy is a medical test involving sampling of cells or tissues for examination. It is the medical removal of tissue from a living subject to determine the presence or extent of a disease. The tissue is generally examined under a microscope by a pathologist, and can also be analyzed chemically...
of the breast. Most of these will prove to be false positives, resulting in sometimes debilitating anxiety
Anxiety
Anxiety is a psychological and physiological state characterized by somatic, emotional, cognitive, and behavioral components. The root meaning of the word anxiety is 'to vex or trouble'; in either presence or absence of psychological stress, anxiety can create feelings of fear, worry, uneasiness,...
over nothing. Most women recalled will undergo additional imaging only, without any further intervention. Recall rates are higher in the U.S. than in the UK.
Whether it works
On balance, screening mammography in older women noticeably increases medical treatment and saves a small number of lives. Usually, it has no effect on the outcome of the cancer. Screening targeted towards women with above-average risk produces more benefit than screening of women at normal or low risk for breast cancer.A 2009 Cochrane review estimated that mammography in women between 50 and 75 years old results in a relative risk reduction
Relative risk reduction
In epidemiology, the relative risk reduction is a measure calculated by dividing the absolute risk reduction by the control event rate.The relative risk reduction can be more useful than the absolute risk reduction in determining an appropriate treatment plan, because it accounts not only for the...
of death from breast cancer of 15% or an absolute risk reduction
Absolute risk reduction
In epidemiology, the absolute risk reduction or risk difference is the decrease in risk of a given activity or treatment in relation to a control activity or treatment. It is the inverse of the number needed to treat....
of 0.05%. Those who have mammograms however end up with increased surgeries, chemotherapy, radiotherapy and other potentially procedures resulting from the over-detection of harmless lumps. Many women will experience important psychological distress for many months because of false positive findings. Consequently, the value of routine mammography in women at low or average risk is controversial. With unnecessary treatment of ten women for every one woman whose life was prolonged, the authors concluded that routine mammography may do more harm than good.
If 1,000 women in their 50s are screened every year for ten years, the following outcomes are considered typical in the developed world:
- One woman's life will be extended due to earlier detection of breast cancer.
- 2–10 women will be overdiagnosed and needlessly treated for a cancer that would have stopped growing on its own or otherwise caused no harm during the woman's lifetime.
- 5–15 women will be treated for breast cancer, with the same outcome as if they had been detected after symptoms appeared.
- 250–500 will be incorrectly told they might have breast cancer (false positive).
- 125–250 will undergo breast biopsyBreast biopsySeveral methods for a breast biopsy now exist. The most appropriate method of biopsy for a patient depends upon a variety of factors, including the size, location, appearance and characteristics of the abnormality.- Fine needle aspiration :...
.
The outcomes are worse for women in their 20s, 30s, and 40s, as they are far less likely to have a life-threatening breast cancer, and more likely to have dense breasts that make interpreting the mammogram more difficult. Among women in their 60s, who have a somewhat higher rate of breast cancer, the proportion of positive outcomes to harms are better:
- For women in their 40s: 2,000 women would need to be screenedNumber needed to treatThe number needed to treat is an epidemiological measure used in assessing the effectiveness of a health-care intervention, typically a treatment with medication. The NNT is the average number of patients who need to be treated to prevent one additional bad outcome...
every year for 10 years to prevent one death from breast cancer. 1,000 of these women would experience false results and 250 healthy women would undergo unnecessary biopsies. - For women in their 50s: 1,339 women would need to be screened for every year for 10 years to prevent one death from breast cancer. Half of these women would experience false positives and one quarter would undergo unnecessary biopsies.
- For women in their 60s: 377 women would need to be screened for every year for 10 years to prevent one death from breast cancer. Half of these women would experience false positives and one quarter would undergo unnecessary biopsies.
Mammography is not generally considered as an effective screening technique for women at average or low risk of developing cancer who are less than 50 years old. For normal-risk women 40 to 49 years of age, the risks of mammography outweigh the benefits, and the US Preventive Services Task Force says that the evidence in favor of routine screening of women under the age of 50 is "weak". Part of the difficulty in interpreting mammograms in younger women stems from breast density. Radiographically, a dense breast has a preponderance of glandular tissue, and younger age or estrogen
Estrogen
Estrogens , oestrogens , or œstrogens, are a group of compounds named for their importance in the estrous cycle of humans and other animals. They are the primary female sex hormones. Natural estrogens are steroid hormones, while some synthetic ones are non-steroidal...
hormone replacement therapy
Hormone replacement therapy (menopause)
Hormone replacement therapy is a system of medical treatment for surgically menopausal, perimenopausal and to a lesser extent postmenopausal women...
contribute to mammographic breast density. After menopause, the breast glandular tissue gradually is replaced by fatty tissue, making mammographic interpretation much more accurate.
What is recommended
Different countries and organizations make different recommendations about screening mammography. The most important differences are the age at which it should begin and how frequently it should be performed in women at typical risk for developing breast cancer.In the UK, all women are invited for screening once every three years beginning at age 50. As of 2009 the United States Preventive Services Task Force recommends that women over the age of 50 receive mammography once every two years. Some other organizations recommend mammograms begin as early as age 40 in normal-risk women, and take place more frequently, up to once each year.
Women at higher risk may benefit from earlier or more frequent screening. Women with one or more first-degree relatives (mother, sister, daughter) with premenopausal breast cancer often begin screening at an earlier age, perhaps at an age 10 years younger than the age when the relative was diagnosed with breast cancer.
Health programs
In 2005, about 68% of all U.S. women age 40–64 had a mammogram in the past two years (75% of women with private health insurance, 56% of women with MedicaidMedicaid
Medicaid is the United States health program for certain people and families with low incomes and resources. It is a means-tested program that is jointly funded by the state and federal governments, and is managed by the states. People served by Medicaid are U.S. citizens or legal permanent...
insurance, 38% of currently uninsured women, and 33% of women uninsured for more than 12 months).
All U.S. states except Utah
Utah
Utah is a state in the Western United States. It was the 45th state to join the Union, on January 4, 1896. Approximately 80% of Utah's 2,763,885 people live along the Wasatch Front, centering on Salt Lake City. This leaves vast expanses of the state nearly uninhabited, making the population the...
require private health insurance plans and Medicaid to pay for breast cancer screening.
As of 1998, Medicare
Medicare (United States)
Medicare is a social insurance program administered by the United States government, providing health insurance coverage to people who are aged 65 and over; to those who are under 65 and are permanently physically disabled or who have a congenital physical disability; or to those who meet other...
(available to those aged 65 or older or who have been on Social Security Disability Insurance
Social Security Disability Insurance
Social Security Disability Insurance is a payroll tax-funded, federal insurance program of the United States government. It is managed by the Social Security Administration and is designed to provide income supplements to people who are physically restricted in their ability to be employed...
for over 2 years) pays for annual screening mammography in women aged 40 or older.
All organized breast cancer screening programs in Canada offer clinical breast examinations for women aged 40 and over and screening mammography every two years for women aged 50–69. In 2003, about 61% of women aged 50–69 in Canada reported having had a mammogram within the past two years.
The UK's NHS
National Health Service
The National Health Service is the shared name of three of the four publicly funded healthcare systems in the United Kingdom. They provide a comprehensive range of health services, the vast majority of which are free at the point of use to residents of the United Kingdom...
Breast Screening Programme, the first of its kind in the world, began in 1988 and achieved national coverage in the mid-1990s. It provides free breast cancer screening mammography every three years for all women in the UK aged 50 and over.
As 2006, about 76% of women aged 53–64 resident in England
England
England is a country that is part of the United Kingdom. It shares land borders with Scotland to the north and Wales to the west; the Irish Sea is to the north west, the Celtic Sea to the south west, with the North Sea to the east and the English Channel to the south separating it from continental...
had been screened at least once in the previous three years.
The Australian national breast screening program, BreastScreen Australia, was commenced in the early 1990s and invites women aged 50–69 to screening every 2 years. No routine clinical examination is performed, and the cost of screening is free to the point of diagnosis.
The Singapore national breast screening program, BreastScreen Singapore, is the only publicly funded national breast screening program in Asia, and enrolls women aged 50–64 for screening every two years. Like the Australian system, no clinical examination is performed routinely. Unlike most national screening systems, however, clients have to pay half of the cost of the screening mammogram; this is in line with the Singapore health system's core principle of co-payment for all health services.
Criticisms
Most women significantly overestimate both their own risk of dying from breast cancer and the effect screening mammography could have on it. Some researchers worry that if women correctly understood that screening programs offer a small, but statistically significant benefit, more women would refuse to participate.The contribution of mammography to the early diagnosis of cancer is controversial, and for those found with benign lesions, mammography can create a high psychological and financial cost. Most women participating in mammography screening programs accept the risk of false positive recall, and the majority do not find it very distressing. Many patients find the recall very frightening, and are intensely relieved to discover that it was a false positive, as about 90% of women do.
A major effect of routine breast screening is to greatly increase the rate of early breast cancer detection, in particular for non-invasive ductal carcinoma in situ (DCIS), sometimes called "pre-breast cancer", which is almost never forms a lump and which generally cannot be detected except through mammography. While this ability to detect such very early breast malignancies is at the heart of claims that screening mammography can improve survival from breast cancer, it is also controversial. This is because a very large proportion of such cases will not progress to kill the patient, and thus mammography cannot be genuinely claimed to have saved any lives in such cases; in fact, it would lead to increased sickness and unnecessary surgery for such patients.
Consequently, finding and treating many cases of DCIS represents overdiagnosis
Overdiagnosis
Overdiagnosis is the diagnosis of "disease" that will never cause symptoms or death during a patient's lifetime. Overdiagnosis is the least familiar side effect of testing for early forms of disease – and, arguably, the most important...
and overtreatment. Treatment is given to all women with DCIS because it is currently impossible to predict which patients with DCIS will have an indolent, non-fatal course, and which few will inevitably progress to invasive cancer and premature death if left untreated. Consequently, all patients with DCIS are treated in much the same way, with at least wide local excision, and sometimes mastectomy if the DCIS is very extensive. The cure rate for DCIS if treated appropriately is extremely high, partly because the majority of DCIS cases were harmless in the first place.
The phenomenon of finding pre-invasive malignancy or nonmalignant benign disease is commonplace in all forms of cancer screening, including pap smear
Pap smear
The Papanicolaou test is a screening test used in to detect pre-cancerous and cancerous processes in the endocervical canal of the female reproductive system. Changes can be treated, thus preventing cervical cancer...
s for cervical cancer, fecal occult blood
Fecal occult blood
Fecal occult blood refers to blood in the feces that is not visibly apparent. A fecal occult blood test checks for hidden blood in the stool...
testing for colon cancer, and prostate-specific antigen testing for prostate cancer. All of these tests have the potential to detect asymptomatic cancers, and all of them have a high rate of false positives and lead to invasive procedures that are unlikely to benefit the patient.
Molecular breast imaging
Molecular breast imaging is a nuclear medicine technique that is currently under study. It shows promising results for imaging people with dense breast tissue and may have accuracies comparable to MRI. MBI is claimed to be cheaper than MRI.Breast MRI
Magnetic resonance imagingMagnetic resonance imaging
Magnetic resonance imaging , nuclear magnetic resonance imaging , or magnetic resonance tomography is a medical imaging technique used in radiology to visualize detailed internal structures...
(MRI) has been shown to detect cancers not visible on mammograms. The chief strength of breast MRI is its very high negative predictive value
Negative predictive value
In statistics and diagnostic testing, the negative predictive value is a summary statistic used to describe the performance of a diagnostic testing procedure. It is defined as the proportion of subjects with a negative test result who are correctly diagnosed. A high NPV means that when the test...
. A negative MRI can rule out the presence of cancer to a high degree of certainty, making it an excellent tool for screening in patients at high genetic risk or radiographically dense breasts, and for pre-treatment staging where the extent of disease is difficult to determine on mammography and ultrasound. MRI can diagnose benign proliferative change, fibroadenomas, and other common benign findings at a glance, often eliminating the need for costly and unnecessary biopsies or surgical procedures. The spatial and temporal resolution of breast MRI has increased markedly in recent years, making it possible to detect or rule out the presence of small in situ cancers, including ductal carcinoma in situ.
However, breast MRI has long been regarded to have disadvantages. For example, although it is 27–36% more sensitive, it has been claimed to be less specific than mammography. As a result, MRI studies may have more false positives
Type I and type II errors
In statistical test theory the notion of statistical error is an integral part of hypothesis testing. The test requires an unambiguous statement of a null hypothesis, which usually corresponds to a default "state of nature", for example "this person is healthy", "this accused is not guilty" or...
(up to 30%), which may have undesirable financial and psychological costs. It is also a relatively expensive procedure, and one which requires the intravenous injection of gadolinium
Gadolinium
Gadolinium is a chemical element with the symbol Gd and atomic number 64. It is a silvery-white, malleable and ductile rare-earth metal. It is found in nature only in combined form. Gadolinium was first detected spectroscopically in 1880 by de Marignac who separated its oxide and is credited with...
, which has been implicated in a rare reaction called nephrogenic systemic fibrosis
Nephrogenic systemic fibrosis
Nephrogenic systemic fibrosis or nephrogenic fibrosing dermopathy is a rare and serious syndrome that involves fibrosis of skin, joints, eyes, and internal organs. Its cause is not fully understood...
. Although NSF is extremely uncommon, patients with a history of renal disease may not be able to undergo breast MRI. Further, an MRI may not be used for screening patients with a pacemaker or breast reconstruction patients with a tissue expander due to the presence of metal.
Proposed indications for using MRI for screening include:
- Strong family history of breast cancer
- Patients with BRCA-1 or BRCA-2 oncogene mutations
- Evaluation of women with breast implants
- History of previous lumpectomy or breast biopsy surgeries
- Axillary metastasis with an unknown primary tumor
- Very dense or scarred breast tissue
In addition, breast MRI may be helpful for screening in women who have had breast augmentation procedures involving intramammary injections of various foreign substances that may mask the appearances of breast cancer on mammography and/or ultrasound. These substances include silicone oil
Silicone oil
A silicone oil is any polymerized siloxanes with organic side chains. They are formed of alternating silicon-oxygen atoms or siloxane, rather than carbon atoms . Other species attach to the tetravalent silicon atoms, not to the divalent oxygen atoms which are fully committed to forming the...
and polyacrylamide gel.
Two studies published in 2007 demonstrated the strengths of MRI-based screening:
- In March 2007, an article published in the New England Journal of MedicineNew England Journal of MedicineThe New England Journal of Medicine is an English-language peer-reviewed medical journal published by the Massachusetts Medical Society. It describes itself as the oldest continuously published medical journal in the world.-History:...
demonstrated that in 3.1% of patients with breast cancer, whose contralateral breast was clinically and mammographically tumor-free, MRI could detect breast cancer. Sensitivity for detection of breast cancer in this study was 91%, specificity 88%. - In August 2007, an article published in The LancetThe LancetThe Lancet is a weekly peer-reviewed general medical journal. It is one of the world's best known, oldest, and most respected general medical journals...
compared MRI breast cancer screening to conventional mammographic screening in 7,319 women. MRI screening was highly more sensitive (97% in the MRI group vs. 56% in the mammography group) in recognizing early high-grade Ductal Carcinoma in situ (DCIS)Carcinoma in situCarcinoma in situ is an early form of cancer that is defined by the absence of invasion of tumor cells into the surrounding tissue, usually before penetration through the basement membrane. In other words, the neoplastic cells proliferate in their normal habitat, hence the name "in situ"...
, the most important precursor of invasive carcinoma. Despite the high sensitivity, MRI screening had a positive predictive valuePositive predictive valueIn statistics and diagnostic testing, the positive predictive value, or precision rate is the proportion of subjects with positive test results who are correctly diagnosed. It is a critical measure of the performance of a diagnostic method, as it reflects the probability that a positive test...
of 52%, which is totally accepted for cancer screening tests. The author of a comment published in the same issue of The Lancet concludes that "MRI outperforms mammography in tumour detection and diagnosis."
Based on this evidence, and the lack of effective alternative methods for screening in young women of very high genetic risk (either an extremely strong first degree family history or proven BRCA1 or BRCA2 oncogene mutation carrier status) for breast cancer, the Australian federal government decided to routinely reimburse annual breast MRI scans for such women under the age of 50 from January 2009 onwards.
BRCA testing
Genetic testingGenetic testing
Genetic testing is among the newest and most sophisticated of techniques used to test for genetic disorders which involves direct examination of the DNA molecule itself. Other genetic tests include biochemical tests for such gene products as enzymes and other proteins and for microscopic...
does not detect cancers, but may reveal a propensity to develop cancer. Women who are known to have a higher risk of developing breast cancer usually undertake more aggressive screening programs.
A clinical practice guideline by the US Preventive Services Task Force recommends against routine referral for genetic counseling
Genetic counseling
Genetic counseling or traveling is the process by which patients or relatives, at risk of an inherited disorder, are advised of the consequences and nature of the disorder, the probability of developing or transmitting it, and the options open to them in management and family planning...
or routine testing for BRCA mutation
BRCA mutation
A BRCA mutation is a mutation in either of the genes BRCA1 and BRCA2. Harmful mutations in these genes produce a hereditary breast-ovarian cancer syndrome in affected families...
s, on fair evidence that the harms outweigh the benefits. It also encourages a referral for counseling and testing in women whose a family history that indicates they have an increased risk of a BRCA mutation, on fair evidence of benefit. About 2% of American women have family histories that indicate an increased risk of having a medically significant BRCA mutation.
External links
- Breast cancer screening page from the National Cancer InstituteNational Cancer InstituteThe National Cancer Institute is part of the National Institutes of Health , which is one of 11 agencies that are part of the U.S. Department of Health and Human Services. The NCI coordinates the U.S...
- Breast Cancer Screening from AARP.orgAARPAARP, formerly the American Association of Retired Persons, is the United States-based non-governmental organization and interest group, founded in 1958 by Ethel Percy Andrus, PhD, a retired educator from California, and based in Washington, D.C. According to its mission statement, it is "a...

