
Cancer pain
Encyclopedia
Pain is a symptom frequently associated with cancer
. Cancer can cause pain by irritating or damaging nerves, by stimulating nociceptor
s (pain sensitive nerve fibers), or by releasing chemicals that make nociceptors respond to normally non-painful stimuli. Cancer pain may be caused by the tumor itself or by medical interventions in the diagnosis and treatment of cancer. Pain can be eliminated or well controlled in 80–90% of cases, but nearly one in two patients receives less-than-optimal care.
of pain is distinct from the unpleasantness associated with it. For example, it is possible in some cases, through psychosurgery
or drug treatment, to remove the unpleasantness from pain without affecting its intensity, and cognitive processes such as placebo
and hypnotic suggestion can temporarily reduce pain's unpleasantness but leave its intensity unchanged. Some drug therapies and other interventions can remove both the sensation of pain and its unpleasantness, and certain emotional states, such as the excitement of sport or war, can produce the same effect.
Pain makes complex thought more difficult: it impairs attention control, working memory
, mental flexibility
, problem solving, and information processing speed
, and it is associated with increased depression
, anxiety, fear, and anger. Cancer pain is classed as acute (usually caused by medical investigation or treatment) or chronic
. About 75% of patients with chronic cancer pain have pain caused by the cancer itself. In most of the remainder, pain is the result of treatment.
, swelling, and hardening or thickening of the surrounding tissue, whose previously well-controlled pain escalated significantly over several days. Antibiotic treatment produced pain relief in all patients within three days.
s; brain tumors cause pain by pressing on blood vessels or the membrane
that encapsulates the brain, or indirectly by causing edema
which may compress pain-sensitive tissue.
Ten percent of patients with disseminated cancer develop meningeal carcinomatosis
, where metastatic seedlings develop in the meninges
of both brain and spinal cord, with possible invasion of the spinal cord or brain. Melanoma
and breast
and lung cancer
account for 90 percent of such cases. Headache (often severe and possibly associated with nausea, vomiting, photophobia
and neck rigidity) and back pain are frequently the first symptoms. Paresthesia
, bowel or bladder dysfunction and lower motor neuron weakness are common features.
 About three percent of cancer patients experience spinal cord compression, usually from expansion of the vertebral body or pedicle
About three percent of cancer patients experience spinal cord compression, usually from expansion of the vertebral body or pedicle
(fig. 1) due to metastasis, sometimes involving collapse of the vertebral body. Occasionally compression is caused by nonvertebral metastasis adjacent to the spinal cord. Compression of a spinal nerve root (fig. 3) produces radicular pain
, and compression of the long tracts of the cord itself produces funicular pain. Seventy percent of cases involve the thoracic, 20 percent the lumbar, and 10 percent the cervical spine; and about 20 percent of cases involve multiple sites of compression. The nature of the pain depends on the location of the compression.
Between one and five percent of cancer patients suffer peripheral neuropathy
due to infiltration or compression of a peripheral nerve
by a primary tumor. Small cell lung cancer and, less often, cancer of the breast, colon or ovary may produce inflammation of the dorsal root ganglia
(fig. 3), precipitating burning, tingling pain in the extremities, with occasional "lightening" or lancenating pains.
Brachial plexopathy is a common product of Pancoast tumor
, lymphoma and breast cancer, and can produce severe burning dysesthesic
pain on the back of the hand, and cramping, crushing forearm pain.
cancers develop bone metastases. It is commonly felt as tenderness, with constant background pain and instances of spontaneous or movement-related exacerbation, and is frequently described as severe. Tumors in the marrow instigate a vigorous immune response which enhances pain sensitivity, and they release chemicals that stimulate nociceptors. As they grow, tumors compress, infiltrate, cut off blood supply to, or consume
body tissues, which can cause nociceptive or neuropathic pain.
Rib fractures, common in breast, prostate and other cancers with rib metastases, can cause brief severe pain on twisting the trunk, coughing, laughing, breathing deeply or moving between sitting and lying.
The base of the skull may be affected by metastases from cancer of the bronchus
, breast or prostate, or cancer may spread directly to this area from the nasopharynx
, and this may cause headache, facial paresthesia
, dysesthesia
or pain, or cranial nerve dysfunction – the exact symptoms depending on the cranial nerves impacted.
to the lumbar
region. Lumbosacral plexopathy is often caused by recurrence of cancer in the presacral space
, and may refer to the external genitalia or perineum
rather than the legs. Local recurrence of cancer attached to the side of the pelvic wall may cause pain in one of the iliac fossa
e. Pain on walking that confines the patient to bed indicates possible cancer adherence to or invasion of the iliacus muscle
. Pain in the hypogastrium
(between the navel and pubic bone
) is often found in cancers of the uterus and bladder, and sometimes in colorectal cancer especially if infiltrating or attached to either uterus or bladder.
pain is diffuse and difficult to locate, and is often referred
to more distant, usually superficial, sites.
A tumor can expand the size of the liver several times, and consequent stretching of its capsule can cause aching pain in the right hypochondrium
. Other causes of pain in enlarged liver
are traction of the supporting ligaments when standing or walking, internal bleeding of the liver, the liver pressing against the rib cage or pinching the wall of the abdomen, and straining the lumbar spine. In some postures the liver may pinch the parietal peritoneum
against the lower rib cage, producing sharp, transitory pain, relieved by changing position. The tumor may also infiltrate the liver's capsule, causing dull, and sometimes stabbing pain.
Cancer of the kidneys and spleen produces less pain than that caused by liver tumor – kidney tumors eliciting pain only once the organ has been almost totally destroyed and the cancer has invaded the surrounding tissue or adjacent pelvis. Pressure on the kidney or ureter
from a tumor outside the kidney can cause extreme flank pain. Local recurrence of cancer after the removal of a kidney can cause pain in the lumbar back, or L1
or L2
spinal nerve pain in the groin or upper thigh, accompanied by weakness and numbness of the iliopsoas
muscle, exacerbated by activity.
The pain of intestinal tumors may be the result of disturbed motility
, dilation, altered blood flow or ulceration. Malignant lymphomas of the gastrointestinal tract can produce large tumors with significant ulceration and bleeding. Inflammation of artery walls and tissue adjacent to nerves is common in tumors of abdominal and urogenital hollow organs.
Cancer in the bronchial tree is usually painless, but ear and facial pain on one side of the head has been reported in some patients. This is referred
via the auricular branch of the vagus nerve.
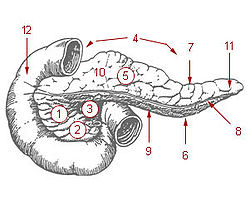 Ten percent of patients with cancer of the pancreatic body or tail
Ten percent of patients with cancer of the pancreatic body or tail
experience pain, whereas 90 percent of those with cancer of the pancreatic head
will, especially if the tumor is near the hepatopancreatic ampulla
. The pain appears on the left or right upper abdomen, is constant, and increases in intensity over time. It is in some cases relieved by leaning forward and heightened by lying on the stomach. Back pain may be present and, if intense, may spread left and right. Back pain may be referred
from the pancreas, or may indicate the cancer has penetrated paraspinal muscle, or entered the retroperitoneum
and paraaortic lymph node
s
Pain of the rectum may be experienced even after the rectum has been surgically removed
. Local recurrence of rectal cancer may cause mild (described as "pressure") or strong pain on sitting; or pain on standing or walking (described as "dragging"). The latter may indicate a deeper recurrence involving attachment to muscle or fascia
. A local tumor in the rectum or recurrence involving the presacral plexus may cause pain normally associated with an urgent need to defecate. This pain may, rarely, be phantom
after surgical removal of the rectum. Distressing, intense, stabbing, "red hot poker" pain is sometimes reported. Pain within a few weeks of surgical removal of the rectum is usually neuropathic
due to the surgery, and described in one study as spontaneous, intermittent, mild to moderate shooting and bursting, or tight and aching. Pain emerging after three months usually signals recurrence, and was described as deep, sharp, aching, intense, and continuous, made worse by sitting or pressure. In over half of patients with late-onset pain in the above study, pain was ameliorated by analgesic
s.
Infection or cancer may irritate the trigone of the urinary bladder, causing spasm of the detrusor urinae muscle
(the muscle that squeezes urine from the urinary bladder
), resulting in deep pain above the pubic bone, possibly referred to the tip of the penis, lasting from a few minutes to half an hour.
of the peritoneum
may cause pain through pressure of the metastases on peripheral nerves, inflammation, or disordered visceral motility. Once a tumor has penetrated or perforated hollow viscera, acute inflammation of the peritoneum appears, inducing severe abdominal pain. Pleural carcinomatosis is normally painless.
, radiation fibrosis, myelopathy
, osteoradionecrosis, neuropathy or plexopathy
; chemotherapy, often associated with mucositis
, joint pain
, muscle pain
, peripheral neuropathy
and abdominal pain due to diarrhea or constipation; hormone therapy, which sometimes causes pain flares; targeted therapies, such as trastuzumab and rituximab, which can cause muscle, joint or chest pain; angiogenesis inhibitors like bevacizumab, known to sometimes cause bone pain; surgery, which may produce postoperative pain, post-amputation pain or pelvic floor myalgia
; and invasive investigations such as lumbar puncture
, bone marrow biopsy
, venipuncture
, paracentesis
, and thoracentesis
.
, muscle pain, joint pain, abdominal pain caused by diarrhea or constipation, and peripheral neuropathy
(pain and numbness in the hands, wrists, feet and ankles).
/vinblastine
, aclitaxel/docetaxel, cisplatin
/oxaliplatin
/carboplatin
, thalidomide
, and bortezomib
, can cause chemotherapy-induced peripheral neuropathy (CIPN), experienced as tingling numbness, intense pain, and hypersensitivity to cold in a glove and sock pattern. CIPN often follows the first chemotherapy dose and increases in severity as treatment continues, but this progressive degeneration usually halts at completion of treatment. The platinum-based drugs such as oxaliplatin and cisplatin are the exception; with these drugs, sensation may continue to deteriorate for several months after the end of treatment. Some CIPN appears to be irreversible.
Pain can often be helped with drug treatment but the numbness is usually resistant to treatment.
CIPN disrupts leisure, work and family relations, and the pain of CIPN is often accompanied by sleep and mood disturbance, fatigue and functional difficulties. A 2007 American study found that most patients did not recall being told to expect CIPN, and doctors monitoring the condition rarely asked how it affects daily living but focused on practical effects such as dexterity and gait.
It is not known what causes the condition, but microtubule
and mitochondrial damage, and leaky blood vessels near nerve cells are some of the possibilities being explored. It is unknown what percentage of patients are affected.
As possible preventative interventions, the American National Cancer Institute
Symptom Management and Health-related Quality of Life Steering Committee recommends continued investigation of glutathione
, and intravenous calcium and magnesium, which have shown early promise in limited human trials; acetyl-L-carnitine, which was effective in animal models and on diabetes and HIV patients; and the anti-oxidant alpha-lipoic acid.
) of the fibrous tissue enveloping the brachial
or lumbosacral
plexus, which can result in damage to the nerves over time (6 months to 20 years). This nerve damage can cause numbness, "pins and needles
" or unpleasant sensation
and weakness in the affected limb. If pain develops, it is described as diffuse, severe, burning pain, increasing over time, in part or all of the affected limb.
" can manifest from six weeks to six months after treatment; the usual symptom is a Lhermitte sign ("a brief, unpleasant sensation of numbness, tingling and often electric-like discharge going from the neck to the spine and extremities, triggered by neck flexion"), and is usually followed by improvement two to nine months after onset, though in some cases symptoms persist for a long time. "Late delayed radiation-induced myelopathy" may occur six months to ten years after treatment. The typical presentation is Brown-Séquard syndrome
(a motor deficit and numbness to touch and vibration on one side of the body and loss of pain and temperature sensation on the other). Onset may be sudden but is usually progressive. Some patients improve and others deteriorate.
and level of function and a relatively painless death. Though 80–90% of cancer pain can be eliminated or well controlled, nearly half of all patients throughout the world with cancer pain receive less than optimal care.
(WHO) and others,
doctors and nurses frequently lack understanding of key aspects of pain management including assessment, dosing, tolerance and addiction, and many do not know that pain elimination is possible in most cases, that this should be offered wherever possible, and where complete elimination of suffering is not achievable due to intolerable drug side effects, the maximum tolerable dose should be offered.
Systemic problems in the delivery of pain management include failure in the clinical setting to refer patients for pain management, inadequate reimbursement for pain management, lack of stocks of pain medicines in poorer areas, out-dated government policy on cancer pain management, and legal restraints on prescription of opioid medication.
Patients may not report pain due to a belief that pain is inevitable, fear of side effects of treatment, fear of developing addiction or tolerance to opioids, fear of distracting the doctor from treating the illness, or fear of masking a symptom important for monitoring progress of the disease. Patients may be reluctant to take adequate pain medicine because they are unaware of the prognosis
or unwilling to accept the diagnosis. Patient failure to report pain or misguided reluctance to take pain medicine can be overcome by sensitive coaching.
Cancer is a dynamic process, and pain interventions need to reflect this. Several different treatment modalities may be required over time, as the disease progresses. Pain managers should clearly explain to the patient the cause of the pain and the various treatment possibilities, and should consider, as well as drug therapy, directly modifying the underlying disease, raising the pain threshold, interrupting, destroying or stimulating pain pathways, and suggesting lifestyle modification. The relief of psychological, social and spiritual distress is a key element in effective pain management.
, dipyrone, non-steroidal anti-inflammatory drug
s or COX-2 inhibitor
s. Then, if complete pain relief is not achieved or disease progression necessitates more aggressive treatment, mild opioids such as codeine phosphate, dextropropoxyphene
, dihydrocodeine
or tramadol
are added to the existing non-opioid regime. If this is or becomes insufficient, mild opioids are replaced by stronger opioids such as morphine, while continuing the non-opioid therapy, escalating opioid dose until the patient is pain-free or the maximum possible relief without intolerable side effects has been achieved. If the initial presentation is severe cancer pain, this stepping process should be skipped and a strong opioid should be started immediately in combination with a non-opioid analgesic.
The usefulness of the second step is being debated in the clinical and research communities. Some are challenging the pharmacological validity of the step and, pointing to the higher toxicity and low efficacy of mild opioids, argue that they, with the possible exception of tramadol due to its unique action, could be replaced by smaller doses of strong opioids.
Antiemetic
and laxative
treatment should be commenced concurrently with strong opioids, to counteract the usual nausea and constipation. Nausea normally resolves after two or three weeks of treatment but laxatives will need to be aggressively maintained. More than half of patients with advanced cancer and pain will need strong opioids, and these in combination with non-opioids can produce acceptable analgesia in 70–90 percent of cases. Sedation and cognitive impairment usually occur with the initial dose or a significant increase in dosage of a strong opioid, but improve after a week of consistent dosage.
Analgesics should not be taken "on demand" but "by the clock" (every 3–6 hours), with each dose delivered before the preceding dose has worn off, in doses sufficiently high to ensure continuous pain relief. Patients taking slow-release morphine should also be provided with immediate-release ("rescue") morphine to use as necessary, for pain spikes that are not suppressed by their regular medication.
Oral analgesia is the cheapest, simplest and most acceptable mode of delivery. Other delivery routes such as sublingual, topical, parenteral, rectal or spinal should be considered if the need is urgent, or in case of vomiting, impaired swallow, obstruction of the gastrointestinal tract, poor absorption or coma. Liver and kidney disease can affect the biological activity of analgesics. When such patients are treated with oral opioids they must be monitored for the possible need to reduce dose, extend dosing intervals, or switch to other opioids or other modes of delivery.
Not all pain yields completely to classic analgesics, and drugs that are not traditionally considered analgesics but which effect pain relief in certain cases, such as steroids or bisphosphonates, may be employed concurrently with analgesics at any stage. Tricyclic antidepressants, class I antiarrhythmics
, or anticonvulsants are the drugs of choice for neuropathic pain. Up to 90 percent of patients at death are using such "adjuvant
s". Many adjuvants carry a significant risk of serious complications.
Anxiety reduction can reduce the unpleasantness of pain but is least effective for moderate or severe pain. Since anxiolytic
s such as benzodiazepines, psychotropic drugs and major tranquilizer
s add to sedation, they should only be used to address anxiety
, depression
, disturbed sleep or muscle spasm.
Targets for neurolytic block include the celiac plexus
, most commonly for cancer of the gastrointestinal tract up to the transverse colon, and pancreatic cancer, but also for stomach cancer, gall bladder cancer, adrenal mass, common bile duct cancer, chronic pancreatitis and active intermittent porphyria
; the splanchnic nerve, for retroperitoneal pain, and similar conditions to those addressed by the celiac plexus block but, because of its higher rate of complications, used only if the celiac plexus block is not producing adequate relief; hypogastric plexus
, "for cancer affecting the descending colon, sigmoid colon and rectum," as well as cancers of the bladder, prostatic urethra, prostate, seminal vesicles, testicles, uterus, ovary and vaginal fundus; ganglion impar
, for the perinium, vulva, anus, distal rectum, distal urethra, and distal third of the vagina; the stellate ganglion
, usually for head and neck cancer, or sympathetically mediated arm and hand pain; the intercostal nerves
, which serve the skin of the chest and abdomen; and a posterior root ganglion
may be injured by targeting the root inside the subarachnoid cavity
(fig.3), most effective for pain in the chest or abdominal wall, but also used for other areas including arm/hand or leg/foot pain.
, hydromorphone
, fentanyl, sufentanyl and meperidine directly into the subarachnoid cavity (fig. 3) provides enhanced analgesia with reduced systemic side effects, and has reduced the level of pain in otherwise intractable cases. The anxiolytic clonidine
, or the nonopioid analgesic ziconotide, and local anesthetics such as bupivacaine
, ropivacaine
or tetracaine
may also be infused along with the opioid.
. Between this and the surrounding vertebrae is the epidural space
, filled with connective tissue, fat and blood vessels, and crossed by the spinal nerve roots. A catheter
may be inserted into this space for three to six months, to deliver anesthetics or analgesics. The line carrying the drug may be threaded under the skin to emerge at the front of the patient, a process called tunneling. This is recommended with long term use so as to reduce the chance of any infection at the exit site reaching the epidural space.
, and the generator is worn externally for several days to assess efficacy. If pain is reduced by more than half, the therapy is deemed to be suitable. A small pocket is cut into the tissue beneath the skin of the upper buttocks, chest wall or abdomen and the leads are threaded under the skin from the stimulation site to the pocket, where they are attached to the snugly-fitting generator. It seems to be more helpful with neuropathic and ischemic pain than nociceptive pain, and is not often used in the treatment of cancer pain.
and periventricular gray for nociceptive pain, and the internal capsule
, ventral posterolateral nucleus
and ventral posteromedial nucleus
for neuropathic pain – has produced impressive results with some patients but results vary and appropriate patient selection is important. One study of seventeen patients with intractable cancer pain found that thirteen were virtually pain free and only four required opioid analgesics on release from hospital after the intervention. Most ultimately did resort to opioids, usually in the last few weeks of life.
is the destruction of the pituitary gland
, and has been used successfully on metastatic breast and prostate cancer pain.
or central
nervous tissue is now rarely used in the treatment of pain. Procedures include neurectomy, cordotomy, dorsal root entry zone lesioning, and cingulotomy.
Neurectomy
involves cutting a peripheral nerve, and is (rarely) used in patients with short life expectancy who are unsuitable for drug therapy due to ineffectiveness or intolerance. The dorsal (sensory) root
or dorsal root ganglion
may be usefully targeted (called rhizotomy
); with the dorsal root ganglion possibly the more effective target because some sensory fibers enter the spinal cord from the dorsal root ganglion via the ventral (motor) root
, and these would not be interrupted by dorsal root neurectomy. Because peripheral nerves often carry both sensory and motor fibers, motor impairment is a possible side effect of neurectomy. A common result of this procedure is "deafferentation pain" where, 6–9 months after surgery, the original pain returns at greater intensity.
Cordotomy
involves cutting into the spinothalamic tract
s, which run up the front/side (anterolateral) quadrant of the spinal cord, carrying heat and pain signals to the brain (fig. 4). Pancoast tumor pain has been effectively treated with dorsal root entry zone (DREZ) lesioning – damaging a region of the spinal cord where peripheral pain signals cross to spinal cord fibers – this is major surgery, carrying the risk of significant neurological side-effects. Cingulotomy involves cutting the fibers that carry signals directly from the cingulate gyrus to the entorhinal cortex
in the brain. It reduces the unpleasantness of pain without affecting its intensity, but may have cognitive
side-effects.
Some, especially exhausted, terminally ill patients, may not wish to be involved in making pain management decisions, and delegate such choices to the professionals. The patient's participation is a right not an obligation, and though reduced patient involvement may result in less than optimal pain management, this choice should be respected.
As professionals become better informed about the interdependent relationship between physical, emotional, social and spiritual pain, and the demonstrated benefit to physical pain from alleviation of these other forms of suffering, they may be tempted to question the patient and family about personal relationships. Unless the patient has asked for such psychosocial intervention, or at least freely consented to such questioning, this would be an ethically unjustifiable intrusion into the patient's very personal affairs, analogous to providing drugs without the patient's informed consent.
A professional's obligation to alleviate suffering may occasionally come into conflict with the obligation to prolong life. If a terminally ill patient prefers to be free of pain, despite sedation and the risk of shortening life, they should be provided with their desired pain relief, at the cost of sedation and a possibly slightly shorter life. Where a patient is unable to be involved in this decision, the law and the medical profession in the United Kingdom allow the doctor to assume the patient would prefer to be pain-free, and provide adequate analgesia, even if this treatment may slightly hasten death. It is taken that the underlying cause of death in this case is the illness and not the necessary pain management.
A philosophical justification for this approach is the doctrine of double effect, where, to justify an act involving both a good and a bad effect, four conditions are necessary: the act must be good overall or morally neutral, the person acting must intend only the good effect with the bad effect as an unwanted side effect, the bad effect must not be the cause of the good effect, and the good effect must outweigh the bad. Just as an oncologist who intends to treat cancer may foresee but not intend nausea and other effects of chemotherapy, so a doctor treating suffering may foresee but not intend shortening life.
A 2003 review comparing studies of patients at all stages of cancer yielded a mean prevalence of 48%, ranging from 38% to 100%. Studies of patients at all stages with primary cancer in the head and neck, genitourinary system, prostate or esophagus reported a mean pain prevalence of 70%. Evidence for prevalence of pain in newly diagnosed cancer is scarce. One study found pain in 38% of newly diagnosed cases, and another found 35% of new patients had experienced pain in the preceding two weeks, while a third reported that pain was an early symptom in 18%-49% of cases. Comparison of twenty seven studies of the prevalence of pain in advanced cancer found a weighted mean prevalence of 74%, with reported prevalence rates ranging from 53% to 100%. Metastatic cancer is associated with a higher prevalence of pain than nonmetastatic cancer but this may be related to the disease stage. About 33% of cancer survivors report chronic pain after treatment has been completed.
Cancer
Cancer , known medically as a malignant neoplasm, is a large group of different diseases, all involving unregulated cell growth. In cancer, cells divide and grow uncontrollably, forming malignant tumors, and invade nearby parts of the body. The cancer may also spread to more distant parts of the...
. Cancer can cause pain by irritating or damaging nerves, by stimulating nociceptor
Nociceptor
A nociceptor is a sensory receptor that responds to potentially damaging stimuli by sending nerve signals to the spinal cord and brain. This process, called nociception, usually causes the perception of pain.-History:...
s (pain sensitive nerve fibers), or by releasing chemicals that make nociceptors respond to normally non-painful stimuli. Cancer pain may be caused by the tumor itself or by medical interventions in the diagnosis and treatment of cancer. Pain can be eliminated or well controlled in 80–90% of cases, but nearly one in two patients receives less-than-optimal care.
Pain
The sensationSense
Senses are physiological capacities of organisms that provide inputs for perception. The senses and their operation, classification, and theory are overlapping topics studied by a variety of fields, most notably neuroscience, cognitive psychology , and philosophy of perception...
of pain is distinct from the unpleasantness associated with it. For example, it is possible in some cases, through psychosurgery
Psychosurgery
Psychosurgery, also called neurosurgery for mental disorder , is the neurosurgical treatment of mental disorder. Psychosurgery has always been a controversial medical field. The modern history of psychosurgery begins in the 1880s under the Swiss psychiatrist Gottlieb Burckhardt...
or drug treatment, to remove the unpleasantness from pain without affecting its intensity, and cognitive processes such as placebo
Placebo
A placebo is a simulated or otherwise medically ineffectual treatment for a disease or other medical condition intended to deceive the recipient...
and hypnotic suggestion can temporarily reduce pain's unpleasantness but leave its intensity unchanged. Some drug therapies and other interventions can remove both the sensation of pain and its unpleasantness, and certain emotional states, such as the excitement of sport or war, can produce the same effect.
Pain makes complex thought more difficult: it impairs attention control, working memory
Working memory
Working memory has been defined as the system which actively holds information in the mind to do verbal and nonverbal tasks such as reasoning and comprehension, and to make it available for further information processing...
, mental flexibility
Cognitive flexibility
Cognitive flexibility is the term used to describe one of the executive functions; a function which is an important component of human behavior; the ability to switch behavioral response according to the context of the situation...
, problem solving, and information processing speed
Mental chronometry
Mental chronometry is the use of response time in perceptual-motor tasks to infer the content, duration, and temporal sequencing of cognitive operations....
, and it is associated with increased depression
Depression (mood)
Depression is a state of low mood and aversion to activity that can affect a person's thoughts, behaviour, feelings and physical well-being. Depressed people may feel sad, anxious, empty, hopeless, helpless, worthless, guilty, irritable, or restless...
, anxiety, fear, and anger. Cancer pain is classed as acute (usually caused by medical investigation or treatment) or chronic
Chronic pain
Chronic pain has several different meanings in medicine. Traditionally, the distinction between acute and chronic pain has relied upon an arbitrary interval of time from onset; the two most commonly used markers being 3 months and 6 months since the initiation of pain, though some theorists and...
. About 75% of patients with chronic cancer pain have pain caused by the cancer itself. In most of the remainder, pain is the result of treatment.
Infection
Infection of a tumor or its surrounding tissue can cause rapidly escalating pain, but is sometimes overlooked as a possible cause of pain. One study found infection was the cause of pain in four percent of nearly 300 cancer patients referred for pain relief. Another report described seven patients with large ulcerated and necrotic tumors of the head and neck, with erythemaErythema
Erythema is redness of the skin, caused by hyperemia of the capillaries in the lower layers of the skin. It occurs with any skin injury, infection, or inflammation...
, swelling, and hardening or thickening of the surrounding tissue, whose previously well-controlled pain escalated significantly over several days. Antibiotic treatment produced pain relief in all patients within three days.
Nervous system
Brain tissue itself contains no nociceptorNociceptor
A nociceptor is a sensory receptor that responds to potentially damaging stimuli by sending nerve signals to the spinal cord and brain. This process, called nociception, usually causes the perception of pain.-History:...
s; brain tumors cause pain by pressing on blood vessels or the membrane
Meninges
The meninges is the system of membranes which envelopes the central nervous system. The meninges consist of three layers: the dura mater, the arachnoid mater, and the pia mater. The primary function of the meninges and of the cerebrospinal fluid is to protect the central nervous system.-Dura...
that encapsulates the brain, or indirectly by causing edema
Edema
Edema or oedema ; both words from the Greek , oídēma "swelling"), formerly known as dropsy or hydropsy, is an abnormal accumulation of fluid beneath the skin or in one or more cavities of the body that produces swelling...
which may compress pain-sensitive tissue.
Ten percent of patients with disseminated cancer develop meningeal carcinomatosis
Meningeal carcinomatosis
Meningeal carcinomatosis is a condition in which a solid tumor diffusely spreads to the leptomeninges. Lung tumors, breast tumors, and malignant melanoma comprise the majority of solid tumors spreading to the leptomeninges.-Causes:...
, where metastatic seedlings develop in the meninges
Meninges
The meninges is the system of membranes which envelopes the central nervous system. The meninges consist of three layers: the dura mater, the arachnoid mater, and the pia mater. The primary function of the meninges and of the cerebrospinal fluid is to protect the central nervous system.-Dura...
of both brain and spinal cord, with possible invasion of the spinal cord or brain. Melanoma
Melanoma
Melanoma is a malignant tumor of melanocytes. Melanocytes are cells that produce the dark pigment, melanin, which is responsible for the color of skin. They predominantly occur in skin, but are also found in other parts of the body, including the bowel and the eye...
and breast
Breast cancer
Breast cancer is cancer originating from breast tissue, most commonly from the inner lining of milk ducts or the lobules that supply the ducts with milk. Cancers originating from ducts are known as ductal carcinomas; those originating from lobules are known as lobular carcinomas...
and lung cancer
Lung cancer
Lung cancer is a disease characterized by uncontrolled cell growth in tissues of the lung. If left untreated, this growth can spread beyond the lung in a process called metastasis into nearby tissue and, eventually, into other parts of the body. Most cancers that start in lung, known as primary...
account for 90 percent of such cases. Headache (often severe and possibly associated with nausea, vomiting, photophobia
Photophobia
Photophobia is a symptom of abnormal intolerance to visual perception of light. As a medical symptom photophobia is not a morbid fear or phobia, but an experience of discomfort or pain to the eyes due to light exposure or by presence of actual physical photosensitivity of the eyes, though the term...
and neck rigidity) and back pain are frequently the first symptoms. Paresthesia
Paresthesia
Paresthesia , spelled "paraesthesia" in British English, is a sensation of tingling, burning, pricking, or numbness of a person's skin with no apparent long-term physical effect. It is more generally known as the feeling of "pins and needles" or of a limb "falling asleep"...
, bowel or bladder dysfunction and lower motor neuron weakness are common features.

Pedicle of vertebral arch
The pedicles are two short, thick processes, which project dorsally, one on either side, from the superior part of the vertebral body at the junction of its posterior and lateral surfaces. They connect the body of the spinal vertebra to the arch...
(fig. 1) due to metastasis, sometimes involving collapse of the vertebral body. Occasionally compression is caused by nonvertebral metastasis adjacent to the spinal cord. Compression of a spinal nerve root (fig. 3) produces radicular pain
Radicular pain
Radicular pain, or radiculitis, is pain "radiated" along the dermatome of a nerve due to inflammation or other irritation of the nerve root at its connection to the spinal column...
, and compression of the long tracts of the cord itself produces funicular pain. Seventy percent of cases involve the thoracic, 20 percent the lumbar, and 10 percent the cervical spine; and about 20 percent of cases involve multiple sites of compression. The nature of the pain depends on the location of the compression.
Between one and five percent of cancer patients suffer peripheral neuropathy
Peripheral neuropathy
Peripheral neuropathy is the term for damage to nerves of the peripheral nervous system, which may be caused either by diseases of or trauma to the nerve or the side-effects of systemic illness....
due to infiltration or compression of a peripheral nerve
Peripheral nervous system
The peripheral nervous system consists of the nerves and ganglia outside of the brain and spinal cord. The main function of the PNS is to connect the central nervous system to the limbs and organs. Unlike the CNS, the PNS is not protected by the bone of spine and skull, or by the blood–brain...
by a primary tumor. Small cell lung cancer and, less often, cancer of the breast, colon or ovary may produce inflammation of the dorsal root ganglia
Dorsal root ganglion
In anatomy and neuroscience, a dorsal root ganglion is a nodule on a dorsal root that contains cell bodies of neurons in afferent spinal nerves.-Unique unipolar structure:...
(fig. 3), precipitating burning, tingling pain in the extremities, with occasional "lightening" or lancenating pains.
Brachial plexopathy is a common product of Pancoast tumor
Pancoast tumor
A Pancoast tumor, also called a pulmonary sulcus tumor or superior sulcus tumor, is a tumor of the pulmonary apex. It is a type of lung cancer defined primarily by its location situated at the top end of either the right or left lung. It typically spreads to nearby tissues such as the ribs and...
, lymphoma and breast cancer, and can produce severe burning dysesthesic
Dysesthesia
Dysesthesia comes from the Greek word "dys", meaning "not-normal" and "aesthesis", which means "sensation" . It is defined as an unpleasant, abnormal sense of touch, and it may be, or not be, considered as a kind of pain...
pain on the back of the hand, and cramping, crushing forearm pain.
Bone
Invasion of bone by cancer is the most common source of cancer pain. About 70 percent of breast and prostate cancer patients, and 40 percent of those with lung, kidney and thyroidThyroid
The thyroid gland or simply, the thyroid , in vertebrate anatomy, is one of the largest endocrine glands. The thyroid gland is found in the neck, below the thyroid cartilage...
cancers develop bone metastases. It is commonly felt as tenderness, with constant background pain and instances of spontaneous or movement-related exacerbation, and is frequently described as severe. Tumors in the marrow instigate a vigorous immune response which enhances pain sensitivity, and they release chemicals that stimulate nociceptors. As they grow, tumors compress, infiltrate, cut off blood supply to, or consume
Proteolysis
Proteolysis is the directed degradation of proteins by cellular enzymes called proteases or by intramolecular digestion.-Purposes:Proteolysis is used by the cell for several purposes...
body tissues, which can cause nociceptive or neuropathic pain.
Rib fractures, common in breast, prostate and other cancers with rib metastases, can cause brief severe pain on twisting the trunk, coughing, laughing, breathing deeply or moving between sitting and lying.
The base of the skull may be affected by metastases from cancer of the bronchus
Bronchus
A bronchus is a passage of airway in the respiratory tract that conducts air into the lungs. The bronchus branches into smaller tubes, which in turn become bronchioles....
, breast or prostate, or cancer may spread directly to this area from the nasopharynx
Nasopharynx
The nasopharynx is the uppermost part of the pharynx. It extends from the base of the skull to the upper surface of the soft palate; it differs from the oral and laryngeal parts of the pharynx in that its cavity always remains patent .-Lateral:On its lateral wall is the pharyngeal ostium of the...
, and this may cause headache, facial paresthesia
Paresthesia
Paresthesia , spelled "paraesthesia" in British English, is a sensation of tingling, burning, pricking, or numbness of a person's skin with no apparent long-term physical effect. It is more generally known as the feeling of "pins and needles" or of a limb "falling asleep"...
, dysesthesia
Dysesthesia
Dysesthesia comes from the Greek word "dys", meaning "not-normal" and "aesthesis", which means "sensation" . It is defined as an unpleasant, abnormal sense of touch, and it may be, or not be, considered as a kind of pain...
or pain, or cranial nerve dysfunction – the exact symptoms depending on the cranial nerves impacted.
Pelvis
Pain produced by cancer within the pelvis varies according to the cause, but it frequently radiates diffusely to the upper thigh, and may referReferred pain
Referred pain is pain perceived at a location other than the site of the painful stimulus. An example is the case of ischemia brought on by a myocardial infarction , where pain is often felt in the neck, shoulders, and back rather than in the chest, the site of the injury...
to the lumbar
Lumbar
In tetrapod anatomy, lumbar is an adjective that means of or pertaining to the abdominal segment of the torso, between the diaphragm and the sacrum ...
region. Lumbosacral plexopathy is often caused by recurrence of cancer in the presacral space
Presacral space
In human anatomy, the presacral space is inside the pelvis, behind the rectum and in front of the coccyx and sacrum. Normally it is empty, or it contains a pocket of fat.It is usually covered by sigmoid colon.-Clinical significance:...
, and may refer to the external genitalia or perineum
Perineum
In human anatomy, the perineum is a region of the body including the perineal body and surrounding structures...
rather than the legs. Local recurrence of cancer attached to the side of the pelvic wall may cause pain in one of the iliac fossa
Iliac fossa
The iliac fossa is a large, smooth, concave surface located on the internal surface of the ilium...
e. Pain on walking that confines the patient to bed indicates possible cancer adherence to or invasion of the iliacus muscle
Iliacus muscle
The iliacus is a flat, triangular muscle which fills the iliac fossa.- Course :The iliacus arises from the iliac fossa on the interior side of the hip bone, and also from the region of the anterior inferior iliac spine...
. Pain in the hypogastrium
Hypogastrium
The hypogastrium is an area of the human abdomen located below the navel. The pubis bone constitutes its lower limit....
(between the navel and pubic bone
Pubis (bone)
In vertebrates, the pubic bone is the ventral and anterior of the three principal bones composing either half of the pelvis.It is covered by a layer of fat, which is covered by the mons pubis....
) is often found in cancers of the uterus and bladder, and sometimes in colorectal cancer especially if infiltrating or attached to either uterus or bladder.
Visceral
VisceralViscus
In anatomy, a viscus is an internal organ, and viscera is the plural form. The viscera, when removed from a butchered animal, are known collectively as offal...
pain is diffuse and difficult to locate, and is often referred
Referred pain
Referred pain is pain perceived at a location other than the site of the painful stimulus. An example is the case of ischemia brought on by a myocardial infarction , where pain is often felt in the neck, shoulders, and back rather than in the chest, the site of the injury...
to more distant, usually superficial, sites.
A tumor can expand the size of the liver several times, and consequent stretching of its capsule can cause aching pain in the right hypochondrium
Hypochondrium
The hypochondrium is the upper part of the abdomen dorsal to the lowest ribs of the thorax. The word derives from the Greek term ὑποχονδρος hupochondros, meaning abdomen, or literally under cartilage.The liver is found in the right hypochondrium....
. Other causes of pain in enlarged liver
Hepatomegaly
Hepatomegaly is the condition of having an enlarged liver. It is a nonspecific medical sign having many causes, which can broadly be broken down into infection, direct toxicity, hepatic tumours, or metabolic disorder. Often, hepatomegaly will present as an abdominal mass...
are traction of the supporting ligaments when standing or walking, internal bleeding of the liver, the liver pressing against the rib cage or pinching the wall of the abdomen, and straining the lumbar spine. In some postures the liver may pinch the parietal peritoneum
Peritoneum
The peritoneum is the serous membrane that forms the lining of the abdominal cavity or the coelom — it covers most of the intra-abdominal organs — in amniotes and some invertebrates...
against the lower rib cage, producing sharp, transitory pain, relieved by changing position. The tumor may also infiltrate the liver's capsule, causing dull, and sometimes stabbing pain.
Cancer of the kidneys and spleen produces less pain than that caused by liver tumor – kidney tumors eliciting pain only once the organ has been almost totally destroyed and the cancer has invaded the surrounding tissue or adjacent pelvis. Pressure on the kidney or ureter
Ureter
In human anatomy, the ureters are muscular tubes that propel urine from the kidneys to the urinary bladder. In the adult, the ureters are usually long and ~3-4 mm in diameter....
from a tumor outside the kidney can cause extreme flank pain. Local recurrence of cancer after the removal of a kidney can cause pain in the lumbar back, or L1
Lumbar spinal nerve 1
The lumbar spinal nerve 1 is a spinal nerve of the lumbar segment..It originates from the spinal column from below the lumbar vertebra 1 .The two terminal branches of this nerve is the iliohypogastric and the ilioinguinal nerves-Muscles:...
or L2
Lumbar spinal nerve 2
The lumbar spinal nerve 2 is a spinal nerve of the lumbar segment..It originates from the spinal column from below the lumbar vertebra 2 .-Muscles:...
spinal nerve pain in the groin or upper thigh, accompanied by weakness and numbness of the iliopsoas
Iliopsoas
-External links:*...
muscle, exacerbated by activity.
The pain of intestinal tumors may be the result of disturbed motility
Motility
Motility is a biological term which refers to the ability to move spontaneously and actively, consuming energy in the process. Most animals are motile but the term applies to single-celled and simple multicellular organisms, as well as to some mechanisms of fluid flow in multicellular organs, in...
, dilation, altered blood flow or ulceration. Malignant lymphomas of the gastrointestinal tract can produce large tumors with significant ulceration and bleeding. Inflammation of artery walls and tissue adjacent to nerves is common in tumors of abdominal and urogenital hollow organs.
Cancer in the bronchial tree is usually painless, but ear and facial pain on one side of the head has been reported in some patients. This is referred
Referred pain
Referred pain is pain perceived at a location other than the site of the painful stimulus. An example is the case of ischemia brought on by a myocardial infarction , where pain is often felt in the neck, shoulders, and back rather than in the chest, the site of the injury...
via the auricular branch of the vagus nerve.
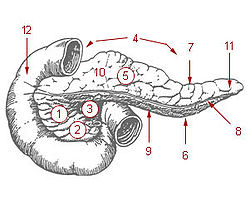
Tail of pancreas
The tail of the pancreas, located anatomically left near the hilum of the spleen, is not simply an anatomical distinction. The tail is the only part of the pancreas which contains Pancreatic Polypeptide cells, which are responsible for secreting pancreatic polypeptide to coordinate exocrine and...
experience pain, whereas 90 percent of those with cancer of the pancreatic head
Head of pancreas
The head of pancreas is a portion of the pancreas that is lodged within the curve of the duodenum, and is flattened anteriorly . The other parts of the pancreas are the body and the tail....
will, especially if the tumor is near the hepatopancreatic ampulla
Hepatopancreatic ampulla
The ampulla of Vater, also known as the ', is formed by the union of the pancreatic duct and the common bile duct. The ampulla is specifically located at the major duodenal papilla....
. The pain appears on the left or right upper abdomen, is constant, and increases in intensity over time. It is in some cases relieved by leaning forward and heightened by lying on the stomach. Back pain may be present and, if intense, may spread left and right. Back pain may be referred
Referred pain
Referred pain is pain perceived at a location other than the site of the painful stimulus. An example is the case of ischemia brought on by a myocardial infarction , where pain is often felt in the neck, shoulders, and back rather than in the chest, the site of the injury...
from the pancreas, or may indicate the cancer has penetrated paraspinal muscle, or entered the retroperitoneum
Retroperitoneum
The retroperitoneal space is the anatomical space in the abdominal cavity behind the peritoneum. It has no specific delineating anatomical structures...
and paraaortic lymph node
Paraaortic lymph node
The paraaortic lymph nodes are a group of lymph nodes that lie in front of the lumbar vertebral bodies near the aorta...
s
Pain of the rectum may be experienced even after the rectum has been surgically removed
Abdominoperineal resection
An abdominoperineal resection, formally known as abdominoperineal resection of the rectum and abdominoperineal excision of the rectum or simply abdominoperineal excision, is a surgery for rectal cancer or anal cancer...
. Local recurrence of rectal cancer may cause mild (described as "pressure") or strong pain on sitting; or pain on standing or walking (described as "dragging"). The latter may indicate a deeper recurrence involving attachment to muscle or fascia
Fascia
A fascia is a layer of fibrous tissue that permeates the human body. A fascia is a connective tissue that surrounds muscles, groups of muscles, blood vessels, and nerves, binding those structures together in much the same manner as plastic wrap can be used to hold the contents of sandwiches...
. A local tumor in the rectum or recurrence involving the presacral plexus may cause pain normally associated with an urgent need to defecate. This pain may, rarely, be phantom
Phantom pain
Phantom pain sensations are described as perceptions that an individual experiences relating to a limb or an organ that is not physically part of the body. Limb loss is a result of either removal by amputation or congenital limb deficiency . However, phantom limb sensations can also occur following...
after surgical removal of the rectum. Distressing, intense, stabbing, "red hot poker" pain is sometimes reported. Pain within a few weeks of surgical removal of the rectum is usually neuropathic
Neuropathic pain
Neuropathic pain results from lesions or diseases affecting the somatosensory system. It may be associated with abnormal sensations called dysesthesia, which occur spontaneously and allodynia that occurs in response to external stimuli. Neuropathic pain may have continuous and/or episodic ...
due to the surgery, and described in one study as spontaneous, intermittent, mild to moderate shooting and bursting, or tight and aching. Pain emerging after three months usually signals recurrence, and was described as deep, sharp, aching, intense, and continuous, made worse by sitting or pressure. In over half of patients with late-onset pain in the above study, pain was ameliorated by analgesic
Analgesic
An analgesic is any member of the group of drugs used to relieve pain . The word analgesic derives from Greek an- and algos ....
s.
Infection or cancer may irritate the trigone of the urinary bladder, causing spasm of the detrusor urinae muscle
Detrusor urinae muscle
The detrusor urinae muscle, also detrusor muscle, muscularis propria of the urinary bladder and muscularis propria, contracts when urinating to squeeze out urine. Otherwise, it remains relaxed to allow the bladder to fill...
(the muscle that squeezes urine from the urinary bladder
Urinary bladder
The urinary bladder is the organ that collects urine excreted by the kidneys before disposal by urination. A hollow muscular, and distensible organ, the bladder sits on the pelvic floor...
), resulting in deep pain above the pubic bone, possibly referred to the tip of the penis, lasting from a few minutes to half an hour.
Serous mucosa
CarcinosisCarcinosis
Carcinosis, or carcinomatosis, is a condition in which cancer has spread widely throughout the body, or, in some cases, to a relatively large region of the body.- External links :* entry in the public domain NCI Dictionary of Cancer Terms...
of the peritoneum
Peritoneum
The peritoneum is the serous membrane that forms the lining of the abdominal cavity or the coelom — it covers most of the intra-abdominal organs — in amniotes and some invertebrates...
may cause pain through pressure of the metastases on peripheral nerves, inflammation, or disordered visceral motility. Once a tumor has penetrated or perforated hollow viscera, acute inflammation of the peritoneum appears, inducing severe abdominal pain. Pleural carcinomatosis is normally painless.
Soft tissue
Invasion of soft tissue by a tumor can cause pain by inflammatory or mechanical stimulation of nociceptors, or destruction of mobile structures such as ligaments, tendons and skeletal muscles.Treatment-related
Potentially painful interventions in cancer treatment include immunotherapy which may produce joint or muscle pain; radiotherapy, which can cause skin reactions, enteritisEnteritis
In medicine, enteritis, from Greek words enteron and suffix -itis , refers to inflammation of the small intestine. It is most commonly caused by the ingestion of substances contaminated with pathogenic microorganisms. Symptoms include abdominal pain, cramping, diarrhea, dehydration and fever...
, radiation fibrosis, myelopathy
Myelopathy
Myelopathy refers to pathology of the spinal cord. When due to trauma, it is known as spinal cord injury. When inflammatory, it is known as myelitis. Disease that is vascular in nature is known as vascular myelopathy....
, osteoradionecrosis, neuropathy or plexopathy
Plexopathy
Plexopathy is a disorder affecting a network of nerves, blood vessels, or lymph vessels. The region of nerves it affects are at the brachial or lumbosacral plexus. Symptoms include pain, loss of motor control, and sensory deficits....
; chemotherapy, often associated with mucositis
Mucositis
Mucositis is the painful inflammation and ulceration of the mucous membranes lining the digestive tract, usually as an adverse effect of chemotherapy and radiotherapy treatment for cancer. Mucositis can occur anywhere along the gastrointestinal tract, but oral mucositis refers to the particular...
, joint pain
Arthralgia
Arthralgia literally means joint pain; it is a symptom of injury, infection, illnesses or an allergic reaction to medication....
, muscle pain
Myalgia
Myalgia means "muscle pain" and is a symptom of many diseases and disorders. The most common causes are the overuse or over-stretching of a muscle or group of muscles. Myalgia without a traumatic history is often due to viral infections...
, peripheral neuropathy
Peripheral neuropathy
Peripheral neuropathy is the term for damage to nerves of the peripheral nervous system, which may be caused either by diseases of or trauma to the nerve or the side-effects of systemic illness....
and abdominal pain due to diarrhea or constipation; hormone therapy, which sometimes causes pain flares; targeted therapies, such as trastuzumab and rituximab, which can cause muscle, joint or chest pain; angiogenesis inhibitors like bevacizumab, known to sometimes cause bone pain; surgery, which may produce postoperative pain, post-amputation pain or pelvic floor myalgia
Myalgia
Myalgia means "muscle pain" and is a symptom of many diseases and disorders. The most common causes are the overuse or over-stretching of a muscle or group of muscles. Myalgia without a traumatic history is often due to viral infections...
; and invasive investigations such as lumbar puncture
Lumbar puncture
A lumbar puncture is a diagnostic and at times therapeutic procedure that is performed in order to collect a sample of cerebrospinal fluid for biochemical, microbiological, and cytological analysis, or very rarely as a treatment to relieve increased intracranial pressure.-Indications:The...
, bone marrow biopsy
Bone marrow biopsy
Bone marrow examination refers to the pathologic analysis of samples of bone marrow obtained by bone marrow biopsy and bone marrow aspiration. Bone marrow examination is used in the diagnosis of a number of conditions, including leukemia, multiple myeloma, lymphoma, anemia, and pancytopenia...
, venipuncture
Venipuncture
In medicine, venepuncture, venopuncture or venipuncture is the process of obtaining intravenous access for the purpose of intravenous therapy or for blood sampling of venous blood. This procedure is performed by medical laboratory scientists, medical practitioners, some EMTs, paramedics,...
, paracentesis
Paracentesis
Paracentesis is a medical procedure involving needle drainage of fluid from a body cavity, most commonly the peritoneal cavity in the abdomen.A related procedure is thoracocentesis, which is needle drainage of the chest cavity...
, and thoracentesis
Thoracentesis
Thoracentesis , also known as thoracocentesis or pleural tap, is an invasive procedure to remove fluid or air from the pleural space for diagnostic or therapeutic purposes. A cannula, or hollow needle, is carefully introduced into the thorax, generally after administration of local anesthesia...
.
Chemotherapy
Chemotherapy may cause mucositisMucositis
Mucositis is the painful inflammation and ulceration of the mucous membranes lining the digestive tract, usually as an adverse effect of chemotherapy and radiotherapy treatment for cancer. Mucositis can occur anywhere along the gastrointestinal tract, but oral mucositis refers to the particular...
, muscle pain, joint pain, abdominal pain caused by diarrhea or constipation, and peripheral neuropathy
Peripheral neuropathy
Peripheral neuropathy is the term for damage to nerves of the peripheral nervous system, which may be caused either by diseases of or trauma to the nerve or the side-effects of systemic illness....
(pain and numbness in the hands, wrists, feet and ankles).
Chemotherapy-induced peripheral neuropathy
Some of the more common chemotherapy drugs, including vincristineVincristine
Vincristine , formally known as leurocristine, sometimes abbreviated "VCR", is a vinca alkaloid from the Catharanthus roseus , formerly Vinca rosea and hence its name. It is a mitotic inhibitor, and is used in cancer chemotherapy.-Mechanism:Tubulin is a structural protein that polymerizes to...
/vinblastine
Vinblastine
Vinblastine is an antimicrotubule drug used to treat certain kinds of cancer, including Hodgkin's lymphoma, non-small cell lung cancer, breast cancer, head and neck cancer, and testicular cancer. It is also used to treat Langerhan cell histiocytosis....
, aclitaxel/docetaxel, cisplatin
Cisplatin
Cisplatin, cisplatinum, or cis-diamminedichloroplatinum is a chemotherapy drug. It is used to treat various types of cancers, including sarcomas, some carcinomas , lymphomas, and germ cell tumors...
/oxaliplatin
Oxaliplatin
Oxaliplatin is a coordination complex that is used in cancer chemotherapy. These platinum-based drugs are usually classified as alkylating agents, although they are not actually alkylating groups ....
/carboplatin
Carboplatin
Carboplatin, or cis-Diammineplatinum is a chemotherapy drug used against some forms of cancer...
, thalidomide
Thalidomide
Thalidomide was introduced as a sedative drug in the late 1950s that was typically used to cure morning sickness. In 1961, it was withdrawn due to teratogenicity and neuropathy. There is now a growing clinical interest in thalidomide, and it is introduced as an immunomodulatory agent used...
, and bortezomib
Bortezomib
Bortezomib is the first therapeutic proteasome inhibitor to be tested in humans. It is approved in the U.S. for treating relapsed multiple myeloma and mantle cell lymphoma...
, can cause chemotherapy-induced peripheral neuropathy (CIPN), experienced as tingling numbness, intense pain, and hypersensitivity to cold in a glove and sock pattern. CIPN often follows the first chemotherapy dose and increases in severity as treatment continues, but this progressive degeneration usually halts at completion of treatment. The platinum-based drugs such as oxaliplatin and cisplatin are the exception; with these drugs, sensation may continue to deteriorate for several months after the end of treatment. Some CIPN appears to be irreversible.
Pain can often be helped with drug treatment but the numbness is usually resistant to treatment.
CIPN disrupts leisure, work and family relations, and the pain of CIPN is often accompanied by sleep and mood disturbance, fatigue and functional difficulties. A 2007 American study found that most patients did not recall being told to expect CIPN, and doctors monitoring the condition rarely asked how it affects daily living but focused on practical effects such as dexterity and gait.
It is not known what causes the condition, but microtubule
Microtubule
Microtubules are a component of the cytoskeleton. These rope-like polymers of tubulin can grow as long as 25 micrometers and are highly dynamic. The outer diameter of microtubule is about 25 nm. Microtubules are important for maintaining cell structure, providing platforms for intracellular...
and mitochondrial damage, and leaky blood vessels near nerve cells are some of the possibilities being explored. It is unknown what percentage of patients are affected.
As possible preventative interventions, the American National Cancer Institute
National Cancer Institute
The National Cancer Institute is part of the National Institutes of Health , which is one of 11 agencies that are part of the U.S. Department of Health and Human Services. The NCI coordinates the U.S...
Symptom Management and Health-related Quality of Life Steering Committee recommends continued investigation of glutathione
Glutathione
Glutathione is a tripeptide that contains an unusual peptide linkage between the amine group of cysteine and the carboxyl group of the glutamate side-chain...
, and intravenous calcium and magnesium, which have shown early promise in limited human trials; acetyl-L-carnitine, which was effective in animal models and on diabetes and HIV patients; and the anti-oxidant alpha-lipoic acid.
Mucositis
Cancer drugs can cause changes in the biochemistry of mucous membranes resulting in intense pain in the mouth, throat, nasal passages, and gastrointestinal tract, making talking, drinking, or eating difficult or impossible.Muscle and joint pain
Withdrawal of steroid medication can cause joint pain and diffuse muscle pain accompanied by fatigue; these symptoms resolve with recommencement of steroid therapy. Chronic steroid therapy can result in aseptic necrosis of the humoral or femoral head, resulting in shoulder or knee pain described as dull and aching, and reduced movement in or inability to use arm or hip. Aromatase inhibitors can cause diffuse muscle and joint pain and stiffness, and may increase the likelihood of osteoporosis and consequent fractures.Radiotherapy
Radiotherapy may affect the connective tissue surrounding peripheral nerves, and may damage or kill white or gray matter in the brain or spinal cord.Fibrosis around the brachial or lumbosacral plexus
Radiotherapy may produce excessive growth (fibrosisFibrosis
Fibrosis is the formation of excess fibrous connective tissue in an organ or tissue in a reparative or reactive process. This is as opposed to formation of fibrous tissue as a normal constituent of an organ or tissue...
) of the fibrous tissue enveloping the brachial
Brachial plexus
The brachial plexus is a network of nerve fibers, running from the spine, formed by the ventral rami of the lower four cervical and first thoracic nerve roots...
or lumbosacral
Lumbosacral plexus
The anterior divisions of the lumbar nerves, sacral nerves, and coccygeal nerve form the lumbosacral plexus, the first lumbar nerve being frequently joined by a branch from the twelfth thoracic. For descriptive purposes this plexus is usually divided into three parts:* lumbar plexus* sacral plexus*...
plexus, which can result in damage to the nerves over time (6 months to 20 years). This nerve damage can cause numbness, "pins and needles
Paresthesia
Paresthesia , spelled "paraesthesia" in British English, is a sensation of tingling, burning, pricking, or numbness of a person's skin with no apparent long-term physical effect. It is more generally known as the feeling of "pins and needles" or of a limb "falling asleep"...
" or unpleasant sensation
Dysesthesia
Dysesthesia comes from the Greek word "dys", meaning "not-normal" and "aesthesis", which means "sensation" . It is defined as an unpleasant, abnormal sense of touch, and it may be, or not be, considered as a kind of pain...
and weakness in the affected limb. If pain develops, it is described as diffuse, severe, burning pain, increasing over time, in part or all of the affected limb.
Spinal cord damage
If radiotherapy includes the spinal cord, changes may occur which do not become apparent until some time after treatment. "Early delayed radiation-induced myelopathyMyelopathy
Myelopathy refers to pathology of the spinal cord. When due to trauma, it is known as spinal cord injury. When inflammatory, it is known as myelitis. Disease that is vascular in nature is known as vascular myelopathy....
" can manifest from six weeks to six months after treatment; the usual symptom is a Lhermitte sign ("a brief, unpleasant sensation of numbness, tingling and often electric-like discharge going from the neck to the spine and extremities, triggered by neck flexion"), and is usually followed by improvement two to nine months after onset, though in some cases symptoms persist for a long time. "Late delayed radiation-induced myelopathy" may occur six months to ten years after treatment. The typical presentation is Brown-Séquard syndrome
Brown-Séquard syndrome
Brown-Séquard syndrome, also known as Brown-Séquard's hemiplegia and Brown-Séquard's paralysis, is a loss of sensation and motor function that is caused by the lateral hemisection of the spinal cord...
(a motor deficit and numbness to touch and vibration on one side of the body and loss of pain and temperature sensation on the other). Onset may be sudden but is usually progressive. Some patients improve and others deteriorate.
Management
Cancer pain treatment is directed toward relieving pain with minimal adverse treatment effects, allowing the patient a good quality of lifeQuality of life
The term quality of life is used to evaluate the general well-being of individuals and societies. The term is used in a wide range of contexts, including the fields of international development, healthcare, and politics. Quality of life should not be confused with the concept of standard of...
and level of function and a relatively painless death. Though 80–90% of cancer pain can be eliminated or well controlled, nearly half of all patients throughout the world with cancer pain receive less than optimal care.
Barriers to pain management
Despite the publication and ready availability of simple and effective evidence-based pain management guidelines by the World Health OrganizationWorld Health Organization
The World Health Organization is a specialized agency of the United Nations that acts as a coordinating authority on international public health. Established on 7 April 1948, with headquarters in Geneva, Switzerland, the agency inherited the mandate and resources of its predecessor, the Health...
(WHO) and others,
doctors and nurses frequently lack understanding of key aspects of pain management including assessment, dosing, tolerance and addiction, and many do not know that pain elimination is possible in most cases, that this should be offered wherever possible, and where complete elimination of suffering is not achievable due to intolerable drug side effects, the maximum tolerable dose should be offered.
Systemic problems in the delivery of pain management include failure in the clinical setting to refer patients for pain management, inadequate reimbursement for pain management, lack of stocks of pain medicines in poorer areas, out-dated government policy on cancer pain management, and legal restraints on prescription of opioid medication.
Patients may not report pain due to a belief that pain is inevitable, fear of side effects of treatment, fear of developing addiction or tolerance to opioids, fear of distracting the doctor from treating the illness, or fear of masking a symptom important for monitoring progress of the disease. Patients may be reluctant to take adequate pain medicine because they are unaware of the prognosis
Prognosis
Prognosis is a medical term to describe the likely outcome of an illness.When applied to large statistical populations, prognostic estimates can be very accurate: for example the statement "45% of patients with severe septic shock will die within 28 days" can be made with some confidence, because...
or unwilling to accept the diagnosis. Patient failure to report pain or misguided reluctance to take pain medicine can be overcome by sensitive coaching.
Cancer is a dynamic process, and pain interventions need to reflect this. Several different treatment modalities may be required over time, as the disease progresses. Pain managers should clearly explain to the patient the cause of the pain and the various treatment possibilities, and should consider, as well as drug therapy, directly modifying the underlying disease, raising the pain threshold, interrupting, destroying or stimulating pain pathways, and suggesting lifestyle modification. The relief of psychological, social and spiritual distress is a key element in effective pain management.
Drugs
The WHO guidelines recommend prompt oral administration of drugs when pain occurs, starting, if the patient is not in severe pain, with non-opioid drugs such as paracetamolParacetamol
Paracetamol INN , or acetaminophen USAN , is a widely used over-the-counter analgesic and antipyretic . It is commonly used for the relief of headaches and other minor aches and pains and is a major ingredient in numerous cold and flu remedies...
, dipyrone, non-steroidal anti-inflammatory drug
Non-steroidal anti-inflammatory drug
Nonsteroidal anti-inflammatory drugs, usually abbreviated to NSAIDs or NAIDs, but also referred to as nonsteroidal anti-inflammatory agents/analgesics or nonsteroidal Anti-inflammatory medicines , are drugs with analgesic and antipyretic effects and which have, in higher doses, anti-inflammatory...
s or COX-2 inhibitor
COX-2 inhibitor
COX-2 selective inhibitor is a form of non-steroidal anti-inflammatory drug that directly targets COX-2, an enzyme responsible for inflammation and pain. Targeting selectivity for COX-2 reduces the risk of peptic ulceration, and is the main feature of celecoxib, rofecoxib and other members of this...
s. Then, if complete pain relief is not achieved or disease progression necessitates more aggressive treatment, mild opioids such as codeine phosphate, dextropropoxyphene
Dextropropoxyphene
Dextropropoxyphene, manufactured by Eli Lilly and Company, is an analgesic in the opioid category. It is intended to treat mild pain and has, in addition, anti-tussive and local anesthetic effects. It has been taken off the market in Europe and the US due to concerns of fatal overdoses and...
, dihydrocodeine
Dihydrocodeine
Dihydrocodeine, also called DHC, Drocode, Paracodeine and Parzone and known by the brand names of Synalgos DC, Panlor DC, Panlor SS, Contugesic, New Bron Solution-ACE, Huscode, Drocode, Paracodin, Codidol, Didor Continus, Dicogesic, Codhydrine, Dekacodin, DH-Codeine,...
or tramadol
Tramadol
Tramadol hydrochloride is a centrally acting synthetic opioid analgesic used in treating moderate pain. The drug has a wide range of applications, including treatment for restless legs syndrome and fibromyalgia...
are added to the existing non-opioid regime. If this is or becomes insufficient, mild opioids are replaced by stronger opioids such as morphine, while continuing the non-opioid therapy, escalating opioid dose until the patient is pain-free or the maximum possible relief without intolerable side effects has been achieved. If the initial presentation is severe cancer pain, this stepping process should be skipped and a strong opioid should be started immediately in combination with a non-opioid analgesic.
The usefulness of the second step is being debated in the clinical and research communities. Some are challenging the pharmacological validity of the step and, pointing to the higher toxicity and low efficacy of mild opioids, argue that they, with the possible exception of tramadol due to its unique action, could be replaced by smaller doses of strong opioids.
Antiemetic
Antiemetic
An antiemetic is a drug that is effective against vomiting and nausea. Antiemetics are typically used to treat motion sickness and the side effects of opioid analgesics, general anaesthetics, and chemotherapy directed against cancer....
and laxative
Laxative
Laxatives are foods, compounds, or drugs taken to induce bowel movements or to loosen the stool, most often taken to treat constipation. Certain stimulant, lubricant, and saline laxatives are used to evacuate the colon for rectal and/or bowel examinations, and may be supplemented by enemas under...
treatment should be commenced concurrently with strong opioids, to counteract the usual nausea and constipation. Nausea normally resolves after two or three weeks of treatment but laxatives will need to be aggressively maintained. More than half of patients with advanced cancer and pain will need strong opioids, and these in combination with non-opioids can produce acceptable analgesia in 70–90 percent of cases. Sedation and cognitive impairment usually occur with the initial dose or a significant increase in dosage of a strong opioid, but improve after a week of consistent dosage.
Analgesics should not be taken "on demand" but "by the clock" (every 3–6 hours), with each dose delivered before the preceding dose has worn off, in doses sufficiently high to ensure continuous pain relief. Patients taking slow-release morphine should also be provided with immediate-release ("rescue") morphine to use as necessary, for pain spikes that are not suppressed by their regular medication.
Oral analgesia is the cheapest, simplest and most acceptable mode of delivery. Other delivery routes such as sublingual, topical, parenteral, rectal or spinal should be considered if the need is urgent, or in case of vomiting, impaired swallow, obstruction of the gastrointestinal tract, poor absorption or coma. Liver and kidney disease can affect the biological activity of analgesics. When such patients are treated with oral opioids they must be monitored for the possible need to reduce dose, extend dosing intervals, or switch to other opioids or other modes of delivery.
Not all pain yields completely to classic analgesics, and drugs that are not traditionally considered analgesics but which effect pain relief in certain cases, such as steroids or bisphosphonates, may be employed concurrently with analgesics at any stage. Tricyclic antidepressants, class I antiarrhythmics
Antiarrhythmic agent
Antiarrhythmic agents are a group of pharmaceuticals that are used to suppress abnormal rhythms of the heart , such as atrial fibrillation, atrial flutter, ventricular tachycardia, and ventricular fibrillation....
, or anticonvulsants are the drugs of choice for neuropathic pain. Up to 90 percent of patients at death are using such "adjuvant
Adjuvant
An adjuvant is a pharmacological or immunological agent that modifies the effect of other agents, such as a drug or vaccine, while having few if any direct effects when given by itself...
s". Many adjuvants carry a significant risk of serious complications.
Anxiety reduction can reduce the unpleasantness of pain but is least effective for moderate or severe pain. Since anxiolytic
Anxiolytic
An anxiolytic is a drug used for the treatment of anxiety, and its related psychological and physical symptoms...
s such as benzodiazepines, psychotropic drugs and major tranquilizer
Tranquilizer
A tranquilizer, or tranquilliser , is a drug that induces tranquility in an individual.The term "tranquilizer" is imprecise, and is usually qualified, or replaced with more precise terms:...
s add to sedation, they should only be used to address anxiety
Anxiety
Anxiety is a psychological and physiological state characterized by somatic, emotional, cognitive, and behavioral components. The root meaning of the word anxiety is 'to vex or trouble'; in either presence or absence of psychological stress, anxiety can create feelings of fear, worry, uneasiness,...
, depression
Depression (mood)
Depression is a state of low mood and aversion to activity that can affect a person's thoughts, behaviour, feelings and physical well-being. Depressed people may feel sad, anxious, empty, hopeless, helpless, worthless, guilty, irritable, or restless...
, disturbed sleep or muscle spasm.
Interventional
If the analgesic and adjuvant regimen recommended above does not adequately relieve pain, additional modes of intervention are available.Radiation
Radiotherapy is used when drug treatment is failing to control the pain of a growing tumor, such as in bone metastisis (most commonly), penetration of soft tissue or compression of sensory nerves. Often, low doses are adequate to produce analgesia, thought to be due to reduction in pressure or, possibly, interference with the tumor's production of pain-causing chemicals. Radiopharmaceuticals that target specific tumors have been used to treat the pain of metastatic illnesses. Relief may occur within a week of treatment and may last from two to four months.Nerve blocks
Neurolysis is the injury of a nerve. Chemicals, laser, freezing or heating may be used to injure a sensory nerve and so produce degeneration of the nerve's fibers and the fibers' myelin sheaths, and temporary interference with the transmission of pain signals. In this procedure, the protective casing around the myelin sheath, the basal lamina, is preserved so that, when each damaged fiber regrows, it travels within its basal lamina and connects with the correct loose end, and function may be restored. Surgical cutting of a nerve severs the basal laminae, and without these tubes to channel the regrowing fibers to their lost connections, a neuromata may develop, causing deafferentation pain. This is why neurolysis is preferred over surgically blocking peripheral nerves. A brief "rehearsal" block using local anesthesia should be tried before the actual neurolytic block, to determine efficacy and detect any possible side effects." The aim of this treatment is pain elimination, or the reduction of pain to the point where opioids may be effective. Though neurolysis lacks long-term outcome studies and evidence-based guidelines for its use, for patients with progressive cancer and otherwise incurable pain, it can play an essential role.Targets for neurolytic block include the celiac plexus
Celiac plexus
The celiac plexus or coeliac plexus, also known as the solar plexus, is a complex network of nerves located in the abdomen, where the celiac trunk, superior mesenteric artery, and renal arteries branch from the abdominal aorta...
, most commonly for cancer of the gastrointestinal tract up to the transverse colon, and pancreatic cancer, but also for stomach cancer, gall bladder cancer, adrenal mass, common bile duct cancer, chronic pancreatitis and active intermittent porphyria
Porphyria
Porphyrias are a group of inherited or acquired disorders of certain enzymes in the heme bio-synthetic pathway . They are broadly classified as acute porphyrias and cutaneous porphyrias, based on the site of the overproduction and accumulation of the porphyrins...
; the splanchnic nerve, for retroperitoneal pain, and similar conditions to those addressed by the celiac plexus block but, because of its higher rate of complications, used only if the celiac plexus block is not producing adequate relief; hypogastric plexus
Hypogastric plexus
Hypogastric plexus can refer to:* Superior hypogastric plexus* Inferior hypogastric plexus...
, "for cancer affecting the descending colon, sigmoid colon and rectum," as well as cancers of the bladder, prostatic urethra, prostate, seminal vesicles, testicles, uterus, ovary and vaginal fundus; ganglion impar
Ganglion impar
The pelvic portion of each sympathetic trunk is situated in front of the sacrum, medial to the anterior sacral foramina. It consists of four or five small sacral ganglia, connected together by interganglionic cords, and continuous above with the abdominal portion...
, for the perinium, vulva, anus, distal rectum, distal urethra, and distal third of the vagina; the stellate ganglion
Stellate ganglion
The stellate ganglion is a sympathetic ganglion formed by the fusion of the inferior cervical ganglion and the first thoracic ganglion...
, usually for head and neck cancer, or sympathetically mediated arm and hand pain; the intercostal nerves
Intercostal nerves
The intercostal nerves are the anterior divisions of the thoracic spinal nerves from T1 to T11.Each nerve is connected with the adjoining ganglion of the sympathetic trunk by a gray and a white ramus communicans...
, which serve the skin of the chest and abdomen; and a posterior root ganglion
Dorsal root ganglion
In anatomy and neuroscience, a dorsal root ganglion is a nodule on a dorsal root that contains cell bodies of neurons in afferent spinal nerves.-Unique unipolar structure:...
may be injured by targeting the root inside the subarachnoid cavity
Subarachnoid space
In the central nervous system, the subarachnoid cavity is the interval between the arachnoid membrane and pia mater....
(fig.3), most effective for pain in the chest or abdominal wall, but also used for other areas including arm/hand or leg/foot pain.
Intrathecal programmable pump
Delivery of an opioid such as morphineMorphine
Morphine is a potent opiate analgesic medication and is considered to be the prototypical opioid. It was first isolated in 1804 by Friedrich Sertürner, first distributed by same in 1817, and first commercially sold by Merck in 1827, which at the time was a single small chemists' shop. It was more...
, hydromorphone
Hydromorphone
Hydromorphone, a more common synonym for dihydromorphinone, commonly a hydrochloride is a very potent centrally-acting analgesic drug of the opioid class. It is a derivative of morphine, to be specific, a hydrogenated ketone thereof and, therefore, a semi-synthetic drug...
, fentanyl, sufentanyl and meperidine directly into the subarachnoid cavity (fig. 3) provides enhanced analgesia with reduced systemic side effects, and has reduced the level of pain in otherwise intractable cases. The anxiolytic clonidine
Clonidine
Clonidine is a sympatholytic medication used to treat medical conditions, such as high blood pressure, some pain conditions, ADHD and anxiety/panic disorder...
, or the nonopioid analgesic ziconotide, and local anesthetics such as bupivacaine
Bupivacaine
Bupivacaine is a local anaesthetic drug belonging to the amino amide group. AstraZeneca commonly markets it under various trade names, including Marcain, Marcaine, Sensorcaine and Vivacaine.-Indications:...
, ropivacaine
Ropivacaine
Ropivacaine is a local anaesthetic drug belonging to the amino amide group. The name ropivacaine refers to both the racemate and the marketed S-enantiomer...
or tetracaine
Tetracaine
Tetracaine is a potent local anesthetic of the ester group...
may also be infused along with the opioid.
Long-term epidural catheter
The outer layer of the sheath surrounding the spinal cord is called the dura materDura mater
The dura mater , or dura, is the outermost of the three layers of the meninges surrounding the brain and spinal cord. It is derived from Mesoderm. The other two meningeal layers are the pia mater and the arachnoid mater. The dura surrounds the brain and the spinal cord and is responsible for...
. Between this and the surrounding vertebrae is the epidural space
Epidural space
In the spine, the epidural space is the outermost part of the spinal canal. It is the space within the canal lying outside the dura mater...
, filled with connective tissue, fat and blood vessels, and crossed by the spinal nerve roots. A catheter
Catheter
In medicine, a catheter is a tube that can be inserted into a body cavity, duct, or vessel. Catheters thereby allow drainage, administration of fluids or gases, or access by surgical instruments. The process of inserting a catheter is catheterization...
may be inserted into this space for three to six months, to deliver anesthetics or analgesics. The line carrying the drug may be threaded under the skin to emerge at the front of the patient, a process called tunneling. This is recommended with long term use so as to reduce the chance of any infection at the exit site reaching the epidural space.
Spinal cord stimulation
Electrical stimulation of the dorsal columns of the spinal cord (fig. 4) can produce analgesia. First, the leads are implanted, guided by the patient's report and fluoroscopyFluoroscopy
Fluoroscopy is an imaging technique commonly used by physicians to obtain real-time moving images of the internal structures of a patient through the use of a fluoroscope. In its simplest form, a fluoroscope consists of an X-ray source and fluorescent screen between which a patient is placed...
, and the generator is worn externally for several days to assess efficacy. If pain is reduced by more than half, the therapy is deemed to be suitable. A small pocket is cut into the tissue beneath the skin of the upper buttocks, chest wall or abdomen and the leads are threaded under the skin from the stimulation site to the pocket, where they are attached to the snugly-fitting generator. It seems to be more helpful with neuropathic and ischemic pain than nociceptive pain, and is not often used in the treatment of cancer pain.
Deep brain stimulation
Electrical stimulation of structures deep within the brain – the periaqueductal grayPeriaqueductal gray
Periaqueductal gray is the gray matter located around the cerebral aqueduct within the tegmentum of the midbrain. It plays a role in the descending modulation of pain and in defensive behaviour...
and periventricular gray for nociceptive pain, and the internal capsule
Internal capsule
The internal capsule is an area of white matter in the brain that separates the caudate nucleus and the thalamus from the lenticular nucleus. The internal capsule contains both ascending and descending axons....
, ventral posterolateral nucleus
Ventral posterolateral nucleus
The ventral posterolateral nucleus is a nucleus of the thalamus. Together with the ventral posteromedial nucleus , VPI and VMpo, it constitutes the ventral posterior nucleus.-Input and output:...
and ventral posteromedial nucleus
Ventral posteromedial nucleus
-Inputs and outputs:It conveys information of the trigeminothalamic tract, from the solitary tract and the trigeminal nerve and projects to the postcentral gyrus....
for neuropathic pain – has produced impressive results with some patients but results vary and appropriate patient selection is important. One study of seventeen patients with intractable cancer pain found that thirteen were virtually pain free and only four required opioid analgesics on release from hospital after the intervention. Most ultimately did resort to opioids, usually in the last few weeks of life.
Hypophysectomy
HypophysectomyHypophysectomy
Hypophysectomy is the surgical removal of the hypophysis . It is most commonly performed to treat tumors, especially craniopharyngioma tumors. Sometimes it is used to treat Cushing's syndrome due to pituitary adenoma...
is the destruction of the pituitary gland
Pituitary gland
In vertebrate anatomy the pituitary gland, or hypophysis, is an endocrine gland about the size of a pea and weighing 0.5 g , in humans. It is a protrusion off the bottom of the hypothalamus at the base of the brain, and rests in a small, bony cavity covered by a dural fold...
, and has been used successfully on metastatic breast and prostate cancer pain.
Cutting or destruction of nervous tissue
Surgical cutting or destruction of peripheralPeripheral nervous system
The peripheral nervous system consists of the nerves and ganglia outside of the brain and spinal cord. The main function of the PNS is to connect the central nervous system to the limbs and organs. Unlike the CNS, the PNS is not protected by the bone of spine and skull, or by the blood–brain...
or central
Central nervous system
The central nervous system is the part of the nervous system that integrates the information that it receives from, and coordinates the activity of, all parts of the bodies of bilaterian animals—that is, all multicellular animals except sponges and radially symmetric animals such as jellyfish...
nervous tissue is now rarely used in the treatment of pain. Procedures include neurectomy, cordotomy, dorsal root entry zone lesioning, and cingulotomy.
Neurectomy
Neurectomy
Neurectomy is the surgical removal of a nerve or a section of a nerve. This procedure may be performed, for example, in cases of chronic pain where other treatments have failed. However the removal of the nerve can also cause negative effects, such as permanent numbness...
involves cutting a peripheral nerve, and is (rarely) used in patients with short life expectancy who are unsuitable for drug therapy due to ineffectiveness or intolerance. The dorsal (sensory) root
Dorsal root
In anatomy and neurology, the dorsal root is the afferentsensory root of a spinal nerve.At the distal end of the dorsal root is the dorsal root ganglion, which contains the neuron cell bodies of the nerve fibres conveyed by the root.If the dorsal root of a spinal nerve were severed it would lead...
or dorsal root ganglion
Dorsal root ganglion
In anatomy and neuroscience, a dorsal root ganglion is a nodule on a dorsal root that contains cell bodies of neurons in afferent spinal nerves.-Unique unipolar structure:...
may be usefully targeted (called rhizotomy
Rhizotomy
A rhizotomy is a term chiefly referring to a neurosurgical procedure that selectively severs problematic nerve roots in the spinal cord, most often to relieve the symptoms of neuromuscular conditions such as spastic diplegia and other forms of spastic cerebral palsy...
); with the dorsal root ganglion possibly the more effective target because some sensory fibers enter the spinal cord from the dorsal root ganglion via the ventral (motor) root
Ventral root
In anatomy and neurology, the ventral root is the efferent motor root of a spinal nerve.At its distal end, the ventral root joins with the dorsal root to form a mixed spinal nerve....
, and these would not be interrupted by dorsal root neurectomy. Because peripheral nerves often carry both sensory and motor fibers, motor impairment is a possible side effect of neurectomy. A common result of this procedure is "deafferentation pain" where, 6–9 months after surgery, the original pain returns at greater intensity.
Cordotomy
Cordotomy
Cordotomy is a surgical procedure that disables selected pain-conducting tracts in the spinal cord, in order to achieve loss of pain and temperature perception. This procedure is commonly performed on patients experiencing severe pain due to cancer or other diseases for which there is currently no...
involves cutting into the spinothalamic tract
Spinothalamic tract
The spinothalamic tract is a sensory pathway originating in the spinal cord. It transmits information to the thalamus about pain, temperature, itch and crude touch...
s, which run up the front/side (anterolateral) quadrant of the spinal cord, carrying heat and pain signals to the brain (fig. 4). Pancoast tumor pain has been effectively treated with dorsal root entry zone (DREZ) lesioning – damaging a region of the spinal cord where peripheral pain signals cross to spinal cord fibers – this is major surgery, carrying the risk of significant neurological side-effects. Cingulotomy involves cutting the fibers that carry signals directly from the cingulate gyrus to the entorhinal cortex
Entorhinal cortex
The entorhinal cortex is located in the medial temporal lobe and functions as a hub in a widespread network for memory and navigation. The EC is the main interface between the hippocampus and neocortex...
in the brain. It reduces the unpleasantness of pain without affecting its intensity, but may have cognitive
Cognition
In science, cognition refers to mental processes. These processes include attention, remembering, producing and understanding language, solving problems, and making decisions. Cognition is studied in various disciplines such as psychology, philosophy, linguistics, and computer science...
side-effects.
Ethical considerations
Doctors and nurses have an ethical obligation to ensure that when consent for pain treatment is withheld or given it is, wherever possible, withheld or given by a fully informed patient. Most importantly, patients must be appraised of serious risks and common side effects of pain treatment. What appears to be an obviously acceptable risk or harm to a professional may be unacceptable to the patient. For instance, patients who experience pain on movement may be willing to forgo strong opioids in order to enjoy alertness during pain-free periods, whereas others would choose round-the-clock sedation so as to remain pain-free. Well informed patients can work with their doctors and are more likely to achieve the optimum pain management regimen. The doctor should not insist on treatment if the patient rejects, and must not provide treatment the doctor believes is more harmful or riskier than the possible benefits can justify.Some, especially exhausted, terminally ill patients, may not wish to be involved in making pain management decisions, and delegate such choices to the professionals. The patient's participation is a right not an obligation, and though reduced patient involvement may result in less than optimal pain management, this choice should be respected.
As professionals become better informed about the interdependent relationship between physical, emotional, social and spiritual pain, and the demonstrated benefit to physical pain from alleviation of these other forms of suffering, they may be tempted to question the patient and family about personal relationships. Unless the patient has asked for such psychosocial intervention, or at least freely consented to such questioning, this would be an ethically unjustifiable intrusion into the patient's very personal affairs, analogous to providing drugs without the patient's informed consent.
A professional's obligation to alleviate suffering may occasionally come into conflict with the obligation to prolong life. If a terminally ill patient prefers to be free of pain, despite sedation and the risk of shortening life, they should be provided with their desired pain relief, at the cost of sedation and a possibly slightly shorter life. Where a patient is unable to be involved in this decision, the law and the medical profession in the United Kingdom allow the doctor to assume the patient would prefer to be pain-free, and provide adequate analgesia, even if this treatment may slightly hasten death. It is taken that the underlying cause of death in this case is the illness and not the necessary pain management.
A philosophical justification for this approach is the doctrine of double effect, where, to justify an act involving both a good and a bad effect, four conditions are necessary: the act must be good overall or morally neutral, the person acting must intend only the good effect with the bad effect as an unwanted side effect, the bad effect must not be the cause of the good effect, and the good effect must outweigh the bad. Just as an oncologist who intends to treat cancer may foresee but not intend nausea and other effects of chemotherapy, so a doctor treating suffering may foresee but not intend shortening life.
Epidemiology
The actual global prevalence of cancer pain is difficult to assess because systems for measuring patient pain vary widely, methods of determining prevalence differ from study to study, and there is uncertainty in defining cancer pain because it can be directly or indirectly caused by the cancer.A 2003 review comparing studies of patients at all stages of cancer yielded a mean prevalence of 48%, ranging from 38% to 100%. Studies of patients at all stages with primary cancer in the head and neck, genitourinary system, prostate or esophagus reported a mean pain prevalence of 70%. Evidence for prevalence of pain in newly diagnosed cancer is scarce. One study found pain in 38% of newly diagnosed cases, and another found 35% of new patients had experienced pain in the preceding two weeks, while a third reported that pain was an early symptom in 18%-49% of cases. Comparison of twenty seven studies of the prevalence of pain in advanced cancer found a weighted mean prevalence of 74%, with reported prevalence rates ranging from 53% to 100%. Metastatic cancer is associated with a higher prevalence of pain than nonmetastatic cancer but this may be related to the disease stage. About 33% of cancer survivors report chronic pain after treatment has been completed.

