
Pneumothorax
Encyclopedia
Pneumothorax is a collection of air or gas in the pleural cavity
of the chest between the lung
and the chest wall. It may occur spontaneously in people without chronic lung conditions ("primary") as well as in those with lung disease ("secondary"), and many pneumothoraces occur after physical trauma
to the chest, blast injury
, or as a complication of medical treatment
.
The symptoms of a pneumothorax are determined by the size of the air leak and the speed by which it occurs; they may include chest pain
in most cases and shortness of breath
in many. The diagnosis can be made by physical examination
in severe cases but usually requires a chest X-ray
or computed tomography (CT scan) in milder forms. In a small proportion, the pneumothorax leads to severe oxygen shortage
and low blood pressure
, progressing to cardiac arrest
unless treated; this situation is termed tension pneumothorax.
Small spontaneous pneumothoraces typically resolve by themselves and require no treatment, especially in those with no underlying lung disease. In larger pneumothoraces or when there are severe symptoms, the air may be aspirated with a syringe, or a one-way chest tube
is inserted to allow the air to escape. Occasionally, surgical measures are required, especially if tube drainage is unsuccessful or someone has repeated episodes. Various treatments, usually involving pleurodesis
(sticking the lung to the chest wall), may be used if there is a significant risk of repeated episodes of pneumothorax.
, are characteristically at a higher risk of PSP. It has been found that PSP occurs more commonly during changes in atmospheric pressure
and during exposure to loud music, and this explains to an extent why episodes of pneumothorax may happen in clusters.
Secondary spontaneous pneumothorax (SSP) occurs by definition in those with underlying lung diseases. The symptoms tend to be more severe, as the unaffected lung is generally not capable of replacing the loss of function from the affected side. Hypoxemia
(decreased blood oxygen levels) is usually present and may be observed as cyanosis
(blue discoloration of the lips and skin). Hypercapnia
(accumulation of carbon dioxide in the blood) is sometimes encountered; this may cause confusion
and coma
. Sudden breathlessness in someone with lung problems such as chronic obstructive pulmonary disease
and cystic fibrosis
may therefore prompt investigations for a possible pneumothorax. The size of the pneumothorax bears limited relationship to the symptoms experienced.
Traumatic pneumothorax occurs either because a hole in the chest wall, such as a stab wound
or gunshot wound
, allows air to enter the pleural space, or because of injury to the lung. It has been found to occur in half of all cases of injury to the chest, coming second after rib fracture
in the complications after chest trauma. The pneumothorax can be small (occult) in half of these cases, but they may enlarge if the person requires mechanical ventilation
and their presence is therefore still relevant. It is also often encountered in those already receiving mechanical ventilation.
Tension pneumothorax is defined differently by different sources, but is generally said to exist when there is severe hypoxia despite administration of oxygen, falling blood pressure
or confusion. This is a medical emergency
and may require immediate treatment without further investigations (see below). Tension pneumothorax may also occur in those receiving mechanical ventilation, in which case it may be difficult to spot as the person is typically sedated; it is often noted because of sudden deterioration.
may be diminished on the affected side, as air in the pleural space dampens sound. Percussion
of the chest may sound hyperresonant (higher pitched), and vocal resonance
and tactile fremitus
(both examining the conduction of voice by the lung) can be decreased.
Tension pneumothorax is characterized by rapid breathing
, cyanosis, falling blood pressure
(hypotension) and confusion. The affected side of the chest may be hyperexpanded and show decreased movement, with increased movement on the other side. In very severe cases, the respiratory rate falls sharply, with shock and coma
. Recent studies have shown that the development of tension features may not always be as rapid as previously thought. Particular clinical signs may also be less useful in the recognition of tension pneumothorax, such as the deviation of the trachea
(windpipe) to one side and the presence of raised jugular venous pressure
(distended neck veins).
, and a family history
of pneumothorax. The various suspected underlying mechanisms are discussed below.
Secondary spontaneous pneumothorax occurs in the setting of a variety of lung diseases. The most common is chronic obstructive pulmonary disease
which accounts for approximately 70% of cases. Known lung diseases that may increase the risk for pneumothorax are:
In children, additional causes include measles
, echinococcosis
, inhalation of a foreign body
, and particular congenital malformations (congenital cystic adenomatoid malformation
and congenital lobar emphysema).
A rare genetic disorder, Birt-Hogg-Dubé syndrome
, may cause spontaneous pneumothorax in families. It also causes skin lesions (fibrofolliculoma
s) and lung cysts, and carries an increased risk of kidney cancer. The lung cysts, which probably lead to increased risk of pneumothorax, tend to be in the lower lobes rather than the more common upper lobe cysts encountered in other conditions. Birt-Hogg-Dubé syndrome is caused by mutations in the FLCN gene (chromosome 17p11.2), which encodes a protein named folliculin
. FLCN mutations and lung lesions have also been identified in familial cases of pneumothorax where other features of Birt-Hogg-Dubé syndrome are absent.
and penetrating injuries
to the chest wall. It may be observed in those exposed to an explosive blast
, even if no direct injury to the chest has occurred. The most common mechanism is a cut to the pleura by a fractured rib
.
Medical procedures of the chest (iatrogenic
), such as the taking of biopsy
samples from lung tissue, inserting a central venous catheter
into one of the chest veins, may lead to injury to the lung and resultant pneumothorax. The administration of positive pressure ventilation, either mechanical ventilation
or non-invasive ventilation, may result in barotrauma
(pressure-related injury) leading to a pneumothorax.
 The thoracic cavity
The thoracic cavity
is the hollow space that contains the lungs. The lungs are physically connected at the hila
, where the airways and blood vessels enter the lung. They remain inflated inside the thoracic cavity because the pressure inside the pleural space (the space between the chest wall and the lung) is almost consistently negative throughout the respiratory cycle
, effectively sucking the lung to the chest wall. Both the lung and the chest wall are covered by a layer of cells known as the pleura (visceral and parietal pleura, respectively), and a small amount of serous fluid is typically present. The negative pressure normally does not allow air to enter the pleural space because there are no natural connections to air-containing space, and the pressure of gases in the bloodstream is too low for them to be released into the pleural space. Pneumothorax can therefore only develop if air is allowed to enter, either through damage in the chest wall, or damage to the lung itself, or occasionally because microorganism
s in the space produce gas.
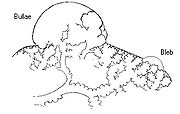
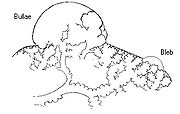
The chest wall defect is usually evident in cases of injury to the chest wall, such as bullet wounds ("open pneumothorax"). In secondary spontaneous pneumothorax, vulnerabilities in the lung tissue
are caused by a variety of disease processes, such as bullae (large air-containing lesions) in emphysema. Areas of necrosis
(tissue death) may precipitate pneumothorax episodes, although the exact mechanism is unclear. Primary spontaneous pneumothorax has for many years been thought to be caused by "blebs", small lesions just under the pleural surface, which were presumed to be more common in those classically at risk of pneumothorax (tall males) due to mechanical factors. Various lines of evidence suggest that this hypothesis may not be correct, such as the fact that pneumothorax may recur even after surgical treatment of blebs, and that blebs occur in 15% of healthy people. It has therefore been suggested that PSP is instead caused by areas of disruption (porosity) in the pleural layer, which are prone to rupture. Smoking may lead to inflammation and obstruction of small airways, accounting for the markedly increased risk of PSP in smokers. Once air has stopped entering the pleural cavity, it is gradually resorbed spontaneously. Estimated rates of resorption are between 1.25% and 2.2% the volume of the cavity per day. This would mean that even a completely collapsed lung would spontaneously reinflate over a period of about 6 weeks.
Tension pneumothorax occurs because the opening that allows air to enter the pleural space functions like a valve, and with every breath more air enters and cannot escape. Severe hypoxia follows, with a resultant drop in blood pressure and level of consciousness. A previously uttered theory that the collapsed lung compresses large blood vessel
s such as the aorta
is probably incorrect.
is usually required. In contrast, tension pneumothorax is ideally treated before imaging, especially if there is severe hypoxia, very low blood pressure, or an impaired level of consciousness; however, X-rays are sometimes required if there is doubt about the location of the pneumothorax.
 Traditionally a plain radiograph of the chest, ideally with the X-ray beams being projected from the back (posteroanterior or PA), has been the most appropriate first investigation. Usually, these are performed in inspiration (holding one's breath); no added information is gathered by obtaining a chest X-ray in expiration (after exhaling). If the PA X-ray does not show a pneumothorax but there is a strong suspicion, lateral X-rays (with beams projecting from the side) may be performed, but this is not routine practice. It is not unusual for the mediastinum
Traditionally a plain radiograph of the chest, ideally with the X-ray beams being projected from the back (posteroanterior or PA), has been the most appropriate first investigation. Usually, these are performed in inspiration (holding one's breath); no added information is gathered by obtaining a chest X-ray in expiration (after exhaling). If the PA X-ray does not show a pneumothorax but there is a strong suspicion, lateral X-rays (with beams projecting from the side) may be performed, but this is not routine practice. It is not unusual for the mediastinum
(the structure between the lungs that contains the heart and several other organs) to be shifted away from the affected lung due to pressure. This is not equivalent to tension pneumothorax, which is determined mainly by symptoms, hypoxia and shock.
The size of the pneumothorax, i.e. the amount of space in the chest taken up by free air rather than air-containing lung, can be determined with a reasonable degree of accuracy by measuring the distance between the chest wall and the lung. This is relevant as smaller pneumothoraces may be treated differently. An air rim of 2 cm or more means that the pneumothorax occupies about 50% of the pleural cavity. British professional guidelines have traditionally stated that the measurement should be performed at the level of the hilum (where blood vessels and airways enter the lung), while American guidelines state that the measurement should happen at the apex (tip) of the lung. The latter method may overestimate the size of a pneumothorax if it is located mainly at the apex, which is a common occurrence. The various methods correlate poorly, but are the best immediately available ways of estimating pneumothorax size. CT scanning (see below) would provide a more accurate determination of the size of the pneumothorax, but its routine use in this setting is not recommended.
Not all pneumothoraces are uniform; some only form a pocket of air in a particular place in the chest. Small amounts of fluid (which may be blood - hemopneumothorax
) may be noted on the chest X-ray. In some cases, the only significant abnormality may be the "deep sulcus sign
", in which the usually small space between the chest wall and the diaphragm
appears enlarged due to the presence of air.
A further use of CT is in the identification of underlying lung lesions. In presumed primary pneumothorax, it may help identify blebs or cystic lesions (in anticipation of treatment, see below), and in secondary pneumothorax it can identify most of the causes listed above.
is used commonly in the evaluation of people who have sustained physical trauma, for example with the FAST protocol
. Ultrasound may be more sensitive than chest X-rays in the identification of pneumothorax after blunt trauma
to the chest.
 The treatment of pneumothorax depends on a number of factors, and may vary from discharge with early follow-up to immediate needle decompression or insertion of a chest tube
The treatment of pneumothorax depends on a number of factors, and may vary from discharge with early follow-up to immediate needle decompression or insertion of a chest tube
. Treatment is determined by the severity of symptoms and indicators of acute illness, the presence of underlying lung disease, the estimated size of the pneumothorax on X-ray, and in some instances also on the personal preference of the person involved. In spontaneous pneumothorax, air travel
is discouraged until it has completely resolved.
In traumatic pneumothorax, chest tubes are usually inserted (unless iatrogenic, see below). It is not yet clear if there is a subgroup of patients with small pneumothoraces who do not require tube treatment and could be managed conservatively. If mechanical ventilation is required, the insertion of a chest tube is mandatory as it would increase the risk of tension pneumothorax.
Tension pneumothorax is usually treated with urgent needle decompression. This may need to happen before transport to hospital, and can be performed by an emergency medical technician
or other trained professional. The needle or cannula
is left in place until a chest tube can be inserted. Any open chest wound is covered, as it carries a high risk of leading to tension pneumothorax, ideally with a dressing called the Asherman seal, which appears to be more effective than standard "three-sided" dressing. The Asherman seal is a specially designed device that adheres to the chest wall and allows air to escape but not to enter the chest through a valve-like mechanism.
Aspiration may also be considered in secondary pneumothorax of moderate size (air rim 1–2 cm) without breathlessness, with the difference that ongoing observation in hospital is required even after a successful procedure. American professional guidelines state that all large pneumothoraces, even those due to PSP, should be treated with a chest tube. Moderately-sized traumatic pneumothorax due to medical procedures (iatrogenic) may initially be treated with aspiration.
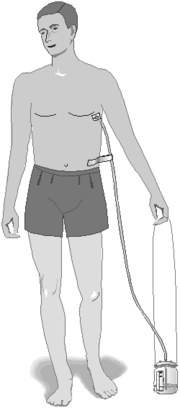
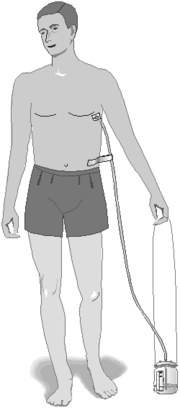
(or intercostal drain) is the most definitive initial treatment of a pneumothorax. This is typically inserted in an area under the axilla (armpit) called the "safe triangle", where damage to internal organs can be avoided; this is delineated by a horizontal line at the level of the nipple and two muscles of the chest wall (latissimus dorsi
and pectoralis major
). Local anesthetic is applied. Two types of tubes may be used. In spontaneous pneumothorax, small-bore (smaller than 14 FG
, 4.7 mm diameter) tubes may be inserted by the Seldinger technique
, and larger tubes do not have an advantage. In traumatic pneumothorax, larger tubes (28 FG, 9.3 mm) are used.
Chest tubes are required in PSP that has not responded to needle aspiration, in any SSP that is large (>50%), and in cases of tension pneumothorax. They are connected to a one-way valve
system that allows air to escape but not to reenter the chest. This may include a bottle with water that functions like a water seal
, or a Heimlich valve
. They are not normally connected to a negative pressure circuit, as this would result in rapid reexpansion of the lung and a risk of pulmonary edema
("reexpansion pulmonary edema"). The tube is left in place until no air is seen to escape from it for a period of time, and X-rays confirm reexpansion of the lung.
If after 2–4 days there is still evidence of air leak, various options are available. Negative pressure suction (at low pressures of –10 to –20 cmH2O
) at a high flow rate may be attempted, especially in PSP; it is thought that this may accelerate the healing of the leak. In SSP, assistance from a thoracic surgeon may be required earlier. Surgical options are similar to those used to prevent further episodes, and are discussed below (thoracotomy and VATS).
, the adherence between the lung and the chest wall. The evidence
on the most effective treatment is still conflicting in some areas, and there is variation between treatments available in Europe and the USA. Not all episodes of pneumothorax require such interventions; the decision depends largely on the suspected risk of recurrence. They however are often recommended after a second pneumothorax. An exception applies in those who engage in diving; diving is considered unsafe unless permanent treatment has been applied; professional guidelines suggest that pleurectomy is performed on both lungs (see below) and that lung function tests
and CT scan must be normal before diving is resumed.
The best results, with a recurrence rate less than 1%, are achieved with a thoracotomy
(surgical opening of the chest) with identification of any clear air leak and stapling of blebs, followed by pleurectomy (stripping of the pleural lining) of the outer pleural layer and pleural abrasion (scraping of the pleura) of the inner layer. During the healing process, the lung adheres to the chest wall, effectively obliterating the pleural space. Thoracotomy is always performed under a general anesthetic.
A less invasive approach is thoracoscopy
, usually in the form of a procedure called video-assisted thoracoscopic surgery
. This also involves a general anesthetic but the lung is approached through a number of small incisions between the ribs. The results from VATS-based pleural abrasion are slightly worse than those achieved by thoracotomy, but with less unsightly skin Scars. VATS may be also be used to achieve chemical pleurodesis; this involves the instillation of talc
, which activates a scarring reaction that may also stick the lung to the chest wall.
Not everyone may be prepared to undergo surgery. If a chest tube is already in place, various agents may be instilled through the tube to achieve pleurodesis, specifically talc and the antibiotic tetracycline. The results from this tend to be worse than from surgical approaches. Talc pleurodesis has few long term consequences in young people.
Death from pneumothorax is very uncommon (except for tension pneumothorax). British statistics have revealed an annual mortality of 1.26 per million per year in men and 0.62 in women. Mortality is higher in older people and those with secondary pneumothorax.
, a student of René Laennec
, first recognised pneumothorax in 1803, and Laennec himself described the full clinical picture in 1819. While Itard and Laennec recognized that some cases were not due to tuberculosis (then the most common cause), the concept of primary spontaneous pneumothorax was reintroduced by the Danish physician Hans Kjærgaard in 1932.
Prior to the advent of anti-tuberculous medications, iatrogenic pneumothoraces were intentionally given to tuberculosis patients in an effort to collapse a lobe, or entire lung around a cavitating lesion. This was known as "resting the lung". It was introduced by the Italian surgeon Carlo Forlanini
in 1888 and publicized by the American surgeon John Benjamin Murphy
in the early 20th century after discovering the same procedure independently. Murphy used the then recently discovered X-ray technology to create pneumothoraces of the correct size.
Pleural cavity
In human anatomy, the pleural cavity is the potential space between the two pleura of the lungs. The pleura is a serous membrane which folds back onto itself to form a two-layered, membrane structure. The thin space between the two pleural layers is known as the pleural cavity; it normally...
of the chest between the lung
Lung
The lung is the essential respiration organ in many air-breathing animals, including most tetrapods, a few fish and a few snails. In mammals and the more complex life forms, the two lungs are located near the backbone on either side of the heart...
and the chest wall. It may occur spontaneously in people without chronic lung conditions ("primary") as well as in those with lung disease ("secondary"), and many pneumothoraces occur after physical trauma
Physical trauma
Trauma refers to "a body wound or shock produced by sudden physical injury, as from violence or accident." It can also be described as "a physical wound or injury, such as a fracture or blow." Major trauma can result in secondary complications such as circulatory shock, respiratory failure and death...
to the chest, blast injury
Blast injury
A blast injury is a complex type of physical trauma resulting from direct or indirect exposure to an explosion. Blast injuries occur with the detonation of high-order explosives as well as the deflagration of low order explosives...
, or as a complication of medical treatment
Iatrogenesis
Iatrogenesis, or an iatrogenic artifact is an inadvertent adverse effect or complication resulting from medical treatment or advice, including that of psychologists, therapists, pharmacists, nurses, physicians and dentists...
.
The symptoms of a pneumothorax are determined by the size of the air leak and the speed by which it occurs; they may include chest pain
Chest pain
Chest pain may be a symptom of a number of serious conditions and is generally considered a medical emergency. Even though it may be determined that the pain is non-cardiac in origin, this is often a diagnosis of exclusion made after ruling out more serious causes of the pain.-Differential...
in most cases and shortness of breath
Dyspnea
Dyspnea , shortness of breath , or air hunger, is the subjective symptom of breathlessness.It is a normal symptom of heavy exertion but becomes pathological if it occurs in unexpected situations...
in many. The diagnosis can be made by physical examination
Physical examination
Physical examination or clinical examination is the process by which a doctor investigates the body of a patient for signs of disease. It generally follows the taking of the medical history — an account of the symptoms as experienced by the patient...
in severe cases but usually requires a chest X-ray
Chest X-ray
In medicine, a chest radiograph, commonly called a chest X-ray , is a projection radiograph of the chest used to diagnose conditions affecting the chest, its contents, and nearby structures...
or computed tomography (CT scan) in milder forms. In a small proportion, the pneumothorax leads to severe oxygen shortage
Hypoxia (medical)
Hypoxia, or hypoxiation, is a pathological condition in which the body as a whole or a region of the body is deprived of adequate oxygen supply. Variations in arterial oxygen concentrations can be part of the normal physiology, for example, during strenuous physical exercise...
and low blood pressure
Hypotension
In physiology and medicine, hypotension is abnormally low blood pressure, especially in the arteries of the systemic circulation. It is best understood as a physiologic state, rather than a disease. It is often associated with shock, though not necessarily indicative of it. Hypotension is the...
, progressing to cardiac arrest
Cardiac arrest
Cardiac arrest, is the cessation of normal circulation of the blood due to failure of the heart to contract effectively...
unless treated; this situation is termed tension pneumothorax.
Small spontaneous pneumothoraces typically resolve by themselves and require no treatment, especially in those with no underlying lung disease. In larger pneumothoraces or when there are severe symptoms, the air may be aspirated with a syringe, or a one-way chest tube
Chest tube
A chest tube is a flexible plastic tube that is inserted through the side of the chest into the pleural space. It is used to remove air or fluid , or pus from the intrathoracic space...
is inserted to allow the air to escape. Occasionally, surgical measures are required, especially if tube drainage is unsuccessful or someone has repeated episodes. Various treatments, usually involving pleurodesis
Pleurodesis
Pleurodesis is a medical procedure in which the pleural space is artificially obliterated. It involves the adhesion of the two pleura.- Uses :Pleurodesis is done to prevent recurrence of pneumothorax or recurrent pleural effusion...
(sticking the lung to the chest wall), may be used if there is a significant risk of repeated episodes of pneumothorax.
Clinical subtypes
Primary spontaneous pneumothorax (PSP), which tends to occur in young people without underlying lung problems, usually causes limited symptoms. Chest pain and sometimes mild breathlessness are the predominant symptoms. Half of those with primary spontaneous pneumothorax wait several days to seek medical attention. It is exceedingly uncommon for PSP to cause tension pneumothorax. The symptoms usually start at rest. Tall males, especially smokersSmoking
Smoking is a practice in which a substance, most commonly tobacco or cannabis, is burned and the smoke is tasted or inhaled. This is primarily practised as a route of administration for recreational drug use, as combustion releases the active substances in drugs such as nicotine and makes them...
, are characteristically at a higher risk of PSP. It has been found that PSP occurs more commonly during changes in atmospheric pressure
Atmospheric pressure
Atmospheric pressure is the force per unit area exerted into a surface by the weight of air above that surface in the atmosphere of Earth . In most circumstances atmospheric pressure is closely approximated by the hydrostatic pressure caused by the weight of air above the measurement point...
and during exposure to loud music, and this explains to an extent why episodes of pneumothorax may happen in clusters.
Secondary spontaneous pneumothorax (SSP) occurs by definition in those with underlying lung diseases. The symptoms tend to be more severe, as the unaffected lung is generally not capable of replacing the loss of function from the affected side. Hypoxemia
Hypoxemia
Hypoxemia is generally defined as decreased partial pressure of oxygen in blood, sometimes specifically as less than or causing hemoglobin oxygen saturation of less than 90%.-Distinction from anemia and hypoxia:...
(decreased blood oxygen levels) is usually present and may be observed as cyanosis
Cyanosis
Cyanosis is the appearance of a blue or purple coloration of the skin or mucous membranes due to the tissues near the skin surface being low on oxygen. The onset of cyanosis is 2.5 g/dL of deoxyhemoglobin. The bluish color is more readily apparent in those with high hemoglobin counts than it is...
(blue discoloration of the lips and skin). Hypercapnia
Hypercapnia
Hypercapnia or hypercapnea , also known as hypercarbia, is a condition where there is too much carbon dioxide in the blood...
(accumulation of carbon dioxide in the blood) is sometimes encountered; this may cause confusion
Mental confusion
Confusion of a pathological degree usually refers to loss of orientation sometimes accompanied by disordered consciousness and often memory Confusion (from Latin confusĭo, -ōnis, noun of action from confundere "to pour together", also "to confuse") of a pathological degree usually refers to loss...
and coma
Coma
In medicine, a coma is a state of unconsciousness, lasting more than 6 hours in which a person cannot be awakened, fails to respond normally to painful stimuli, light or sound, lacks a normal sleep-wake cycle and does not initiate voluntary actions. A person in a state of coma is described as...
. Sudden breathlessness in someone with lung problems such as chronic obstructive pulmonary disease
Chronic obstructive pulmonary disease
Chronic obstructive pulmonary disease , also known as chronic obstructive lung disease , chronic obstructive airway disease , chronic airflow limitation and chronic obstructive respiratory disease , is the co-occurrence of chronic bronchitis and emphysema, a pair of commonly co-existing diseases...
and cystic fibrosis
Cystic fibrosis
Cystic fibrosis is a recessive genetic disease affecting most critically the lungs, and also the pancreas, liver, and intestine...
may therefore prompt investigations for a possible pneumothorax. The size of the pneumothorax bears limited relationship to the symptoms experienced.
Traumatic pneumothorax occurs either because a hole in the chest wall, such as a stab wound
Stabbing
A stabbing is penetration with a sharp or pointed object at close range. Stab connotes purposeful action, as by an assassin or murderer, but it is also possible to accidentally stab oneself or others.Stabbing differs from slashing or cutting in that the motion of the object used in a stabbing...
or gunshot wound
Ballistic trauma
The term ballistic trauma refers to a form of physical trauma sustained from the discharge of arms or munitions. The most common forms of ballistic trauma stem from firearms used in armed conflicts, civilian sporting and recreational pursuits, and criminal activity.-Destructive effects:The degree...
, allows air to enter the pleural space, or because of injury to the lung. It has been found to occur in half of all cases of injury to the chest, coming second after rib fracture
Rib fracture
A rib fracture is a break or fracture in one or more of the bones making up the rib cage.The first rib is rarely fractured because of its protected position behind the clavicle . However, if it is broken serious damage can occur to the brachial plexus of nerves and the subclavian vessels...
in the complications after chest trauma. The pneumothorax can be small (occult) in half of these cases, but they may enlarge if the person requires mechanical ventilation
Mechanical ventilation
In medicine, mechanical ventilation is a method to mechanically assist or replace spontaneous breathing. This may involve a machine called a ventilator or the breathing may be assisted by a physician, respiratory therapist or other suitable person compressing a bag or set of bellows...
and their presence is therefore still relevant. It is also often encountered in those already receiving mechanical ventilation.
Tension pneumothorax is defined differently by different sources, but is generally said to exist when there is severe hypoxia despite administration of oxygen, falling blood pressure
Blood pressure
Blood pressure is the pressure exerted by circulating blood upon the walls of blood vessels, and is one of the principal vital signs. When used without further specification, "blood pressure" usually refers to the arterial pressure of the systemic circulation. During each heartbeat, BP varies...
or confusion. This is a medical emergency
Medical emergency
A medical emergency is an injury or illness that is acute and poses an immediate risk to a person's life or long term health. These emergencies may require assistance from another person, who should ideally be suitably qualified to do so, although some of these emergencies can be dealt with by the...
and may require immediate treatment without further investigations (see below). Tension pneumothorax may also occur in those receiving mechanical ventilation, in which case it may be difficult to spot as the person is typically sedated; it is often noted because of sudden deterioration.
Physical examination
There may be no abnormalities on physical examination, especially if the pneumothorax is small. The breath sounds as audible by stethoscopeStethoscope
The stethoscope is an acoustic medical device for auscultation, or listening to the internal sounds of an animal body. It is often used to listen to lung and heart sounds. It is also used to listen to intestines and blood flow in arteries and veins...
may be diminished on the affected side, as air in the pleural space dampens sound. Percussion
Percussion (medicine)
Percussion is a method of tapping on a surface to determine the underlying structure, and is used in clinical examinations to assess the condition of the thorax or abdomen. It is one of the four methods of clinical examination, together with inspection, palpation and auscultation...
of the chest may sound hyperresonant (higher pitched), and vocal resonance
Vocal resonation
Vocal resonation is the process by which the basic product of phonation is enhanced in timbre and/or intensity by the air-filled cavities through which it passes on its way to the outside air...
and tactile fremitus
Fremitus
Fremitus is a palpable vibration on the human body. In common medical usage, it usually refers to vocal fremitus, although there are several other types.-Pleural fremitus:...
(both examining the conduction of voice by the lung) can be decreased.
Tension pneumothorax is characterized by rapid breathing
Tachypnea
Tachypnea means rapid breathing. Any rate between 12-20 breaths per minute is normal. Tachypnea is a respiration rate greater than 20 breaths per minute. - Distinction from other breathing terms :...
, cyanosis, falling blood pressure
Blood pressure
Blood pressure is the pressure exerted by circulating blood upon the walls of blood vessels, and is one of the principal vital signs. When used without further specification, "blood pressure" usually refers to the arterial pressure of the systemic circulation. During each heartbeat, BP varies...
(hypotension) and confusion. The affected side of the chest may be hyperexpanded and show decreased movement, with increased movement on the other side. In very severe cases, the respiratory rate falls sharply, with shock and coma
Coma
In medicine, a coma is a state of unconsciousness, lasting more than 6 hours in which a person cannot be awakened, fails to respond normally to painful stimuli, light or sound, lacks a normal sleep-wake cycle and does not initiate voluntary actions. A person in a state of coma is described as...
. Recent studies have shown that the development of tension features may not always be as rapid as previously thought. Particular clinical signs may also be less useful in the recognition of tension pneumothorax, such as the deviation of the trachea
Vertebrate trachea
In tetrapod anatomy the trachea, or windpipe, is a tube that connects the pharynx or larynx to the lungs, allowing the passage of air. It is lined with pseudostratified ciliated columnar epithelium cells with goblet cells that produce mucus...
(windpipe) to one side and the presence of raised jugular venous pressure
Jugular venous pressure
The jugular venous pressure is the indirectly observed pressure over the venous system...
(distended neck veins).
Cause
Spontaneous
Spontaneous pneumothoraces are divided into two types: primary, which occurs in the absence of known lung disease, and secondary, which occurs in someone with underlying lung disease. The exact cause of primary spontaneous pneumothorax is unknown, but established risk factors include male sex, smokingSmoking
Smoking is a practice in which a substance, most commonly tobacco or cannabis, is burned and the smoke is tasted or inhaled. This is primarily practised as a route of administration for recreational drug use, as combustion releases the active substances in drugs such as nicotine and makes them...
, and a family history
Family history (medicine)
In medicine, a family history consists of information about disorders from which the direct blood relatives of the patient have suffered. Genealogy typically includes very little of the medical history of the family, but the medical history could be considered a specific subset of the total history...
of pneumothorax. The various suspected underlying mechanisms are discussed below.
Secondary spontaneous pneumothorax occurs in the setting of a variety of lung diseases. The most common is chronic obstructive pulmonary disease
Chronic obstructive pulmonary disease
Chronic obstructive pulmonary disease , also known as chronic obstructive lung disease , chronic obstructive airway disease , chronic airflow limitation and chronic obstructive respiratory disease , is the co-occurrence of chronic bronchitis and emphysema, a pair of commonly co-existing diseases...
which accounts for approximately 70% of cases. Known lung diseases that may increase the risk for pneumothorax are:
- Diseases of the airwayAirwayThe pulmonary airway comprises those parts of the respiratory system through which air flows, conceptually beginning at the nose and mouth, and terminating in the alveoli...
s: chronic obstructive pulmonary diseaseChronic obstructive pulmonary diseaseChronic obstructive pulmonary disease , also known as chronic obstructive lung disease , chronic obstructive airway disease , chronic airflow limitation and chronic obstructive respiratory disease , is the co-occurrence of chronic bronchitis and emphysema, a pair of commonly co-existing diseases...
(especially when emphysemaEmphysemaEmphysema is a long-term, progressive disease of the lungs that primarily causes shortness of breath. In people with emphysema, the tissues necessary to support the physical shape and function of the lungs are destroyed. It is included in a group of diseases called chronic obstructive pulmonary...
and lung bullae are present), acute severe asthmaAsthmaAsthma is the common chronic inflammatory disease of the airways characterized by variable and recurring symptoms, reversible airflow obstruction, and bronchospasm. Symptoms include wheezing, coughing, chest tightness, and shortness of breath...
, cystic fibrosisCystic fibrosisCystic fibrosis is a recessive genetic disease affecting most critically the lungs, and also the pancreas, liver, and intestine... - Lung infections: pneumocystis pneumoniaPneumocystis pneumoniaPneumocystis pneumonia or pneumocystosis is a form of pneumonia, caused by the yeast-like fungus Pneumocystis jirovecii...
(PCP), tuberculosisTuberculosisTuberculosis, MTB, or TB is a common, and in many cases lethal, infectious disease caused by various strains of mycobacteria, usually Mycobacterium tuberculosis. Tuberculosis usually attacks the lungs but can also affect other parts of the body...
, necrotizing pneumoniaPneumoniaPneumonia is an inflammatory condition of the lung—especially affecting the microscopic air sacs —associated with fever, chest symptoms, and a lack of air space on a chest X-ray. Pneumonia is typically caused by an infection but there are a number of other causes... - Interstitial lung diseases: sarcoidosisSarcoidosisSarcoidosis , also called sarcoid, Besnier-Boeck disease or Besnier-Boeck-Schaumann disease, is a disease in which abnormal collections of chronic inflammatory cells form as nodules in multiple organs. The cause of sarcoidosis is unknown...
, idiopathic pulmonary fibrosisIdiopathic pulmonary fibrosisIdiopathic pulmonary fibrosis is a chronic, progressive form of lung disease characterized by fibrosis of the supporting framework of the lungs...
, histiocytosis XLangerhans cell histiocytosisLangerhans cell Histiocytosis is a rare disease involving clonal proliferation of Langerhans cells, abnormal cells deriving from bone marrow and capable of migrating from skin to lymph nodes...
, lymphangioleiomyomatosisLymphangioleiomyomatosisLymphangioleiomyomatosis is a rare lung disease that results in a proliferation of disorderly smooth muscle growth throughout the lungs, in the bronchioles, alveolar septa, perivascular spaces, and lymphatics, resulting in the obstruction of small airways and lymphatics...
(LAM) - Connective tissue diseaseConnective tissue diseaseA connective tissue disease is any disease that has the connective tissues of the body as a target of pathology. Connective tissue is any type of biological tissue with an extensive extracellular matrix that supports, binds together, and protects organs...
s: rheumatoid arthritisRheumatoid arthritisRheumatoid arthritis is a chronic, systemic inflammatory disorder that may affect many tissues and organs, but principally attacks synovial joints. The process produces an inflammatory response of the synovium secondary to hyperplasia of synovial cells, excess synovial fluid, and the development...
, ankylosing spondylitisAnkylosing spondylitisAnkylosing spondylitis , previously known as Bekhterev's disease, Bekhterev syndrome, and Marie-Strümpell disease is a chronic inflammatory disease of the axial skeleton with variable involvement of peripheral joints and nonarticular structures...
, polymyositisPolymyositisPolymyositis is a type of chronic inflammation of the muscles related to dermatomyositis and inclusion body myositis.-Signs and symptoms:...
and dermatomyositisDermatomyositisDermatomyositis is a connective-tissue disease related to polymyositis and Bramaticosis that is characterized by inflammation of the muscles and the skin.- Causes :...
, systemic sclerosis, Marfan's syndrome and Ehlers-Danlos syndromeEhlers-Danlos syndromeEhlers–Danlos syndrome is a group of inherited connective tissue disorders, caused by a defect in the synthesis of collagen . The collagen in connective tissue helps tissues to resist deformation... - CancerCancerCancer , known medically as a malignant neoplasm, is a large group of different diseases, all involving unregulated cell growth. In cancer, cells divide and grow uncontrollably, forming malignant tumors, and invade nearby parts of the body. The cancer may also spread to more distant parts of the...
: lung cancerLung cancerLung cancer is a disease characterized by uncontrolled cell growth in tissues of the lung. If left untreated, this growth can spread beyond the lung in a process called metastasis into nearby tissue and, eventually, into other parts of the body. Most cancers that start in lung, known as primary...
, sarcomaSarcomaA sarcoma is a cancer that arises from transformed cells in one of a number of tissues that develop from embryonic mesoderm. Thus, sarcomas include tumors of bone, cartilage, fat, muscle, vascular, and hematopoietic tissues...
s involving the lung - Catamenial (occurring in relation to the menstrual cycleMenstrual cycleThe menstrual cycle is the scientific term for the physiological changes that can occur in fertile women for the purpose of sexual reproduction. This article focuses on the human menstrual cycle....
): endometriosisEndometriosisEndometriosis is a gynecological medical condition in which cells from the lining of the uterus appear and flourish outside the uterine cavity, most commonly on the ovaries. The uterine cavity is lined by endometrial cells, which are under the influence of female hormones...
in the chest
In children, additional causes include measles
Measles
Measles, also known as rubeola or morbilli, is an infection of the respiratory system caused by a virus, specifically a paramyxovirus of the genus Morbillivirus. Morbilliviruses, like other paramyxoviruses, are enveloped, single-stranded, negative-sense RNA viruses...
, echinococcosis
Echinococcosis
Echinococcosis, which is often referred to as hydatid disease or echinococcal disease, is a parasitic disease that affects both humans and other mammals, such as sheep, dogs, rodents and horses. There are three different forms of echinococcosis found in humans, each of which is caused by the larval...
, inhalation of a foreign body
Foreign body
A foreign body is any object originating outside the body. In machinery, it can mean any unwanted intruding object.Most references to foreign bodies involve propulsion through natural orifices into hollow organs....
, and particular congenital malformations (congenital cystic adenomatoid malformation
Congenital cystic adenomatoid malformation
Congenital cystic adenomatoid malformation is a congenital disorder similar to bronchopulmonary sequestration. In CCAM, usually an entire lobe of lung is replaced by a non-working cystic piece of abnormal lung tissue. This abnormal tissue will never function as normal lung tissue.In most cases the...
and congenital lobar emphysema).
A rare genetic disorder, Birt-Hogg-Dubé syndrome
Birt-Hogg-Dubé syndrome
Birt–Hogg–Dubé syndrome is a human genetic disorder that involves susceptibility to renal cancer, renal and pulmonary cysts, and noncancerous tumors of the hair follicles. The disorder has been reported in more than 100 families worldwide, and it is inherited in an autosomal dominant pattern...
, may cause spontaneous pneumothorax in families. It also causes skin lesions (fibrofolliculoma
Fibrofolliculoma
Fibrofolliculomas are 2 to 4mm in diameter, dome-shaped, yellowish or skin-colored papules usually located on the head, neck, and upper trunk. They are characteristically seen in Birt–Hogg–Dubé syndrome....
s) and lung cysts, and carries an increased risk of kidney cancer. The lung cysts, which probably lead to increased risk of pneumothorax, tend to be in the lower lobes rather than the more common upper lobe cysts encountered in other conditions. Birt-Hogg-Dubé syndrome is caused by mutations in the FLCN gene (chromosome 17p11.2), which encodes a protein named folliculin
Folliculin
Folliculin also known as FLCN, BHD, FLCL, FLCN_HUMAN, MGC17998, or MGC23445 is a tumor-suppressor protein associated with Birt-Hogg-Dubé syndrome...
. FLCN mutations and lung lesions have also been identified in familial cases of pneumothorax where other features of Birt-Hogg-Dubé syndrome are absent.
Traumatic
A traumatic pneumothorax may result from both blunt traumaBlunt trauma
In medical terminology, blunt trauma, blunt injury, non-penetrating trauma or blunt force trauma refers to a type of physical trauma caused to a body part, either by impact, injury or physical attack; the latter usually being referred to as blunt force trauma...
and penetrating injuries
Penetrating trauma
Penetrating trauma is an injury that occurs when an object pierces the skin and enters a tissue of the body, creating an open wound. In blunt, or non-penetrating trauma, there may be an impact, but the skin is not necessarily broken. The penetrating object may remain in the tissues, come back out...
to the chest wall. It may be observed in those exposed to an explosive blast
Blast injury
A blast injury is a complex type of physical trauma resulting from direct or indirect exposure to an explosion. Blast injuries occur with the detonation of high-order explosives as well as the deflagration of low order explosives...
, even if no direct injury to the chest has occurred. The most common mechanism is a cut to the pleura by a fractured rib
Rib fracture
A rib fracture is a break or fracture in one or more of the bones making up the rib cage.The first rib is rarely fractured because of its protected position behind the clavicle . However, if it is broken serious damage can occur to the brachial plexus of nerves and the subclavian vessels...
.
Medical procedures of the chest (iatrogenic
Iatrogenesis
Iatrogenesis, or an iatrogenic artifact is an inadvertent adverse effect or complication resulting from medical treatment or advice, including that of psychologists, therapists, pharmacists, nurses, physicians and dentists...
), such as the taking of biopsy
Biopsy
A biopsy is a medical test involving sampling of cells or tissues for examination. It is the medical removal of tissue from a living subject to determine the presence or extent of a disease. The tissue is generally examined under a microscope by a pathologist, and can also be analyzed chemically...
samples from lung tissue, inserting a central venous catheter
Central venous catheter
In medicine, a central venous catheter is a catheter placed into a large vein in the neck , chest or groin...
into one of the chest veins, may lead to injury to the lung and resultant pneumothorax. The administration of positive pressure ventilation, either mechanical ventilation
Mechanical ventilation
In medicine, mechanical ventilation is a method to mechanically assist or replace spontaneous breathing. This may involve a machine called a ventilator or the breathing may be assisted by a physician, respiratory therapist or other suitable person compressing a bag or set of bellows...
or non-invasive ventilation, may result in barotrauma
Barotrauma
Barotrauma is physical damage to body tissues caused by a difference in pressure between an air space inside or beside the body and the surrounding fluid...
(pressure-related injury) leading to a pneumothorax.
Mechanism

Thoracic cavity
The thoracic cavity is the chamber of the human body that is protected by the thoracic wall ....
is the hollow space that contains the lungs. The lungs are physically connected at the hila
Hilum of lung
Above and behind the cardiac impression is a triangular depression named the hilum, where the structures which form the root of the lung enter and leave the viscus. These include the pulmonary artery, superiormost on the left lung, the superior and inferior pulmonary veins, lymphatic vessels and...
, where the airways and blood vessels enter the lung. They remain inflated inside the thoracic cavity because the pressure inside the pleural space (the space between the chest wall and the lung) is almost consistently negative throughout the respiratory cycle
Breathing
Breathing is the process that moves air in and out of the lungs. Aerobic organisms require oxygen to release energy via respiration, in the form of the metabolism of energy-rich molecules such as glucose. Breathing is only one process that delivers oxygen to where it is needed in the body and...
, effectively sucking the lung to the chest wall. Both the lung and the chest wall are covered by a layer of cells known as the pleura (visceral and parietal pleura, respectively), and a small amount of serous fluid is typically present. The negative pressure normally does not allow air to enter the pleural space because there are no natural connections to air-containing space, and the pressure of gases in the bloodstream is too low for them to be released into the pleural space. Pneumothorax can therefore only develop if air is allowed to enter, either through damage in the chest wall, or damage to the lung itself, or occasionally because microorganism
Microorganism
A microorganism or microbe is a microscopic organism that comprises either a single cell , cell clusters, or no cell at all...
s in the space produce gas.
The chest wall defect is usually evident in cases of injury to the chest wall, such as bullet wounds ("open pneumothorax"). In secondary spontaneous pneumothorax, vulnerabilities in the lung tissue
Parenchyma
Parenchyma is a term used to describe a bulk of a substance. It is used in different ways in animals and in plants.The term is New Latin, f. Greek παρέγχυμα - parenkhuma, "visceral flesh", f. παρεγχεῖν - parenkhein, "to pour in" f. para-, "beside" + en-, "in" + khein, "to pour"...
are caused by a variety of disease processes, such as bullae (large air-containing lesions) in emphysema. Areas of necrosis
Necrosis
Necrosis is the premature death of cells in living tissue. Necrosis is caused by factors external to the cell or tissue, such as infection, toxins, or trauma. This is in contrast to apoptosis, which is a naturally occurring cause of cellular death...
(tissue death) may precipitate pneumothorax episodes, although the exact mechanism is unclear. Primary spontaneous pneumothorax has for many years been thought to be caused by "blebs", small lesions just under the pleural surface, which were presumed to be more common in those classically at risk of pneumothorax (tall males) due to mechanical factors. Various lines of evidence suggest that this hypothesis may not be correct, such as the fact that pneumothorax may recur even after surgical treatment of blebs, and that blebs occur in 15% of healthy people. It has therefore been suggested that PSP is instead caused by areas of disruption (porosity) in the pleural layer, which are prone to rupture. Smoking may lead to inflammation and obstruction of small airways, accounting for the markedly increased risk of PSP in smokers. Once air has stopped entering the pleural cavity, it is gradually resorbed spontaneously. Estimated rates of resorption are between 1.25% and 2.2% the volume of the cavity per day. This would mean that even a completely collapsed lung would spontaneously reinflate over a period of about 6 weeks.
Tension pneumothorax occurs because the opening that allows air to enter the pleural space functions like a valve, and with every breath more air enters and cannot escape. Severe hypoxia follows, with a resultant drop in blood pressure and level of consciousness. A previously uttered theory that the collapsed lung compresses large blood vessel
Blood vessel
The blood vessels are the part of the circulatory system that transports blood throughout the body. There are three major types of blood vessels: the arteries, which carry the blood away from the heart; the capillaries, which enable the actual exchange of water and chemicals between the blood and...
s such as the aorta
Aorta
The aorta is the largest artery in the body, originating from the left ventricle of the heart and extending down to the abdomen, where it branches off into two smaller arteries...
is probably incorrect.
Diagnosis
The symptoms of pneumothorax can be subtle, especially in those with PSP, and confirmation with medical imagingMedical imaging
Medical imaging is the technique and process used to create images of the human body for clinical purposes or medical science...
is usually required. In contrast, tension pneumothorax is ideally treated before imaging, especially if there is severe hypoxia, very low blood pressure, or an impaired level of consciousness; however, X-rays are sometimes required if there is doubt about the location of the pneumothorax.
Chest X-ray

Mediastinum
The mediastinum is a non-delineated group of structures in the thorax, surrounded by loose connective tissue. It is the central compartment of the thoracic cavity...
(the structure between the lungs that contains the heart and several other organs) to be shifted away from the affected lung due to pressure. This is not equivalent to tension pneumothorax, which is determined mainly by symptoms, hypoxia and shock.
The size of the pneumothorax, i.e. the amount of space in the chest taken up by free air rather than air-containing lung, can be determined with a reasonable degree of accuracy by measuring the distance between the chest wall and the lung. This is relevant as smaller pneumothoraces may be treated differently. An air rim of 2 cm or more means that the pneumothorax occupies about 50% of the pleural cavity. British professional guidelines have traditionally stated that the measurement should be performed at the level of the hilum (where blood vessels and airways enter the lung), while American guidelines state that the measurement should happen at the apex (tip) of the lung. The latter method may overestimate the size of a pneumothorax if it is located mainly at the apex, which is a common occurrence. The various methods correlate poorly, but are the best immediately available ways of estimating pneumothorax size. CT scanning (see below) would provide a more accurate determination of the size of the pneumothorax, but its routine use in this setting is not recommended.
Not all pneumothoraces are uniform; some only form a pocket of air in a particular place in the chest. Small amounts of fluid (which may be blood - hemopneumothorax
Hemopneumothorax
Hemopneumothorax, or haemopneumothorax, is a medical term describing the combination of two conditions: pneumothorax, or air in the chest cavity, and hemothorax , or blood in the chest cavity....
) may be noted on the chest X-ray. In some cases, the only significant abnormality may be the "deep sulcus sign
Deep sulcus sign
In radiology, the deep sulcus sign on a supine chest radiograph is an indication of a pneumothorax. In a supine film , it may be the only indication of a pneumothorax because air collects anteriorly and basally, within the nondependent portions of the pleural space as opposed to the apex when the...
", in which the usually small space between the chest wall and the diaphragm
Thoracic diaphragm
In the anatomy of mammals, the thoracic diaphragm, or simply the diaphragm , is a sheet of internal skeletal muscle that extends across the bottom of the rib cage. The diaphragm separates the thoracic cavity from the abdominal cavity and performs an important function in respiration...
appears enlarged due to the presence of air.
Computed tomography
Computed tomography (CT or CAT scan) can be useful in particular situations. In some lung diseases, especially emphysema, it is possible for abnormal lung areas such as bullae (large air-filled sacs) to have the same appearance as a pneumothorax, and it may not be safe to apply any treatment before the distinction is made and before the exact location and size of the pneumothorax is determined. In trauma, where it may not be possible to perform an upright film, chest radiography may miss up to a third of pneumothoraces, while CT remains very sensitive.A further use of CT is in the identification of underlying lung lesions. In presumed primary pneumothorax, it may help identify blebs or cystic lesions (in anticipation of treatment, see below), and in secondary pneumothorax it can identify most of the causes listed above.
Ultrasound
UltrasoundMedical ultrasonography
Diagnostic sonography is an ultrasound-based diagnostic imaging technique used for visualizing subcutaneous body structures including tendons, muscles, joints, vessels and internal organs for possible pathology or lesions...
is used commonly in the evaluation of people who have sustained physical trauma, for example with the FAST protocol
Focused assessment with sonography for trauma
Focused Assessment with Sonography for Trauma is a rapid bedside ultrasound examination performed by surgeons and emergency physicians as a screening test for blood around the heart or abdominal organs after trauma.The four areas that are examined for free fluid are the perihepatic space...
. Ultrasound may be more sensitive than chest X-rays in the identification of pneumothorax after blunt trauma
Blunt trauma
In medical terminology, blunt trauma, blunt injury, non-penetrating trauma or blunt force trauma refers to a type of physical trauma caused to a body part, either by impact, injury or physical attack; the latter usually being referred to as blunt force trauma...
to the chest.
Treatment
Chest tube
A chest tube is a flexible plastic tube that is inserted through the side of the chest into the pleural space. It is used to remove air or fluid , or pus from the intrathoracic space...
. Treatment is determined by the severity of symptoms and indicators of acute illness, the presence of underlying lung disease, the estimated size of the pneumothorax on X-ray, and in some instances also on the personal preference of the person involved. In spontaneous pneumothorax, air travel
Air travel
Air travel is a form of travel in vehicles such as airplanes, helicopters, hot air balloons, blimps, gliders, hang gliding, parachuting or anything else that can sustain flight.-Domestic and international flights:...
is discouraged until it has completely resolved.
In traumatic pneumothorax, chest tubes are usually inserted (unless iatrogenic, see below). It is not yet clear if there is a subgroup of patients with small pneumothoraces who do not require tube treatment and could be managed conservatively. If mechanical ventilation is required, the insertion of a chest tube is mandatory as it would increase the risk of tension pneumothorax.
Tension pneumothorax is usually treated with urgent needle decompression. This may need to happen before transport to hospital, and can be performed by an emergency medical technician
Emergency medical technician
Emergency Medical Technician or Ambulance Technician are terms used in some countries to denote a healthcare provider of emergency medical services...
or other trained professional. The needle or cannula
Cannula
A cannula or canula is a tube that can be inserted into the body, often for the delivery or removal of fluid or for the gathering of data...
is left in place until a chest tube can be inserted. Any open chest wound is covered, as it carries a high risk of leading to tension pneumothorax, ideally with a dressing called the Asherman seal, which appears to be more effective than standard "three-sided" dressing. The Asherman seal is a specially designed device that adheres to the chest wall and allows air to escape but not to enter the chest through a valve-like mechanism.
Conservative
Small spontaneous pneumothoraces do not always require treatment, as they are unlikely to proceed to respiratory failure or tension pneumothorax and generally resolve spontaneously. This approach is most appropriate if the estimated size of the pneumothorax is small (e.g. <50%), there is no breathlessness, and there is no underlying lung disease. It may be appropriate to treat a larger PSP conservatively if the symptoms are limited. Admission to hospital is often not required, as long as clear instructions are given to return to hospital if there are worsening symptoms. Further investigations may be performed as an outpatient, at which time X-rays are repeated to confirm improvement, and advice may be given with regards to preventing recurrence such as surgery (see below). Secondary pneumothoraces are only treated conservatively if the size is very small (1 cm or less air rim) and there are limited symptoms. Admission to hospital is usually recommended. Oxygen given at a high flow rate may accelerate resorption.Aspiration
In a large primary spontaneous pneumothorax (>50%) or PSP associated with breathlessness, some professional guidelines recommend that reducing the size by aspiration is equally effective as insertion of a chest tube. This involves the administration of local anesthetic and inserting a needle connected to a three-way tap; up to 2.5 liters of air (in adults) are removed. If there has been significant reduction in the size of the pneumothorax on a further X-ray, the remainder of the treatment can be conservative. This approach is effective in over 50% of cases. First-line aspiration in PSP reduces the number of people requiring admission to hospital significantly as opposed to tube drainage, without increasing the risk of complications.Aspiration may also be considered in secondary pneumothorax of moderate size (air rim 1–2 cm) without breathlessness, with the difference that ongoing observation in hospital is required even after a successful procedure. American professional guidelines state that all large pneumothoraces, even those due to PSP, should be treated with a chest tube. Moderately-sized traumatic pneumothorax due to medical procedures (iatrogenic) may initially be treated with aspiration.
Chest tube
A chest tubeChest tube
A chest tube is a flexible plastic tube that is inserted through the side of the chest into the pleural space. It is used to remove air or fluid , or pus from the intrathoracic space...
(or intercostal drain) is the most definitive initial treatment of a pneumothorax. This is typically inserted in an area under the axilla (armpit) called the "safe triangle", where damage to internal organs can be avoided; this is delineated by a horizontal line at the level of the nipple and two muscles of the chest wall (latissimus dorsi
Latissimus dorsi muscle
The latissimus dorsi , meaning 'broadest muscle of the back' , is the larger, flat, dorso-lateral muscle on the trunk, posterior to the arm, and partly covered by the trapezius on its median dorsal region.The latissimus dorsi is responsible for extension,...
and pectoralis major
Pectoralis major muscle
The pectoralis major is a thick, fan-shaped muscle, situated at the chest of the body. It makes up the bulk of the chest muscles in the male and lies under the breast in the female...
). Local anesthetic is applied. Two types of tubes may be used. In spontaneous pneumothorax, small-bore (smaller than 14 FG
French catheter scale
The French scale or French gauge system is commonly used to measure the size of a catheter. It is most often abbreviated as Fr, but can often abbreviated as FR or F. It may also be abbreviated as CH or Ch in French speaking countries...
, 4.7 mm diameter) tubes may be inserted by the Seldinger technique
Seldinger technique
The Seldinger technique is a medical procedure to obtain safe access to blood vessels and other hollow organs. It is named after Dr. Sven-Ivar Seldinger , a Swedish radiologist from Mora, Dalarna County, who introduced the procedure in 1953....
, and larger tubes do not have an advantage. In traumatic pneumothorax, larger tubes (28 FG, 9.3 mm) are used.
Chest tubes are required in PSP that has not responded to needle aspiration, in any SSP that is large (>50%), and in cases of tension pneumothorax. They are connected to a one-way valve
Check valve
A check valve, clack valve, non-return valve or one-way valve is a mechanical device, a valve, which normally allows fluid to flow through it in only one direction....
system that allows air to escape but not to reenter the chest. This may include a bottle with water that functions like a water seal
Trap (plumbing)
In plumbing, a trap is a U-, S-, or J-shaped pipe located below or within a plumbing fixture. An S-shaped trap is also known as the S-bend invented by Alexander Cummings in 1775 but became known as the U-bend following the introduction of the U-shaped trap by Thomas Crapper in 1880. The new U-bend...
, or a Heimlich valve
Flutter valve
A flutter valve is a one-way valve used in respiratory medicine to prevent air from travelling back along a chest tube. It is most commonly used to help remove air from a pneumothorax...
. They are not normally connected to a negative pressure circuit, as this would result in rapid reexpansion of the lung and a risk of pulmonary edema
Pulmonary edema
Pulmonary edema , or oedema , is fluid accumulation in the air spaces and parenchyma of the lungs. It leads to impaired gas exchange and may cause respiratory failure...
("reexpansion pulmonary edema"). The tube is left in place until no air is seen to escape from it for a period of time, and X-rays confirm reexpansion of the lung.
If after 2–4 days there is still evidence of air leak, various options are available. Negative pressure suction (at low pressures of –10 to –20 cmH2O
Centimetre of water
A centimetre of water is a less commonly used unit of pressure derived from pressure head calculations using metrology...
) at a high flow rate may be attempted, especially in PSP; it is thought that this may accelerate the healing of the leak. In SSP, assistance from a thoracic surgeon may be required earlier. Surgical options are similar to those used to prevent further episodes, and are discussed below (thoracotomy and VATS).
Prevention
Both medical and surgical treatments exist to reduce the risk of recurrence of a pneumothorax. The main aim is to achieve pleurodesisPleurodesis
Pleurodesis is a medical procedure in which the pleural space is artificially obliterated. It involves the adhesion of the two pleura.- Uses :Pleurodesis is done to prevent recurrence of pneumothorax or recurrent pleural effusion...
, the adherence between the lung and the chest wall. The evidence
Evidence-based medicine
Evidence-based medicine or evidence-based practice aims to apply the best available evidence gained from the scientific method to clinical decision making. It seeks to assess the strength of evidence of the risks and benefits of treatments and diagnostic tests...
on the most effective treatment is still conflicting in some areas, and there is variation between treatments available in Europe and the USA. Not all episodes of pneumothorax require such interventions; the decision depends largely on the suspected risk of recurrence. They however are often recommended after a second pneumothorax. An exception applies in those who engage in diving; diving is considered unsafe unless permanent treatment has been applied; professional guidelines suggest that pleurectomy is performed on both lungs (see below) and that lung function tests
Spirometry
Spirometry is the most common of the pulmonary function tests , measuring lung function, specifically the measurement of the amount and/or speed of air that can be inhaled and exhaled...
and CT scan must be normal before diving is resumed.
The best results, with a recurrence rate less than 1%, are achieved with a thoracotomy
Thoracotomy
Thoracotomy is an incision into the pleural space of the chest. It is performed by a surgeon, and, rarely, by emergency physicians, to gain access to the thoracic organs, most commonly the heart, the lungs, the esophagus or thoracic aorta, or for access to the anterior spine such as is necessary...
(surgical opening of the chest) with identification of any clear air leak and stapling of blebs, followed by pleurectomy (stripping of the pleural lining) of the outer pleural layer and pleural abrasion (scraping of the pleura) of the inner layer. During the healing process, the lung adheres to the chest wall, effectively obliterating the pleural space. Thoracotomy is always performed under a general anesthetic.
A less invasive approach is thoracoscopy
Thoracoscopy
Thoracoscopy is a medical procedure involving internal examination, biopsy, and/or resection of disease or masses within the pleural cavity and thoracic cavity...
, usually in the form of a procedure called video-assisted thoracoscopic surgery
Video-assisted thoracoscopic surgery
Video-assisted thoracoscopic surgery is a type of thoracic surgery performed using a small video camera that is introduced into the patient's chest via a scope. The surgeon is able to view the instruments that are being used along with the anatomy on which the surgeon is operating...
. This also involves a general anesthetic but the lung is approached through a number of small incisions between the ribs. The results from VATS-based pleural abrasion are slightly worse than those achieved by thoracotomy, but with less unsightly skin Scars. VATS may be also be used to achieve chemical pleurodesis; this involves the instillation of talc
Talc
Talc is a mineral composed of hydrated magnesium silicate with the chemical formula H2Mg34 or Mg3Si4O102. In loose form, it is the widely-used substance known as talcum powder. It occurs as foliated to fibrous masses, its crystals being so rare as to be almost unknown...
, which activates a scarring reaction that may also stick the lung to the chest wall.
Not everyone may be prepared to undergo surgery. If a chest tube is already in place, various agents may be instilled through the tube to achieve pleurodesis, specifically talc and the antibiotic tetracycline. The results from this tend to be worse than from surgical approaches. Talc pleurodesis has few long term consequences in young people.
Epidemiology
Spontaneous pneumothorax is more common in males than in females. The annual incidence of PSP is 18–28 per 100,000 in males and 1.2–6.0 in females. Secondary spontaneous pneumothorax is less common, with 6.3 for males and 2.0 for females. Risk of recurrence depends on underlying lung disease. Once a second episode has occurred, there is a high likelihood of subsequent further episodes. Smokers have an increased risk of contracting a first spontaneous pneumothorax of approximately ninefold among women and 22-fold among men compared to non-smokers. The incidence in children has not been well studied, but it is probably less than that of adults and often reflects underlying lung disease.Death from pneumothorax is very uncommon (except for tension pneumothorax). British statistics have revealed an annual mortality of 1.26 per million per year in men and 0.62 in women. Mortality is higher in older people and those with secondary pneumothorax.
History
Jean Marc Gaspard ItardJean Marc Gaspard Itard
Jean Marc Gaspard Itard was a French physician born in Provence.Without a university education and working at a bank, he was forced to enter the army during the French Revolution but presented himself as a physician at that time...
, a student of René Laennec
René Laennec
René-Théophile-Hyacinthe Laennec was a French physician. He invented the stethoscope in 1816, while working at the Hôpital Necker and pioneered its use in diagnosing various chest conditions....
, first recognised pneumothorax in 1803, and Laennec himself described the full clinical picture in 1819. While Itard and Laennec recognized that some cases were not due to tuberculosis (then the most common cause), the concept of primary spontaneous pneumothorax was reintroduced by the Danish physician Hans Kjærgaard in 1932.
Prior to the advent of anti-tuberculous medications, iatrogenic pneumothoraces were intentionally given to tuberculosis patients in an effort to collapse a lobe, or entire lung around a cavitating lesion. This was known as "resting the lung". It was introduced by the Italian surgeon Carlo Forlanini
Carlo Forlanini
Carlo Forlanini was an Italian physician.In 1870 he earned his medical degree from the University of Pavia, where he studied as an alumnus of Borromeo College, and afterwards joined the staff of the Ospedale Maggiore in Milan...
in 1888 and publicized by the American surgeon John Benjamin Murphy
John Benjamin Murphy
John Benjamin Murphy, born John Murphy , was an American physician and abdominal surgeon noted for advocating early surgical intervention in appendicitis appendectomy, and several eponyms: Murphy’s button, Murphy drip, Murphy’s punch, Murphy’s test, and Murphy-Lane bone skid...
in the early 20th century after discovering the same procedure independently. Murphy used the then recently discovered X-ray technology to create pneumothoraces of the correct size.

